Wrist and Hand Pain
|
Red Flag Signs and Symptoms
Any of these signs and symptoms should prompt urgent evaluation and appropriate intervention:
Fevers
Chills
Hot, swollen joint
Progressive neurologic symptoms
Loss of pulses
CARPAL TUNNEL SYNDROME
Background
Carpal tunnel syndrome (CTS) is the most common compressive neuropathy. The carpal bones form the floor and walls of the tunnel, and the rigid flexor retinaculum attaches to the trapezium and scaphoid bones to form the rigid roof. Through this rigid tunnel pass the eight flexor tendons covered in a common sheath as well as the flexor pollicis longus tendon in its own sheath. The median nerve rests superficially just dorsal to the flexor retinaculum. Diabetes mellitus, thyroid dysfunction, pregnancy, rheumatoid arthritis, and other medical conditions predispose to the development of CTS.
Clinical Presentation
Patients typically present with achy pain and numbness that radiates from the wrist into the first three digits and radial side of the fourth digit. It is not unusual for patients frequently to complain of pain and numbness in
the whole hand. Patients may report waking up in the middle of the night with increased symptoms and then shaking the hand to “wake it up,” “get the blood flowing,” and decrease the pain and numbness. Symptoms may be exacerbated during activities such as typing or knitting. In general, activities that require repetitive wrist flexion (typing in a suboptimal anatomic position) or repetitive wrist extension exacerbate symptoms.
the whole hand. Patients may report waking up in the middle of the night with increased symptoms and then shaking the hand to “wake it up,” “get the blood flowing,” and decrease the pain and numbness. Symptoms may be exacerbated during activities such as typing or knitting. In general, activities that require repetitive wrist flexion (typing in a suboptimal anatomic position) or repetitive wrist extension exacerbate symptoms.
|
As the syndrome progresses, symptoms may become more constant. Patients may also note weakness in their grip, including difficulty with activities such as opening jars or buttoning a shirt. They may also report dropping things. Sometimes they perceive this weakness as “clumsiness” in their hands.
Physical Examination
The three classic tests for CTS are the Tinel sign, Phalen test, and carpal compression test. A positive Tinel sign (Fig. 4.1) occurs when repetitive tapping over the median nerve as it
passes through the carpal tunnel elicits symptoms in the median nerve distribution. In the Phalen test (Fig. 4.2), the patient places both wrists in full flexion and juxtaposes the dorsal aspect of each hand against the other. If symptoms are reproduced within 1 minute, the test is positive for CTS. Symptoms typically occur in the first 10 to 20 seconds if the patient has CTS.
passes through the carpal tunnel elicits symptoms in the median nerve distribution. In the Phalen test (Fig. 4.2), the patient places both wrists in full flexion and juxtaposes the dorsal aspect of each hand against the other. If symptoms are reproduced within 1 minute, the test is positive for CTS. Symptoms typically occur in the first 10 to 20 seconds if the patient has CTS.
In the carpal compression test (Fig. 4.3), the physician places steady, firm pressure over the carpal tunnel. If symptoms are reproduced in 30 seconds, the test is considered indicative of CTS.
Patients may report numbness to light palpation over the median nerve distribution in the hand. The thenar eminence should not be numb because the cutaneous branch of the median nerve supplies this region and it branches prior to the carpal tunnel.
In more advanced cases, patients may have wasting of the thenar eminence and/or thenar weakness, which manifests by the patient having difficulty opposing the thumb.
Diagnostic Studies
An electromyelography/nerve conduction velocity (EMG/ NCV) study is the study of choice to distinguish CTS from other pathologies such as a cervical radiculitis or ulnar neuropathy. EMG/NCS also is able to determine the severity of disease. Typically, symptoms correlate with amount of nerve damage. But occasionally a patient with moderate or even mild symptoms may have significant nerve damage when tested with EMG/NCS. This is important to note because it needs to be addressed more urgently or at least needs to be followed more closely. Once the motor nerves are significantly damaged, strength may take a long time to return or may not return. There is debate as to which patients with suspected CTS should receive an electrodiagnostic study. Certainly, any patient considering surgery would benefit from EMG/NCS. Some physicians believe that most, if not all, patients with CTS should receive EMG/NCS both to document the severity of disease and to note which patients need closer
following and/or more aggressive intervention because of nerve damage.
following and/or more aggressive intervention because of nerve damage.
Recent studies have shown that the use of ultrasound for the assessment of the median nerve may be a promising noninvasive imaging study. With the use of ultrasound the edema of the median nerve is assessed. EMG/NCS still remains the standard for diagnosing median nerve pathology.
Treatment
In mild cases a resting wrist splint used at night to keep the wrist in the neutral position may be sufficient. While sleeping, people have a tendency to flex their wrists, placing stress on the nerve in the tunnel. In the case of CTS, this may add constant irritation to the nerve and slow healing.
A short course of nonsteroidal anti-inflammatory drugs may also be helpful. In addition, patients should undergo a short course of occupational (or physical) therapy. In therapy, patients should work on ergonomics education, postural mechanics, strengthening exercises, and tendon gliding exercises. In the acute phase, ice can be used to help reduce inflammation. In addition, a workplace assessment (or education about workspace adjustments) is critical to ensure that repetitive stresses aren’t being placed on the carpal tunnel daily.
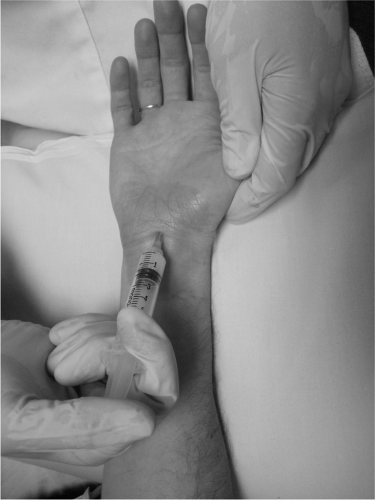
If the symptoms are more constant and/or bothersome to the patient, an effective treatment is a steroid and anesthetic injection into the carpal tunnel (Fig. 4.4), which may speed recovery. Ultrasound guidance may help with injection accuracy.
CARPAL TUNNEL INJECTION
After informed consent is obtained, identify the carpal tunnel. The authors favor using a 25-gauge, 1.5 inch needle, 40 mg of triamcinolone acetate, and 1 mL of 1% lidocaine. Mark a spot in the middle of the proximal wrist crease. Sterilize this area using three iodine swabs and an
alcohol pad. Using sterile technique, aim the needle at a 45-degree angle to the tunnel and inject distally. Always aspirate before injecting. If blood is found in the aspirate, reposition. There should be no aspirate in this injection. If resistance is felt, do not inject. Resistance could indicate that the needle is in a tendon. Never inject directly into a tendon. Reposition and aspirate again. When there is no aspirate and the injectate flows smoothly, inject. Clean the iodine off with alcohol pads.
alcohol pad. Using sterile technique, aim the needle at a 45-degree angle to the tunnel and inject distally. Always aspirate before injecting. If blood is found in the aspirate, reposition. There should be no aspirate in this injection. If resistance is felt, do not inject. Resistance could indicate that the needle is in a tendon. Never inject directly into a tendon. Reposition and aspirate again. When there is no aspirate and the injectate flows smoothly, inject. Clean the iodine off with alcohol pads.
For more constant symptoms, the wrist splints can be used more frequently.
If conservative care is not effective, surgical release of the tunnel may be needed.
Of note, if a pregnant patient develops CTS, the symptoms may resolve spontaneously postpregnancy.
If a patient has an underlying untreated condition causing the CTS (e.g., hypothyroidism) it is of course critical to treat it. Treatment of the underlying condition may alleviate the CTS symptoms as well.
DE QUERVAIN TENOSYNOVITIS
Background
De Quervain tenosynovitis is an inflammation of the tendons in the first dorsal compartment of the wrist. These tendons are the abductor pollicis longus (APL) and extensor pollicis brevis (EPB). They can be remembered by the mnemonic “All peanut lovers (APL) eat peanut butter (EPB).” De Quervain tenosynovitis can be caused by repetitive microtrauma or, less commonly, a sudden trauma to the tendons.
Clinical Presentation
Patients complain of pain localized to the dorsolateral aspect of the wrist over the radial styloid. The pain is classically exacerbated by movements of the thumb. A detailed history often reveals the patient has begun a new activity that involves repetitive thumb use. For example, the patient may be a young mother who has been repetitively picking up her newborn. Other common causes include taking on a new hobby such as knitting, golf, computer use, or gardening. These activities exacerbate the pain. Sometimes, there is mild swelling over the painful area.
Physical Examination
Note any swelling over the first dorsal compartment of the wrist. The Finkelstein test should be performed. In this test, the patient makes a fist with his thumb fully flexed
under his four fingers. The physician then passively applies an ulnar deviating force to the wrist. This test may be “positive” in many asymptomatic people. So it is important to ensure the test reproduces the patient’s typical symptoms to consider the test positive. In addition, the asymptomatic side should be tested.
under his four fingers. The physician then passively applies an ulnar deviating force to the wrist. This test may be “positive” in many asymptomatic people. So it is important to ensure the test reproduces the patient’s typical symptoms to consider the test positive. In addition, the asymptomatic side should be tested.
Diagnostic Studies
No imaging studies are routine for this condition. They should be ordered to rule out other pathologies (such as may be the case with an acute injury to the tendons precipitating symptoms to rule out fracture).
Treatment
Initial treatment consists of the patient using a thumb spica splint. This splint immobilizes the thumb and wrist. Ice may also be used as an excellent anti-inflammatory agent in this area. The patient may benefit from a short course of occupational therapy.
If symptoms are severe or the patient’s symptoms persist despite 2 to 3 weeks of more conservative therapy, an injection into the tendon sheath may be performed (Fig. 4.5). As always, it is important not to inject directly into the tendon itself. Ultrasound can be used to help with visualization of the injection. In addition to the usual risks of injection (e.g., infection, bleeding, allergic reaction, tendon weakening, transient elevation of blood glucose), because of the location of the injection there is a risk of skin hypopigmentation (related to the superficiality of the injection). Subcutaneous atrophy has been reported to (very rarely) extend through the lymphatics more proximally in the forearm and cause injury to the radial sensory nerve. Injury to the radial sensory nerve may result in anesthesia over the first web space of the dorsal hand and dorsal thumb. This generally resolves within a few hours. Rarely, if the radial nerve is severely injured by direct needle penetration, persistent pain may result in the superficial radial nerve distribution.
In severe recalcitrant cases, surgical decompression of the first dorsal compartment may be necessary.
DE QUERVAIN TENOSYNOVITIS INJECTION
After informed consent is obtained, identify the point of maximal tenderness along the tendon sheath of the abductor pollicis longus and extensor pollicis brevis. The authors favor using a 25-gauge, 1.5 inch needle, 20 mg of triamcinolone acetate, and 1 mL of 1% lidocaine. Mark a spot approximately 3 cm distal to the point of maximal tenderness. Sterilize this area using three iodine swabs and an alcohol pad. Using sterile technique, aim the needle at a 30-degree angle to the tendon and inject proximally. Always aspirate before injecting. If blood is found in the aspirate, reposition. There should be no aspirate in this injection. If resistance is felt, do not inject. Resistance could indicate that the needle is in the tendon. Never inject directly into a tendon. Reposition and aspirate again. When there is no aspirate and the injectate flows smoothly, inject. Clean the iodine off with alcohol pads.
FIRST CARPOMETACARPAL JOINT ARTHRITIS (BASE OF THUMB ARTHRITIS)
Background
The first carpometacarpal (CMC) is the hand joint most commonly affected by osteoarthritis. It is an idiopathic condition that occurs primarily in women older than 40 years. Rheumatoid arthritis may also affect this joint (although there are usually systemic symptoms and bilateral involvement of the joints).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree