Dega Acetabuloplasty
Paul D. Sponseller
Jaysson T. Brooks
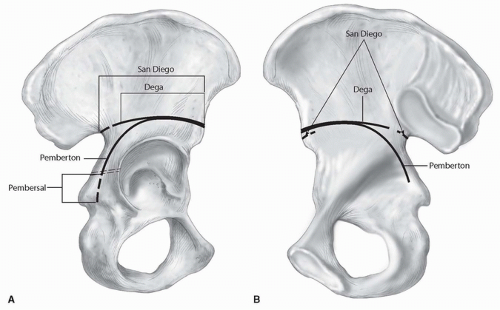
Professor W. Dega, working in Poznan, Poland, described an incomplete iliac osteotomy in 1969. Reported just a few years after Pemberton’s osteotomy, the Dega osteotomy was part of a continuum of incomplete osteotomies that also include the Pembersal and the San Diego osteotomies. These osteotomies correct the acetabulum but maintain hinges on portions of the symphysis pubis and the triradiate cartilage (Fig. 16-1). Because of this second point of hinging, these osteotomies have the potential not only to reorient the acetabulum but also to reshape it. They differ in the extent of the bone cut on the inner and outer tables of the acetabulum—the extent of the remaining hinge. The Pemberton procedure cuts both the inner and the outer tables of the ilium, hinges on the ischial limb of the triradiate cartilage, and extends past the ischial limb of the triradiate cartilage, freeing the acetabulum to rotate more. The San Diego osteotomy preserves the entire medial cortex and cuts through the cortical bone of the sciatic notch in an attempt to produce equal anterior and posterior coverage. The Dega osteotomy preserves the inner table of the pelvis posterior to the iliopectineal line. It also preserves the entire cortex of the sciatic notch, forming a hinge to provide more anterior and lateral femoral head coverage. The exciting aspect, however, about the Dega osteotomy is its versatility in providing femoral head coverage in any direction based on where the ilium is left intact. If the osteotomy is extended through the sciatic notch, instead of stopping short of it, then the medial cortex of the midilium acts as a hinge, which helps to provide more posterior coverage. This modification makes the Dega osteotomy look quite similar to the San Diego osteotomy.
This chapter presents the Dega osteotomy surgical technique, which provides anterior and lateral coverage as classically described by Dega, and discusses its potential modifications.
INDICATIONS
The Dega has been described primarily for use in developmental dysplasia of the hip, a condition in which the posterior portion of the acetabulum is far better developed than is the anterior portion. However, some patients with neuromuscular dysplasia or skeletal dysplasia (such as spondyloepiphyseal dysplasia or Morquio syndrome) may also be candidates for this procedure if the coverage needed is primarily anterolateral. Intraoperatively, if it is observed that a patient with a neuromuscular disorder requires more posterior coverage, the Dega osteotomy can be easily modified by extending the cut into the sciatic notch, as in the San Diego osteotomy. The lower age limit for the osteotomy is primarily determined by bone quality, which must be strong enough (on the younger end) to support the hinge process, yet not too stiff (on the older end) to hinge plastically. For the bone to be adequately plastic, the triradiate cartilage should ideally be open. Therefore, the ideal age range is approximately 2 to 12 years. The Dega also works well for bilateral procedures because the stress on the symphysis pubis is probably less than is that from a complete iliac osteotomy.
CONTRAINDICATIONS
Patients with an acetabulum that is too small to adequately contain the femoral head, even after reorientation, should be treated by another procedure, such as a shelf arthroplasty or Chiari osteotomy. Patients with extreme osteopenia may not tolerate the reorientation without settling of the cut ilium onto the autograft wedge, resulting in a loss of fixation.
PREOPERATIVE PLANNING
The range of hip flexion should be assessed. If flexion is less than 90 degrees before surgery, it may worsen after surgery and may limit the patient’s ability to sit. The rotation and resting position of the hip should also be assessed. The acetabuloplasty tends to produce some apparent external rotation (10 to 20 degrees), which can be compensated for by additional internal rotation of the femur if an osteotomy of this bone is also being performed.
Imaging consists of an anteroposterior radiograph of the pelvis. An abduction-internal rotation anterior-posterior radiograph, taken with the hip in extension, will also give an idea of the degree of potential coverage and possibly the need to perform an open reduction.
Some surgeons like to obtain a preoperative three-dimensional computed tomogram to assess the acetabular abnormality. Others think that this information can be gained intraoperatively by fluoroscopy, inspection, and noting the response of the acetabulum to redirection.
SURGICAL PROCEDURE
The patient is placed supine, with the pelvis on a radiolucent table. Slight elevation of the involved hemipelvis may be produced by placing a “bump” under the iliosacral region. If both sides are to be addressed at one session, a square towel under the sacrum will elevate them both. The fluoroscope should be positioned over the patient from the opposite side.
The incision described by Dega extends from a point inferior to the anterior-superior iliac spine (ASIS) and proceeds posteriorly and inferiorly. Alternatively, the straight “bikini” incision described by Salter can be used in the skin tension lines that run obliquely from posterosuperior to anteroinferior to the ASIS. This incision produces a cosmetically superior result, with no loss in operative exposure. The first structure to identify is the lateral femoral cutaneous nerve, which is underneath the anterior fascia and almost always distal to the ASIS, coursing distally and laterally. Once the lateral femoral cutaneous nerve is identified and freed, it should be retracted medially, making it easier to develop the tensor-sartorius interval up to the ASIS. With a no. 15 blade scalpel, the iliac apophysis is split as far along the iliac crest as possible, allowing exposure for eventual autograft if desired.
In the depths of the tensor-sartorius interval, the ascending branch of the lateral femoral circumflex vessels should be sought and coagulated. The lateral surface of the ilium should be exposed.
Bleeding from bony nutrient foramen should be stopped. Some surgeons also include subperiosteal exposure of the inner table of the ilium to prevent inadvertent harm to structures during cutting of the medial wall with the osteotome. If a capsulorrhaphy is indicated, the tendon of the rectus femoris muscle should be tagged and detached. If the rectus is detached, it can be used to retract and protect the lateral femoral cutaneous nerve. If a capsulorrhaphy is not needed, the tendon may be left intact. The exposure on the medial surface of the ilium should extend at least to the iliopectineal line so that the extent of the osteotomy may be visualized.
Bleeding from bony nutrient foramen should be stopped. Some surgeons also include subperiosteal exposure of the inner table of the ilium to prevent inadvertent harm to structures during cutting of the medial wall with the osteotome. If a capsulorrhaphy is indicated, the tendon of the rectus femoris muscle should be tagged and detached. If the rectus is detached, it can be used to retract and protect the lateral femoral cutaneous nerve. If a capsulorrhaphy is not needed, the tendon may be left intact. The exposure on the medial surface of the ilium should extend at least to the iliopectineal line so that the extent of the osteotomy may be visualized.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree