9
Cervical Syndrome
 Definition and Prevalence
Definition and Prevalence
 Definition: The term “cervical syndrome” refers to all pathological clinical manifestations due to functional disturbances and degenerative changes of the cervical motion segments.
Definition: The term “cervical syndrome” refers to all pathological clinical manifestations due to functional disturbances and degenerative changes of the cervical motion segments.
Cervical syndromes are associated with restricted mobility of the cervical spine, increased tension of the shoulder and neck muscles, and (in some cases) radicular signs in the upper limbs, as well as autonomic manifestations. “Cervical syndrome” is a purely clinical term. The painless partial immobilization of the cervical spine that often occurs in old age because of advanced osteochondrosis and spondylosis is not considered a cervical syndrome.
The involutional changes of old age profoundly affect the morphology of the cervical disks, which lie immediately adjacent to important parts of the central nervous system and the vascular system. Clinical manifestations of several different kinds may result, as will be explained below.
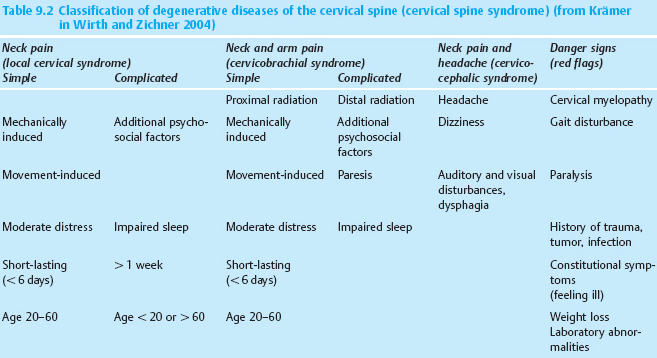
Prevalence; age and sex distribution. Symptoms related to changes in the cervical disks are common. Every fifth patient who visits an orthopedist does so because of a cervical disk syndrome. Women are more commonly affected than men, up to age 60 (Fig. 9.1). The point prevalence of neck pain (i.e., “neck pain today”) in the general population is 30%, and its annual prevalence (i.e., “neck pain within the past year”) is 60%. These figures are only slightly lower than the corresponding ones for back pain (Kohlmann 2001, Borenstein et al. 2004). Similar figures on the prevalence and distribution of cervical spine syndromes were reported by Bovim et al. (1994), Coté et al. (1998), Guez et al. (2002), Borenstein et al. (2004), Fejar et al. (2005), and in the key findings from the Task Force on Neck Pain (Haldeman et al. 2008).
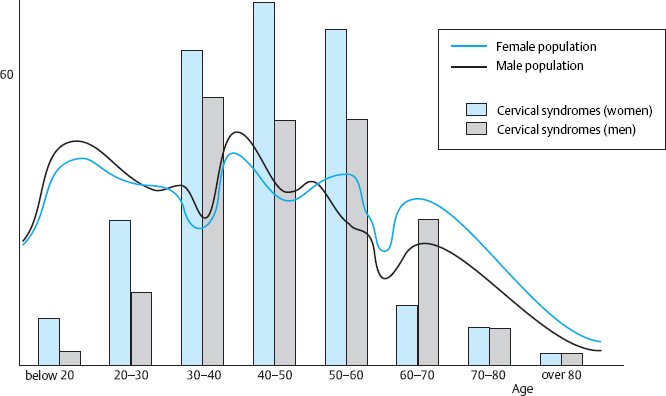
Fig. 9.1 Age distribution of men and women receiving outpatient treatment for cervical syndrome in Düsseldorf and Bochum (North Rhine Westphalia, Germany), compared to the age distribution of men and women in the overall population (population data from the Statistical Yearbook of the State of North Rhine-Westphalia, Germany).
Classification. The cervical syndromes are classified by their cardinal manifestations and duration, and treated accordingly. They are divided into acute and chronic conditions with and without radicular manifestations. The duration of symptoms is correlated with the age of the patient: acute manifestations are more common in younger individuals, while chronic cervical spine conditions are more common in older adults. Traumatic cervical spine syndromes form a class in themselves.
The wide variety of possibilities for the spatial and temporal distribution of pain and other symptoms often makes it impossible to give a more precise and cogent name to a particular instance of a cervical syndrome. The clinical findings are the most important determinant of the treatment to be applied, and the treatment must be continually adapted to the patient’s changing symptoms and to their previous response to the treatments already given. “Polypragmasia,” i.e., a multiple-component treatment strategy, is often the best approach.
 Special Anatomy and Physiology of the Cervical Motion Segments
Special Anatomy and Physiology of the Cervical Motion Segments
Uncinate Processes
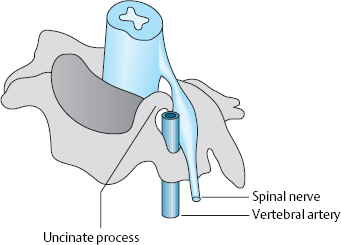
The cervical motion segments differ from those of the rest of the spine in a number of anatomical and biomechanical features that render them more susceptible to early signs of wear and tear, with the consequent development of symptoms. The end plates of vertebral bodies C3–C7 have saddle-like posterior and lateral extensions called the uncinate processes, which in turn give the cervical disks their laterally tapering shape. Furthermore, because of the cervical lordosis, the disks are a third higher ventrally than dorsally. In a frontal anatomical section, the disks look flat and concave upward (Fig. 9.2).
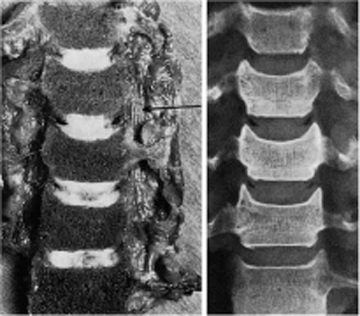
Fig. 9.2 a, b Coronal section through the mid-cervical spine of a 27-year-old man. The arrow indicates the vertebral artery.
a Anatomical specimen.
b Radiograph.
The uncinate processes develop during the growth period of the cervical spine and finally assume the shape of shovel-like crests of bone sticking out from the lateral edges of the vertebrae. Because of the uncinate processes, the cervical disks are mainly bordered by bone laterally, unlike the disks elsewhere in the spine. Our studies of cervical spine biomechanics (Stahl 1977) showed that the uncinate processes are located more laterally on the edge of the vertebrae in the upper segments of the cervical spine and more dorsolaterally in the lower segments, with a transition at C6.
Cervical disk degeneration is accompanied by osteophyte formation from the uncinate processes. These osteophytes are often of clinical importance, as they may lie in the immediate vicinity of the cervical nerve roots or the vertebral artery (Fig. 9.3). Aufdermaur (1968) showed that osteophytes grow dorsolaterally from the uncinate processes between the ages of 30 and 50. As an individual ages, osteophytes tend to form more laterally, i.e., closer to the vertebral artery.
The transition at C6 regarding the lateral vs. dorsolateral position of osteophytes was mentioned above. In consequence, the formation of large osteophytes is more likely to cause vascular compression in the upper and middle cervical segments and neural compression in the lower cervical segments (Faustmann 2004).
Horizontal Fissures
Von Luschka (1858) was the first to describe horizontal fissures in the cervical disks, which he designated as lateral half-joints. These fissures develop in childhood at the level of the uncinate processes and tend to progress in a medial direction. They are so commonly seen that they are considered a normal finding. Horizontal fissures are a sign, not of degeneration, but rather of adaptation of the cervical spine to allow greater mobility (Töndury 1958, Ecklin 1969, Shark and Parke 1983, Faustmann 2004).
Unlike the degenerative radial fissures of the disks elsewhere in the spine, the horizontal fissures of the cervical disks appear in the midst of entirely normal disk tissue. They begin in the outer lamellae of the anulus fibrosus and gradually narrow as they proceed toward the center of the disk. Often, a meniscus-like wedge of tissue grows into the fissure from the neighboring paravertebral connective tissue. According to Ecklin (1960), an anatomical situation arises that is in all respects comparable to a joint: the fissure possesses an enclosed space with smooth borders, layers of hyaline cartilage on the uncinate process and on the opposite pole (von Luschka’s joint facet), a meniscus-like articulation, and, often, tough fibrous bands separating the “joint” from the spinal canal, in the manner of a capsule (Stahl and Huth 1980). In our own anatomical studies, we have found synovium-lined cavities in the uncovertebral region in all decades of life.
 The horizontal fissures increase the mobility of the cervical spine, but they are also a biomechanically vulnerable “site of least resistance” because of their tendency to extend medially and laterally.
The horizontal fissures increase the mobility of the cervical spine, but they are also a biomechanically vulnerable “site of least resistance” because of their tendency to extend medially and laterally.
Vertebral Artery and Cervical Sympathetic Chain
The uncovertebral region lies in the immediate vicinity of both the vertebral artery and the cervical sympathetic chain. The age-associated changes of the uncovertebral region can impinge on either or both of these structures, producing neurovascular manifestations of various kinds. The cervical sympathetic chain, which communicates with the spinal nerves through the rami communicantes, and its three associated ganglia provide autonomic innervation to the head, neck, and upper limbs. The upper ganglion serves segments C1–C4, and the middle ganglion serves C5–C6; the lower ganglion is fused with the uppermost thoracic ganglion to form the stellate ganglion, which serves C7–T2. The stellate ganglion is the most important relay station among these ganglia, because all of the efferent and nearly all of the afferent sympathetic fibers of the head, neck, upper limb, and upper part of the thorax pass through it. From the sympathetic chain ganglia, the sympathetic fibers travel upward by various routes, including along the sympathetic arterial plexus of the vertebral artery.
The studies of Hovelacque (1925), Werte (1934), Kummer (1984), Kehr and Jung (1985), Bogduk et al. (1988), Lang (1991), Faustmann (2004), and Heller et al. (2005) demonstrate the interconnections of the cervical sympathetic innervation with the cervical spinal nerves and the sympathetic arterial plexus of the vertebral artery. Sympathetic fibers from all three cervical ganglia pass from the sympathetic chain to spinal nerves C4–C8 and partially encircle the vertebral artery.
The vertebral artery originates from the subclavian artery and passes upward through the foramina of the transverse processes of cervical vertebrae C6 through C2. At the level of each intervertebral disk from C5/6 to C2/3, it lies immediately adjacent to the uncinate process. Jung et al. (1974) and Lang (1991) pointed out the relative narrowness of the transverse foramina in relation to the lumen of the vertebral artery. Even head movements within the normal range of motion, in individuals with normal anatomy, can narrow the arterial lumen. The joints of the craniocervical junction create further possibilities for compression of the vertebral artery on movement.
Brown and Tissington (1963) found that rotation and reclination of the head caused marked narrowing of the vertebral artery on the opposite side. The two vertebral arteries constitute a functional unit, i.e., a disturbance of either of the two arteries can be compensated for by the other, because they join superiorly to form the basilar artery. This compensating mechanism is absent, however, if one of the vertebral arteries is nonfunctional to begin with, e.g., because of hypoplasia. The anatomy of the vertebral arteries is variable, and the arteries on the right and left sides may not have the same diameter. A hypoplastic artery on one side may explain the presence of unexpectedly severe symptoms in a patient with relatively mild changes of the uncovertebral joints. Because of the close anatomical relationship of the vertebral artery, sympathetic chain, and intervertebral disks, cervical syndrome can produce vascular and autonomic manifestations. The brainstem and inner ear may be affected, as these structures, among others, derive their blood supply from the vertebral artery (Fig. 9.4).
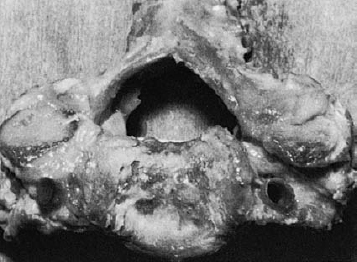
Fig. 9.4 Horizontal section of the C4/5 motion segment of a 23-year-old man. The lumen of the vertebral artery is immediately adjacent to the lateral portion of the uncinate process and to the soft tissue around the spinal nerve.
Our own studies have demonstrated that blood flow in the vertebral arteries depends on the position of the head (Oppel and Fritz 1986).
 The blood flow in the vertebral arteries is greatest when the cervical spine is in mild flexion.
The blood flow in the vertebral arteries is greatest when the cervical spine is in mild flexion.
More pronounced flexion of the cervical spine, the neutral position of the cervical spine, and extension (i.e., reclination of the head) are all associated with a reduction of blood flow (Fig. 9.5). Mild flexion also produces a marked widening of the intervertebral foramina (Grifka et al. 1989, Struckhoff 1994, Tomoaki et al. 2004).
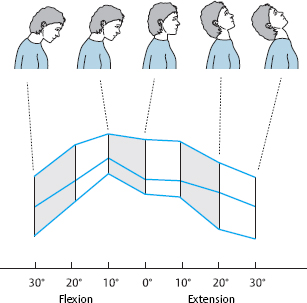
Fig. 9.5 Dependence of blood flow in the vertebral artery on head posture. Mild inclination (ca. 10°) affords better flow than the neutral position. Any deviation from this optimal position is associated with lower blood flow.
The blood flow in the vertebral artery may be tenuous because of arteriosclerosis, anatomical variants, or (most commonly) lateral osteophytes arising from the uncinate processes. If so, any additional factor, such as trauma or an abnormal posture of the cervical spine, may induce vertebrobasilar insufficiency, which can then be compensated for by mild flexion of the neck.
Cervical Nerve Roots and Nerve Root Sleeves
The lower cervical nerve roots and nerve root sleeves are of special clinical significance, particularly with respect to cervical spinal nerve analgesia. In this procedure, which is discussed in greater detail toward the end of this chapter, the nerve roots to be treated are flooded with local anesthetic injected via a dorsal approach. The physician doing the procedure must be aware of the topographical anatomic relationship of the bone, specifically the lateral mass of the cervical vertebra, to the exiting nerve root. As in all other regions of the spine, the proximal segment of a cervical nerve root is bathed in cerebrospinal fluid for a short distance within the so-called nerve root sleeve. If the local anesthetic is improperly injected into the nerve root sleeve because of faulty technique, it will enter the cervical subarachnoid space and affect the cervical spinal cord, with ensuing respiratory arrest and circulatory collapse.
Standard anatomy textbooks unfortunately tend to depict the central nervous system and the musculoskeletal tissues surrounding it in separate images, so that the student cannot gain a clear idea of the anatomical relationship of the bones and nerves. Lang (1991) described the apertures of the individual cervical nerve root sleeves receiving the bundled anterior and posterior fascicles of the cervical rootlets. The arachnoid, which typically fuses with the anterior and posterior root a few millimeters proximal to the spinal ganglion, is one component of the inner nerve sheath system. The dura mater of the nerve root sleeves is continuous with the fibrous layer of the perineurium. Frykholm (1951) studied the lower cervical nerve roots and their coverings and found that each root sleeve possesses two openings, one ventral and one dorsal, separated by a dural septum. Each root ostium leads to its own root sleeve, which is a lateral extension of the dural sac (Fig. 9.6).

Fig. 9.6 Nerve root sheaths and ostia (opened dorsally) (from Lang 1991).
1 C5 and C6 spinal ganglia.
2 Dura mater (reflected).
3 C6 dorsal root.
4 Dural spur between the ostia for the dorsal and ventral roots.
5 C6 ventral root and millimeter gauge (for scale).
6 Denticulate ligament.
7 Linea radicularis dorsalis (dorsal root entry zone, DREZ).
In the anatomy department of our institution, Heinze and Rubenthaler (2004) dissected the spinal nerves of C5–C8 bilaterally, marking their sites of exit from the spinal canal and demonstrating and measuring the nerve root sleeves (Fig. 9.7). They studied the relationship of the nerve root sleeves to the encasing bony structures of the intervertebral foramina. The root sleeves were measured with a probe and dissected under 16× magnification to demonstrate the transition to perineurial connective tissue. The root sleeves were then cannulated at their bony site of exit and marked by injection of methylene blue under high pressure. Finally, the intrathecal space was studied radiologically after the injection of contrast medium.
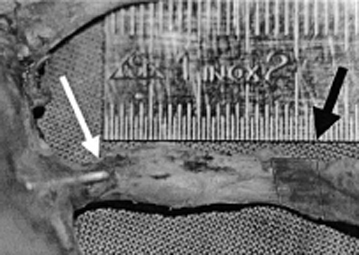
Fig. 9.7 Dissected lower cervical spinal nerve, with mark (black arrow) at the point of its lateral exit from bone. A probe lies in the nerve root sheath (white arrow). The distance from the lateral mark to the tip of the probe is measured with a ruler (from Rubenthaler 2005).
No layer that was separable from the nerve itself could be found lateral to the ganglion, even with sharp dissection. The ganglion lies proximal to the exit of the spinal nerve through the intervertebral foramen. It follows, therefore, that there is a safety zone (extending, in this study, from the outer mark on the root to the deepest point of the root sleeve than can be reached with the probe) in which the direct intrathecal injection of local anesthetic is not possible.
This study also revealed that the C5–C8 nerve roots are thick and lie closely adjacent to one another (Fig. 9.8). One must therefore assume that an infiltration of the C7 root for cervical spinal nerve analgesia will also affect the C6 and C8 roots if 5 mL or more of local anesthetic is injected. One can thus treat C8 irritation with an infiltration at C7 in order to minimize the risk of pneumothorax.
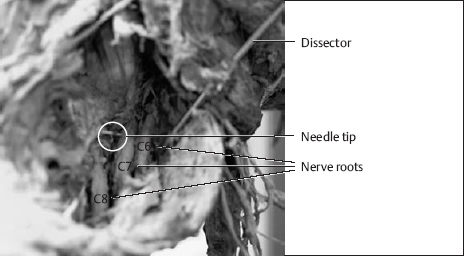
Fig. 9.8 The C5–C8 nerve roots, after removal of the soft tissue covering dorsally. Note the proximity of the roots to each other (from Theodoridis and Krämer 2006).
 Biomechanics
Biomechanics
 The cervical spine is the most mobile part of the axial skeleton. The head and neck can be moved in all directions. Much of this mobility is derived from the two uppermost segments, i.e., the segments of the craniocervical junction, which possess no intervertebral disks. The atlanto-occipital joint enables nodding movements, while the atlantoaxial joint primarily subserves rotation.
The cervical spine is the most mobile part of the axial skeleton. The head and neck can be moved in all directions. Much of this mobility is derived from the two uppermost segments, i.e., the segments of the craniocervical junction, which possess no intervertebral disks. The atlanto-occipital joint enables nodding movements, while the atlantoaxial joint primarily subserves rotation.
The remaining segments of the cervical spine all possess intervertebral disks; most of the mobility of the cervical spine is at C4/5–C6/7. The position of the joint facets enables movement in all directions at these levels as well, but forward and backward bending are favored, because the sagittally oriented uncinate processes serve as guides for these movements along their entire range (Jofe et al. 1983, Panjabi et al. 2005). The track-like uncinate processes thus limit rotatory movements of the cervical spine that might place excessive strain on the disks.
Flexion of the cervical spine, like flexion of (e.g.) the knee, is a process of rolling and sliding. The vertebral bodies do not merely tilt, they also slide in the dorsoventral direction, particularly in younger individuals. Radiographs reveal a typical staircase-like arrangement of the posterior edges of the cervical vertebrae. Flexion from the midposition leads to 2–3 mm of anterior displacement of each vertebra with respect to the one immediately below it, and extension leads to 1–2 mm of displacement in the opposite direction (Exner 1954).
Any movement of the cervical spine also alters the width of the intervertebral foramina at each level. Studies of dissected specimens, as well as radiological studies in vivo, have shown that the foramina are wider on the convex side of the laterally inclined cervical spine, and narrower on the opposite (concave) side. Forward bending or kyphosis of the cervical spine widens all of the intervertebral foramina, whereas backward bending or lordosis narrows them. These facts explain the posture that individuals suffering from an acute cervical syndrome typically assume to lessen nerve compression (acute torticollis, wry neck). The position in which the head is held, and the directions in which movement is resisted, are clinical clues pointing to the site of the lesion.
 The relatively heavy human head puts the cervical disks under high mechanical stress.
The relatively heavy human head puts the cervical disks under high mechanical stress.
Grob (1968) estimated the stress on the lower cervical disks at 550 kPa with normal head position and muscle tone, and 3900 kPa if muscle tone is absent. Panjabi et al. (2005) carried out biomechanical experiments on the cervical spine that yielded similar results. They also calculated the reduction of stress on the cervical spine that could be obtained with the Glisson kyphotic traction method (stretch test), demonstrating the potential usefulness of this method in the conservative management of cervical syndromes.
The nucleus pulposus of a cervical intervertebral disk changes its position in response to asymmetrical compression of the disk, just as the nucleus pulposus does in other regions of the spine. We studied the question whether the mobile, centrally located tissue of a cervical disk tends to be displaced in the same way as that of a lumbar disk when the disk is asymmetrically compressed. We did so by inserting a small metal bolt into the center of the nucleus pulposus in a dissected cervical motion segment specimen, then following its movements radiographically when the segment was manipulated (Stahl 1977). Asymmetrical compression, as expected, produced displacement of the bolt to the side that was under less pressure, i.e., dorsally when the stress was greater ventrally (in kyphosis), ventrally when the stress was greater dorsally (in lordosis), and to the convex side on lateral bending (Fig. 9.9). The degree of displacement was surprisingly large after no more than a few minutes of asymmetrical compression. If the compression was kept up for some time and then released, displacement of the nucleus pulposus was still evident several hours later. The mobility of the central disk tissue in response to asymmetrical compression is greater in adolescents and young adults than in elderly individuals.
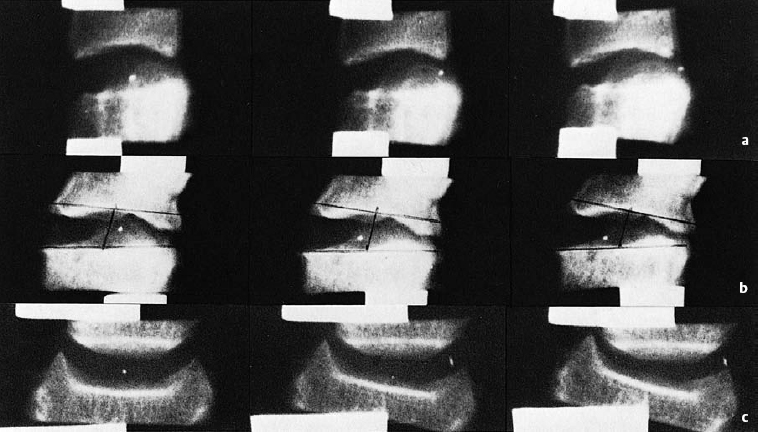
Fig. 9.9 a–c Mobility of central disk tissue (marked with a metal bolt) with asymmetrical compression of the C4/5 intervertebral disk of an 18-year-old man (50–100 kPa of pressure, or 500–1000 N of force).
a Compression of the anterior edge (kyphosis).
b Compression of the posterior edge (lordosis).
c Lateral compression.
 Any maintained asymmetrical posture of the cervical spine can be expected to cause intradiscal tissue displacement.
Any maintained asymmetrical posture of the cervical spine can be expected to cause intradiscal tissue displacement.
Such tissue displacements play a role in the pathogenesis of cervical syndromes.
 Special Pathoanatomy and Pathophysiology
Special Pathoanatomy and Pathophysiology
Degenerative changes of the lower cervical motion segments begin to appear at an early age, though they are not evident in radiological studies till later on in life. Their main cause is the mechanical stress associated with the larger excursions of movement in these segments, compared to the relatively immobile thoracic spine. The intradiscal pressure is also higher at cervical than at thoracic and lumbar levels, because of the weight of the head. Nor is there, in the cervical spine, any counterpart to the mechanism of reducing the intradiscal pressure in the lumbar spine by raising the intra-abdominal pressure (abdominal pressing, Valsalva maneuver).
Persistent mechanical stress and the wide range of motion of the cervical spine, particularly with regard to rotation, lead to overstretching of the anulus fibrosus, which, in turn, results in anular tears and intradiscal tissue displacement. This situation predisposes to disk protrusion.
 The horizontal fissures are the primary sites of occurrence of pathological changes in the cervical motion segments.
The horizontal fissures are the primary sites of occurrence of pathological changes in the cervical motion segments.
The joint-like construction of the horizontal fissures is biomechanically ideal only for a short time, because these fissures tend to spread both medially and laterally.
Laterally, the outermost fibrous lamellae of the anulus fibrosus remain in place while the disk begins to protrude in the direction of the intervertebral foramen. The fissures also provide a path along which mobile disk material can find its way toward the boundaries of the disk and beyond, though the site of potential egress remains narrow. Töndury (1958) found contained disk protrusions in histological sections of the uncovertebral region even in the cervical spine of children: the overstretched inner fibrous lamellae bulged out through tears in the outer lamellae, without at first overstepping the boundary of the intervertebral disk itself. In adults, Töndury found nucleus pulposus tissue that had nearly found its way out of the disk along the horizontal fissure and was held back merely by the ligamentous bands around the uncovertebral joint, which served as a kind of joint capsule. Such protrusions of disk tissue can occur only when the turgor pressure in the disk is normal or elevated, which is the case only in relatively young individuals (Figs. 9.10, 9.11). Indeed, Töndury found moderately large cervical disk protrusions only in young people. Elderly individuals had dried-out disk tissue that did not protrude outside the boundaries of the disk even in the presence of full-thickness horizontal tears.
The horizontal fissures can spread so far medially that they actually cut the cervical disk in half. It is then held together only by the joint capsules and the ligaments between the vertebrae. The movement segment is lax and unstable.
 Lateral spread of the horizontal fissures disturbs the osmotic system of the disk.
Lateral spread of the horizontal fissures disturbs the osmotic system of the disk.
The boundaries of the intervertebral disk become permeable to larger molecules as well as smaller ones, so that the intradiscal osmotic pressure falls; the disk consequently dries out and loses height. The vertebrae above and below it come closer together, making a greater degree of bony contact at the uncinate processes and the intervertebral joints. The uncinate processes bend laterally and develop bony appositions. Reactive thickening of bone occurs on the bony surfaces of the upper vertebra opposite the uncinate processes of the lower one. The uncovertebral region develops a new, supportive function. The uncinate processes and their cartilaginous lining are biomechanically not up to the task, however, and they soon develop arthrosis-like changes as a result.
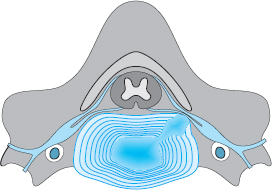
Fig. 9.10 Dorsolateral displacement of central, mobile disk tissue (nucleus pulposus) with compression of a cervical nerve root.

Fig. 9.11 Prolapsed nucleus pulposus tissue (arrow) protruding in mushroom-like fashion under the uncovertebral ligamentous connection. The fissure communicates internally with the anulus pulposus cavity (from Ecklin U. Die Altersveränderungen der Halswirbelsäule. Berlin: Springer; 1960).
 The osteophytic reaction of the uncinate processes and the loss of disk height lead to narrowing of the intervertebral foramen.
The osteophytic reaction of the uncinate processes and the loss of disk height lead to narrowing of the intervertebral foramen.
As Fig. 9.12 shows, this narrowing is due not only to the bony extensions of the uncinate process that are visible in the radiograph, but also to the radiolucent soft tissue surrounding the bone. Sometimes this soft tissue alone suffices to compress a cervical nerve root and produce clinical symptoms, even in the absence of visible intervertebral foraminal stenosis on an oblique plain radiograph of the cervical spine.
Once the intervertebral foramen is sufficiently narrowed, nerve root irritation and signs of vascular compression can appear. The cervical intervertebral foramina are narrower than the thoracic and lumbar ones and are thus more vulnerable to osteogenic constriction. This constriction is produced by uncovertebral exostoses in combination with the telescoping of the intervertebral joint facets due to osteochondrotic disk collapse, which narrows the upper portion of the intervertebral foramen in particular. Unlike lumbar nerve root irritation, cervical nerve root irritation is usually not caused by direct pressure of the disk on the nerve, but rather by the secondary effects of disk degeneration on the sides of the vertebrae and on the intervertebral joints. The peak age for cervicobrachialgia is accordingly 10 years later than that for sciatica.
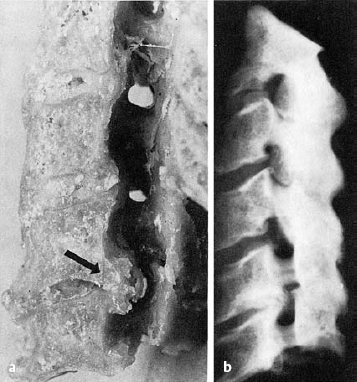
Fig. 9.12 a, b Parasagittal section of the cervical spine of a 65-year-old man: anatomical specimen (a) and radiograph (b). Note the osteophytic reactions on the uncinate process and on the surface of the vertebral body opposite, with narrowing of the C5/6 intervertebral foramen.
All other degenerative changes, such as spondylosis, osteochondrosis, and spondylarthrosis, occur in the cervical spine just as they do elsewhere in the spinal column.
 The C5/6 and C6/7 segments are affected earliest and most frequently because they are under the greatest mechanical stress.
The C5/6 and C6/7 segments are affected earliest and most frequently because they are under the greatest mechanical stress.
Monoradicular nerve root irritation syndromes also affect these motion segments more frequently than others (see Fig. 9.20).
 95–100% of people over age 70 have spondylotic changes of the cervical spine of greater or lesser severity.
95–100% of people over age 70 have spondylotic changes of the cervical spine of greater or lesser severity.
Loss of disk height causes a loss of lordosis and a fixed, extended position of the osteochondrotic segments, which is compensated for by hyperlordosis of the segments above and below.
Arthrotic changes of the intervertebral joints (spondylarthrosis) are rarer than was previously thought. As the cervical disks lose height, the uncinate processes come into contact with the vertebral bodies above before the joints can be exposed to any marked elevation of mechanical stress. Intervertebral joint arthrosis is generally more severe in the upper and middle portions of the cervical spine than at C5/6 and C6/7.
Fibrous ankylosis with ingrowth of organized vascular connective tissue finally leads to a comfortable rigidity of the affected cervical motion segments.
Osteophytes and areas of bony thickening regress once the bony support elicited by slackening of the intervertebral disks is no longer needed. The loss of function resulting from the immobilization of multiple motion segments is well tolerated by older individuals because most of the mobility of the head is provided by the two uppermost (i.e., atlanto-occipital and atlantoaxial) segments.
Summary
The special feature of the anatomy of the cervical intervertebral disks is their proximity to important neural and vascular structures. The vertebral artery, the spinal nerve, and the spinal cord are all immediately adjacent to the disk, and these structures may be impinged upon in acceleration–deceleration injuries of the cervical spine, during sporting activities, or during passive movement of the neck in manual therapy. Mild flexion of the neck optimizes (i.e., increases) the distance between the skeletal and neurovascular elements, whereas extension decreases it. This explains the marked positional dependence of disk-related symptoms in the cervical spine.
A special biomechanical feature of the human cervical spine is the apparent disproportion between the relatively heavy head and the relatively small cervical disks. This, combined with the wide range of motion of the neck in all directions, results in a high potential for injury. Because of their unfavorable biomechanical situation, the lower cervical motion segments tend to show early signs of wear and tear. Clinical manifestations tend to be produced particularly by such changes occurring in the region of the uncinate process and intervertebral foramen.
Conclusion
The cervical spine moves freely in all directions, bears the relatively large weight of the head, and lies in the immediate vicinity of important neurovascular structures. These features combine to make it one of the more injury-prone areas of the axial skeleton.
 Clinical Features of Cervical Syndromes
Clinical Features of Cervical Syndromes
Overview of Symptoms and Their Classification
The term “cervical syndrome” refers to any disease state directly or indirectly caused by degenerative changes of the cervical intervertebral disks. Thus, it covers not only conditions with painful limitation of movement of the cervical spine, but also excessive muscle tension in the shoulder and neck, segmental radicular syndromes of the upper limb, cervicogenic headache and dizziness, spinal cord syndromes, cochleovestibular irritative conditions, and various functional disturbances arising in the internal organs. Any systematic classification of such a wide-ranging group of illnesses is necessarily imperfect, regardless of whether it is based on a fundamental subdivision by localization (upper vs. lower) or by disease course (acute vs. chronic).
A strict separation of each one of these conditions from all the others is often not possible, because each condition may consist of a large number of different symptoms that change, or vary in severity, over time, and the clinical pictures of different conditions often overlap. We consider a division of cervical syndromes into upper, middle, and lower to be potentially misleading, as it is definitely not the case that all of their symptoms can be attributed, respectively, to pathology in the upper, middle, or lower regions of the cervical spine.
 Nearly all cervical syndromes are due to pathology in the lower cervical motion segments, no matter which segments manifest the greatest degenerative disturbances of form and function.
Nearly all cervical syndromes are due to pathology in the lower cervical motion segments, no matter which segments manifest the greatest degenerative disturbances of form and function.
A separation of cervical syndromes into acute and chronic is likewise problematic, because the course of disk-related complaints is highly variable.
Our classification is mainly based on the participation of individual spinal nerve roots in the generation of symptoms. In most cases, multiple roots participate, with one root playing the most prominent role.
Patients’ Description of Symptoms
The patient’s own description of the symptoms is all the more important as a clue for the diagnostician because objective signs are often absent (for which reason medicolegal assessment is often difficult). In our series of patients presenting to private orthopedic practices, we always record the patient’s chief complaint in their own words.
The typical pains in the shoulder and neck, combined with stiffness in the cervical spine, tend to arise suddenly and to be precipitated by rotation of the head or by prolonged maintenance of a kyphotic posture for reading, watching television, or working at a desk (Table 9.1). Patients often draw a connection between the initial appearance of symptoms and cooling of the shoulder and neck muscles by a draft of air, e.g., in an air-conditioned room or while driving.
 Sudden onset Sudden onset | |
 Positional dependence Positional dependence | |
 Pain worse at night Pain worse at night |
 A maintained improper posture (generalized cervical kyphosis under mechanical stress), increased muscle tension due to lower temperatures, and muscle tension raising the intradiscal pressure are important pathogenetic mechanisms for cervical syndromes.
A maintained improper posture (generalized cervical kyphosis under mechanical stress), increased muscle tension due to lower temperatures, and muscle tension raising the intradiscal pressure are important pathogenetic mechanisms for cervical syndromes.
The symptoms sometimes appear as soon as the patient wakes up in the morning. They are position-dependent: typically, they can be brought on or exacerbated by certain movements and positions of the cervical spine. The patient assumes a protective posture (which takes an extreme form in acute torticollis). Patients often state that they can partially relieve the pain with a movement in the opposite direction or with manual pressure on one side of the head. Patients should be asked specifically about the positional dependence of their symptoms, as this may yield important clues for differential diagnosis.
Worsening of symptoms at night is characteristic of cervical syndromes. The patient is awakened by the pain. Because of the normal diminution of muscle tone and absence of voluntary muscle contraction during sleep, the patient involuntarily assumes positions that induce pain. For example, pronounced lateral bending combined with hyperlordosis narrows the intervertebral foramina on the concave side of the bend. Once the nerves and vessels in the foramen are mechanically irritated, a vicious circle of neurovascular irritation, pain, and muscle contraction is set up. Sleeping prone or propped up on too many pillows can predispose to such situations. The pain is usually combined with a feeling of stiffness. The various kinds of symptom that can arise include shoulder and neck pain, paresthesiae, occipital pain, tinnitus, syncopal attacks, a feeling of tightness in the chest, and migraine-like phenomena.
In addition to the specific symptoms just described, patients also complain of general accompanying symptoms such as fatigue, irritability, and impaired concentration. Functional disturbances of the internal organs, including the heart, may also arise. In contrast to the relatively stereotypic complaints of organic heart diseases, spondylogenic pseudo-cardiac symptoms come in a dazzling variety of forms, including palpitations or a stabbing, pulling, rippling or tearing sensation. These symptoms are induced by certain postures of the cervical spine and can be relieved by traction in a Glisson sling.
Most patients presenting with cervical complaints to a physician’s office or outpatient clinic seem to have a certain degree of emotional coloring of symptoms. We have confirmed this impression in our own outpatient clinic with psychological testing.
 Patients with cervical syndrome have more emotional abnormalities than a comparable group of normal control individuals.
Patients with cervical syndrome have more emotional abnormalities than a comparable group of normal control individuals.
There is no longer any doubt about the purely mechanical and organic cause of cervical syndromes. It therefore seems to be the case that continual, deep pain in the shoulder and neck, present day and night and interfering with sleep, can in the long run disturb the patient’s emotional balance. The physician must bear this in mind when dealing with such patients, and especially when prescribing treatment and observing its effects.
Clinical Findings
The clinical findings in patients with cervical syndromes fall into two major categories. In the first category are those findings that generally indicate a disorder of the cervical spine, such as muscle tension in the shoulder and neck, painful restriction of cervical movement, and tenderness to pressure in the entire region of the neck; in the second category are the findings that allow precise segmental localization. These include circumscribed tenderness of a single spinous process to pressure or shaking, restriction of movement of a single motion segment, segmental radicular manifestations, and, lastly, the findings of special tests such as EMG, neurography, myelography, discography, CT, MRI, and the distension test.
The clinical examination begins, as always, with inspection. The experienced clinician will immediately notice a certain degree of neck stiffness that is maintained while the patient undresses and dresses. The shoulders are often held high. Above all, the patient takes care not to rotate the head and prefers to turn with the entire trunk. The oblique posture of the head in torticollis (wry neck) is unmistakable and often grotesque. Only by keeping the head in this position can the patient derive some relief of symptoms (as the examiner must remember while testing the range of motion). The cervical spine is not only laterally flexed and rotated, but also bent forward (kyphosed) to a certain degree, as can be seen in a lateral plain radiograph. Our studies have shown that this position decompresses the neurovascular structures in the uncovertebral region to the greatest possible extent.
Palpation reveals tension of the shoulder and neck muscles. Pressure-sensitive local muscle hardening (“myogelosis”) is found mainly at the upper edge of the trapezius from the occiput to the acromioclavicular joint, in the scalene region, and in the rhomboid muscles. The spinous and transverse processes are also tender to palpation. The transverse processes of the atlas can be palpated in the mandibulomastoid angle. Tenderness is usually found bilaterally at these preferred sites, but more intensely on the affected side.
Functional testing of the cervical spine in cervical syndromes nearly always reveals a restricted range of motion, though the restriction may be limited to one or a few segments. One should test forward and backward bending (distance of chin from sternum), lateral bending, and rotation. The ranges of motion in each direction should be reported in degrees from the neutral position. The absolute ranges of motion of the cervical spine vary naturally with the length of the neck, the degree of muscularity, and the age of the patient. Thus, pathologically restricted movement is best detected by the difference between the ranges of motion on the two sides and by pain produced at the end of the range of motion in any particular direction.
Testing of segmental mobility is performed with the patient first in the supine position, and then sitting. The edges of the joint facets and transverse processes of each successive segment are fixed by the examiner’s hands while the patient carries out rotatory, lateral bending, and flexion–extension movements of the segment above.
Functional testing of the cervical spine should always include a distension (stretch) test (also known as the Glisson test). The examiner stands behind the patient, takes hold of the patient’s mastoid processes with the palms of the hands, rests the forearms on the patient’s shoulders, and pushes the patient’s head upward. This maneuver momentarily produces strong axial traction on the cervical spine. If the patient reports temporary relief of shoulder and arm pain, this is of diagnostic significance (Fig. 9.13) and points to potentially beneficial forms of therapy.
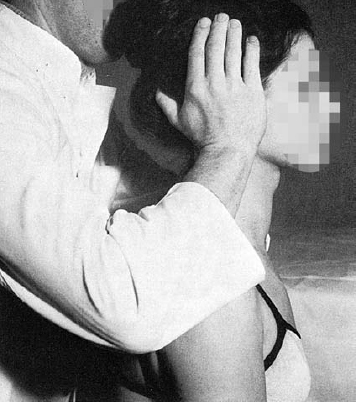
Fig. 9.13 Glisson test of the cervical spine: the examiner holds the patient’s mastoid processes in the palms while supporting the forearms on the patient’s shoulders and pushing the patient’s head upward. This type of grip is also used in manual therapy.
Finally, the clinical examination of a patient with a cervical disk syndrome must always include a neurological examination. The single most important piece of localizing information for a cervical radicular irritation syndrome is the patient’s description of the pattern of radiation of sensory symptoms. The patient should be asked to outline the band of pain and the area of paresthesia as accurately as possible with one finger. Objective neurological signs such as reflex asymmetry, paresis, muscle hypotonia, atrophy, and hyperesthesia should always be sought as well, though they are relatively rarely seen in cervical disk syndromes.
Radiological Studies
Radiological studies and basic laboratory tests are also a routine part of the evaluation of cervical syndromes. Radiological imaging can effectively rule out tumors (metastases) and infection (spondylitis) as the cause of symptoms. Its usefulness in the precise diagnosis of cervical syndromes and their localization to a particular motion segment is generally overrated, however, and is in fact limited. As already pointed out, cervical spondylosis and osteochondrosis are almost ubiquitous concomitants of aging and are usually of no clinical significance.
The routine radiological evaluation of cervical syndromes consists of anteroposterior and lateral plain radiographs of the entire cervical spine (Fig. 9.14). The anteroposterior view reveals any deviation of the spinal axis from the vertical in the frontal plane and displays the state of the uncinate processes at middle and lower cervical levels. If the disk has lost height and the uncinate processes make contact with the vertebral body above, they are flattened, so that the end plate is dish-shaped. In advanced spondylarthrosis, joint osteophytes are seen to project from the lateral border of the cervical spine.
The lateral view is more important than the anteroposterior view for the exclusion of metastases and infection and for the detection of degenerative disk disease. Disk narrowing, sclerosis of the corresponding upper and lower end plates, and spondylotic projections jutting anteriorly from the lower edge of the cervical vertebrae should not be interpreted as the cause of the present symptoms, but rather as evidence of earlier disk slackening that has, by now, run its natural course.
One should avoid being overly impressed by abnormalities seen in plain radiographs.
 Even massive spondylotic osteophytes, disk collapse, and close approximation of neighboring vertebrae may be associated with only mild symptoms or none at all.
Even massive spondylotic osteophytes, disk collapse, and close approximation of neighboring vertebrae may be associated with only mild symptoms or none at all.
These changes are usually found incidentally. The clinical findings alone are decisive.
 The only radiological finding of direct relevance to an acute cervical disk syndrome is a possible loss of the physiological lordosis due to muscle spasm.
The only radiological finding of direct relevance to an acute cervical disk syndrome is a possible loss of the physiological lordosis due to muscle spasm.
For the lateral radiograph, the patient’s head must be in the normal, neutral position, with the neck bent neither forward nor backward. The symptomatic flattening of the lordosis may be limited to one or a few cervical segments. Segmental loss of lordosis, visible as a mild kyphotic kinking of the cervical spine, is caused by reflexive muscle spasm. The patient involuntarily assumes a kyphotic posture to open the intervertebral foramina in the affected motion segment as widely as possible. The associated dorsal widening of the disk space additionally counteracts discogenic nerve compression.
 In most cases, all motion segments above the site of the lesion are abnormally kyphotic (Güntz sign).
In most cases, all motion segments above the site of the lesion are abnormally kyphotic (Güntz sign).
In acute cervical disk syndromes, generalized loss of lordosis and segmental kyphosis can also be seen on functional (dynamic) lateral plain radiographs obtained with maximal forward and backward bending of the neck. The abnormal findings on forward bending (inclination) include not only the dorsally convex arch of the cervical spine but also a mild ventral displacement of each cervical vertebra on the one below it, the so-called staircase phenomenon. This is seen mainly in younger individuals and may be more pronounced in a single segment where there is additional pathology of the intervertebral disk.
A further means of “objectifying” degenerative segmental slackening is provided by the radiological stretch test described by White and Panjabi (1978) and Panjabi (2004). Lateral plain radiographs and a neurological examination are carried out before and during Glisson traction of the cervical spine at one-third of body weight.
The evaluation of cervicobrachial and cervicocephalic syndromes should also include oblique plain radiographs of the cervical spine for visualization of the intervertebral foramina (Fig. 9.14 c). These may show osteophytes growing from the uncinate process and narrowing the foramen. The degenerative changes of the uncinate processes are seen on oblique radiographs as either sharp or blunt bony projections pointing laterally toward the foramen. The lower vertebral body end plate lying opposite often displays reactive sclerosis and osteophyte formation.

Fig. 9.14a–c Anteroposterior (AP), lateral, and oblique radiographs of the cervical spine. The osteophytic reactions on the uncinate processes can be seen in the AP and oblique views (a, c); the lateral view (b) reveals narrowing of the C5/6 intervertebral space.
Our measurements in radiographic images and dissected specimens have revealed that the radiographs show only a part of the uncovertebral protrusion, i.e., its hard, bony, radiodense core (see Fig. 9.12). This core, however, is often covered by a tough connective tissue layer that is composed of remnants of the anulus fibrosus and the longitudinal ligaments and is therefore invisible on plain radiographs. Thus, the nerve root may be compressed within the foramen by encroachment of the uncinate process even in the absence of radiologically evident critical foraminal narrowing.
 Conversely, however, one often finds quite marked osteophyte formation from the uncinate processes, with marked radiologically evident narrowing of the intervertebral foramina, in the absence of any symptoms of nerve root compression. This is most often the case in older individuals.
Conversely, however, one often finds quite marked osteophyte formation from the uncinate processes, with marked radiologically evident narrowing of the intervertebral foramina, in the absence of any symptoms of nerve root compression. This is most often the case in older individuals.
Cervical intervertebral foraminal stenosis is of clinical significance mainly when it arises rapidly, so that the nerves and vessels have no time to adapt. Rapid decreases in foraminal size can be caused, for example, by slackening of the motion segment, leading to a situation in which the relative position of the two adjacent vertebral bodies is constantly changing.
CT and MRI
These neuroimaging techniques enable the visualization of cervical disk prolapses. Myelography is only rarely needed for the exclusion of relevant types of neurological disease (Figs. 9.15, 9.16).

Fig. 9.15 Cervical spine MRI revealing C4/5 and C5/6 disk protrusions with well-hydrated (soft) sequestra. Conservative management.
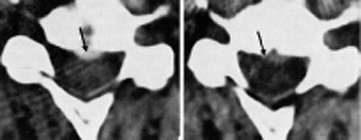
Fig. 9.16 Cervical spine CT revealing a broad-based median disk protrusion at C4/5, which lightly indents the dura mater in the midline (arrow). Conservative management.
CT can be used to image the entire cervical spine or only the clinically relevant part of it, to limit radiation exposure. Cervical CT reveals the width of the vertebral canal and the extent of the osteophytic reaction at the uncinate processes. CT after the intrathecal injection of contrast medium enables visualization of the nerve root sleeves.
MRI enables visualization of the entire cervical spine and is particularly good for showing the intervertebral disks. Disk protrusions are best seen in the sagittal sections. Over-interpretation of MR images should be avoided (Siivola et al. 2002, Ullrich 2005).
 MRI shows disk protrusions as being larger than they really are.
MRI shows disk protrusions as being larger than they really are.
Neurophysiological Testing: EMG
Neurophysiological methods are useful for the differentiation of nerve root compression syndromes and cervical spondylogenic myelopathy from systemic diseases such as multiple sclerosis and amyotrophic lateral sclerosis, as well as from peripheral compression syndromes such as carpal tunnel syndrome. They also provide important information about the severity and extent of damage of the sensory and motor pathways. Preoperative neurophysiological assessment of the peripheral nerves (neurography, EMG), the pyramidal pathways (motor evoked potentials), and the afferent pathways of the posterior columns (somatosensory evoked potentials) is helpful not just to confirm the indication for a surgical procedure, but also as a baseline test that can be compared with postoperative follow-up studies (Dvořák 1996, 2002)
The more time-consuming motor and somatosensory evoked potentials play a less important role than conventional EMG in the diagnostic evaluation of cervical radiculopathy. Evoked potentials are very useful, however, in the evaluation of spinal stenosis with possible spinal cord compression.
EMG is a major aid to the objectification of cervical root dysfunction. The muscle action potentials, detected either at the skin or directly from muscle with needle electrodes, are amplified, displayed, and recorded to reveal the state of the muscle and of the nerves supplying it. EMG abnormalities can often be seen before any clinical signs such as paresthesia or muscle atrophy.
EMG technique. Muscle action potentials are recorded with a needle electrode at various positions and at various depths to ensure that a representative picture of muscle activity is obtained. The electrical activity of the skeletal muscle is recorded and analyzed. EMG requires the cooperation of the patient; it is time-consuming and, at times, painful. It should be done only in selected cases to answer specific questions (Dvořák and Haldeman 2004).
Indications. Nerve root compression not only causes segmental pain and paresthesia, but also impairs motor activity in the muscles that are mainly supplied by the root in question. EMG can thus be used to determine which nerve root is involved, with important therapeutic implications (e.g., for selective cervical root block procedures). The indications for EMG in cervical syndromes include the following:
 differentiation from carpal tunnel syndrome
differentiation from carpal tunnel syndrome
 differentiation of isolated discogenic nerve root compression from a systemic neurological disease
differentiation of isolated discogenic nerve root compression from a systemic neurological disease
 differentiation of radicular from peripheral nerve lesions
differentiation of radicular from peripheral nerve lesions
 determination of the severity of neural involvement
determination of the severity of neural involvement
 assessment of the extent of re-innervation, if any.
assessment of the extent of re-innervation, if any.
Findings. Cervical nerve root compression usually causes no more than a mild slowing of motor and sensory nerve conduction. This is not surprising, as the speed of conduction is measured in the region of the forearm and hand, although the lesion is much more proximal. Only severe, chronic radicular compression syndromes are accompanied by muscle atrophy with reduced amplitude of muscle action potentials and by a low-amplitude or undetectable sensory nerve action potential. F-waves are often harder to generate, or their latency is prolonged (Dvořák 1996, Dvořák and Haldeman 2004). Comprehensive and detailed descriptions of EMG findings can be found in Conrad and Bischoff (1988), Hopf (1988), Dvořák (1998, 2002), Haig et al. (1998), Mumenthaler et al. (1998), Nargol (1998), Balague (1999), Hirayama (1999), Krämer and Nentwig (1999), Perlick et al. (1999), Colloca (2000), Greenough (2003), and Dvořák and Haldeman (2004).
 General Differential Diagnosis
General Differential Diagnosis
Cervical syndromes produce many different kinds of symptoms and signs and their differential diagnosis is correspondingly broad. Any type of cervical discogenic syndrome must be distinguished from similar clinical pictures due to other kinds of disease. A cervical syndrome can only be confidently diagnosed when all other possibilities have been ruled out.
 Cervical syndromes should be diagnosed by exclusion.
Cervical syndromes should be diagnosed by exclusion.
The high prevalence of disk disease must not tempt the clinician to diagnose a cervical syndrome, and then immediately begin treating it, after a cursory clinical examination of a patient complaining of pain in the shoulder and neck. Massage, traction, and manual therapy may have decidedly negative consequences in patients who are actually suffering from a vertebral metastasis or spondylitis. On the other hand, the primary battery of diagnostic tests should be chosen so as to avoid unnecessary expense. Thus, it generally suffices to carry out a thorough clinical examination, including a neurological examination, supplemented by a basic laboratory profile and a plain radiograph series of the cervical spine. The sudden onset and positional dependence of the symptoms are highly suggestive evidence of a discogenic syndrome. The age of the patient is a further diagnostic criterion (cf. age-related prevalence curves, Fig. 9.1). Unexpected features of the following types should prompt further testing:
 insidious onset
insidious onset
 persistent pain independent of position
persistent pain independent of position
 advanced age
advanced age
 elevated erythrocyte sedimentation rate (ESR)
elevated erythrocyte sedimentation rate (ESR)
 bone destruction in plain radiographs
bone destruction in plain radiographs
 fever
fever
 abnormalities in the complete blood count, with differential.
abnormalities in the complete blood count, with differential.
Unclear neurological findings can be further investigated with MRI, CT, cervical myelography, EMG, and evoked potentials.
Classification of Cervical Syndromes
“Cervical syndrome,” as we have seen, is a general term covering all cervical spine problems due to the degenerative process rather than to a tumor, infection, or developmental anomaly. If the symptoms are limited to the cervical spine, the disorder is called a local cervical syndrome, and the patient is said to be suffering from neck pain (just as the patient with a local lumbar syndrome suffers from low back pain). Neck pain, in turn, is subdivided into two kinds, simple and complex. Simple neck pain regresses rapidly, whereas complex neck pain carries a risk of becoming chronic (for the danger signs, see Table 9.2).
Simple neck pain is usually mechanically induced, e.g., by an unthinking, sudden movement, but can also arise spontaneously, e.g., after a draft of cold air on the nape of the neck. The pain is typically motion-dependent, moderately severe, and short-lasting, with spontaneous remission in 3–6 days. A longer duration is likelier if there are complicating psychosocial factors (a danger sign!), if the pain is severe enough to disturb sleep, or if it has already lasted longer than a week. Particular attention should be paid to recurrent neck pain in adolescents or elderly people.
Similar considerations apply to the cervicobrachial syndrome, i.e., to pain in the neck radiating into the shoulder and arm, no matter whether it is of radicular or pseudoradicular type. Here, too, simple neck and arm pain, with proximal radiation, moderate severity, and brief duration, can be contrasted with complicated neck and arm pain, which is usually in a radicular distribution, radiating as far down as the hand, and sometimes accompanied by weakness.
The term “cervicocephalic syndrome” encompasses all pains in the head and neck with origin in the cervical spine, with or without associated dizziness, visual or auditory dysfunction, or dysphagia. Head and neck pain often arises after an acceleration–deceleration injury of the cervical spine (see Chapter 17).
Dangerous varieties of head and neck pain include the pain of cervical myelopathy (often accompanied by gait disturbance and weakness) and pain due to a tumor, infection, or malformation (see the section on differential diagnosis, p. 93).
Local Cervical Syndrome
Etiology and Symptoms
 Definition: the term “local cervical syndrome” refers to any combination of clinical manifestations that is confined to the neck and is the direct or indirect result of degenerative and functional disturbances of the cervical motion segments.
Definition: the term “local cervical syndrome” refers to any combination of clinical manifestations that is confined to the neck and is the direct or indirect result of degenerative and functional disturbances of the cervical motion segments.
These conditions are characterized exclusively by position-dependent shoulder and neck pain, muscle tension, and restricted movement of the cervical spine (Table 9.3).
 Position-dependent shoulder and neck pain Position-dependent shoulder and neck pain |
 Restricted range of motion of cervical spine Restricted range of motion of cervical spine |
 Tension of neck and shoulder girdle musculature Tension of neck and shoulder girdle musculature |
The symptoms are caused by degenerative and posttraumatic changes of the cervical motion segments, which produce mechanical irritation of the posterior longitudinal ligament, the intervertebral joint capsules, and the vertebral periosteum. The sensory fibers of the meningeal and dorsal branches are predominantly affected. Local cervical syndrome can be either acute or chronic. Any symptoms that can be shown to originate in the intervertebral joint capsules (e.g., by injection of local anesthetic) are designated as cervical facet syndrome, which is analogous to its lumbar counterpart. Clinical studies indicate that the facet joint is the origin of a good percentage of lumbar and cervical spinal pain. Studies using diagnostic blocks suggest that the incidence of cervical facet pain is higher than that of lumbar facet pain (Cavanaugh, 2006).
Local cervical syndromes are the most common disk-related clinical conditions of the cervical spine. Precise epidemiological data are impossible to obtain, because most individuals with local cervical syndromes probably have only mild symptoms and therefore do not seek medical attention. Furthermore, the condition is often self-limiting and responds well to traditional household remedies such as heating pads, hot-water bottles, etc.
Among the more prominent symptoms of local cervical syndromes is painful muscle tension in the shoulder and neck. The muscles in these areas are supplied by the dorsal branches of the spinal nerves. A precise segmental localization of the etiology of the pain is not possible, because each muscle is supplied by the dorsal branches of more than one nerve (the pattern of innervation of the ventral branches is more highly segregated). The onset of symptoms may be acute, e.g., after abrupt turning of the head, or gradual without any particular precipitating factor. Patients often mention a cool draft as a possible cause; another common precipitant is prolonged sitting in a hunched position with a kyphotic posture of the neck, e.g. while typing, reading, or working at a desk. Pain in such situations is not only discogenic but also partly due to muscular insufficiency.
On examination, the patient can localize the pain fairly precisely. Pain due to involvement of the upper cervical segments is localized to the territory of the dorsal branches of the spinal nerves on the upper border of the trapezius muscle, which stretches from the occiput to the acromioclavicular joint.
 Irritation of the lower cervical motion segments causes pain between the shoulder blades.
Irritation of the lower cervical motion segments causes pain between the shoulder blades.
In the latter situation, there is tenderness of the rhomboids and of the levator scapulae and subscapularis muscles.
In addition to the typical localization of the pain, examination also reveals a greater or lesser degree of spasm of the entire musculature of the shoulder and neck, with resulting restriction of neck movement. The pain may radiate into the shoulder and the dorsolateral portion of the arm; because it does not extend into the forearm and does not follow a radicular pattern, it is called “pseudoradicular brachialgia.” Discography with a disk-distension test (see p. 121) can often provoke pain of this type.
Occipital neuralgia is a special type of local cervical syndrome. This is a local process in the nuchal–occipital region involving irritation of the greater occipital nerve, which lies just below the skin at the level of the external occipital protuberance (inion) and is tender to palpation at this point. The tender tendinous insertions of the upper portions of the trapezius muscles are immediately adjacent.
Local cervical disk syndromes have a chronic, recurrent course. Symptom-free intervals lasting months or even years alternate with bouts of very severe symptoms. Patients are often aware of their own individual precipitating factors (cooling, maintained unfavorable postures) and do their best to avoid them.
Differential Diagnosis
Tumors and infections can, depending on their precise location and extent, produce symptoms resembling those of a local cervical syndrome. Primary tumors of the cervical spinal cord, such as neurinomas of the spinal nerve roots and spinal meningioma, are rare compared to metastases into the cervical spine. The common sources of metastases include tumors of the bronchi, breast, thyroid gland, and kidney. The presence of a tumor may be suggested by the insidious onset of symptoms, abnormal laboratory findings, evidence of bone destruction on plain radiographs, or a deterioration of the patient’s general condition (weight loss). These patients are also usually elderly. Their further diagnostic evaluation includes tomographic imaging of the cervical spine, bone scan, further laboratory tests, and, most importantly, a search for the primary tumor.
Infection (spondylitis) reveals itself in an elevated CRP and ESR, as well as fever. The loss of disk height that accompanies discitis can be mistaken, at first, for intervertebral chondrosis. Rheumatoid arthritis, too, commonly affects the cervical intervertebral joints.
The differential diagnosis of local cervical syndromes, like that of all other spinal diseases, must include ankylosing spondylitis (Bekhterev disease) (respiratory excursion, Schober distance). When this disease is suspected, plain radiographs of the sacroiliac joints should be obtained, even if there is no pain in these joints.
Sternal syndrome, as described by Brügger (1971), consists of pain arising in the sternum and sternoclavicular joints and leading to painful reflex contraction of the musculature of the shoulder girdle and neck. Pain due to excessive mechanical stress on the sternum usually comes about after prolonged sitting in a hunched position so that the weight of the head and shoulder girdle is transmitted through the clavicles and ribs to the sternum. Another set of conditions that must be distinguished from local cervical syndromes consists of tendinopathies affecting the spinous and transverse processes. Here, examination reveals radiating pain that can be reproduced by local pressure and intensified by muscle contraction. The diagnosis can be confirmed by infiltration with local anesthetic.
Acute Torticollis (Wry Neck)
Etiology and Manifestations
 Acute torticollis is a variety of local cervical syndrome characterized by an abnormal posture and restricted mobility of the cervical spine.
Acute torticollis is a variety of local cervical syndrome characterized by an abnormal posture and restricted mobility of the cervical spine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree