Wrist and Hand
Epidemiology
Overall, wrist and hand injuries account for between 3-9% of all sports injuries.
Incidence varies between sports, with up to 87% of gymnasts reported to experience wrist pain during their career, due to the wrist being a weight-bearing joint in many of the activities of this sport.
Hand injuries account for 44% of all injuries in rock climbing.
Injuries to the hand and wrist are common in tennis and golf (especially the left hand in right-handed golfers).
The majority of injuries are soft tissue, but a diagnosis of ‘wrist sprain’ should only be made by exclusion of other more serious injuries.
Hand and wrist injuries are more common in children, and may involve the epiphyseal plates with the potential for growth disturbance.
Wrist biomechanics
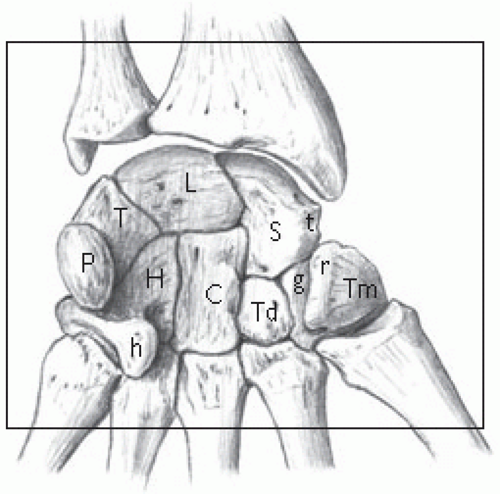
See Fig. 19.1 for an anterior view of the carpal bones.
Normal daily activities require 30° of extension, 5° flexion, 10° radial deviation, and 15° of ulnar deviation.
Throwing requires a similar degree of extension and radio-ulnar deviation, but flexion is increased to 80-90° at the end of the acceleration phase prior to ball release.
Studies of the golf swing have shown a flexion-extension arc of 103° in the right wrist compared with 71° in the left wrist for right handed players (advanced players show less movement at the left wrist but more at the right).
With an intact triangular fibrocartilage complex (TFCC), the radius bears 82% and the ulna 18% of the force during axial loading of the wrist.
This pattern of force transmission can be altered in sports such as gymnastics, where a significant load can be applied to the ulnar side of the wrist.
Excision of the TFCC increases the load on the radius to 94%.
Ulnar shortening (negative ulnar variance) of 2.5mm reduces the ulnar load bearing to 4%, while lengthening by 2.5mm increases it to 42%.
Fracture of the distal radius/ulna (Colles’ fracture)
History and examination
Common in the elderly athlete (approximately 7% of all Colles’ fractures occur during sport) and are caused by a fall on the outstretched hand.
Fractures in the younger athlete may be accompanied by intra-articular injury and warrant careful assessment.
Dorsal angulation and impaction leads to the classic ‘dinner fork’ deformity.
May involve the epiphyseal plate in children (especially distal radius) and careful follow up is required to ensure that premature growth arrest does not occur (see also ‘The Paediatric Wrist’, p. 544).
Investigation
Diagnosis confirmed by X-ray.
Treatment
Accurate closed reduction and cast immobilization for 6-8 weeks with regular review to ensure that a satisfactory position is being maintained. Physiotherapy to restore range of movement should be started following removal of cast.
Any intra-articular involvement in the young athlete should be treated by open reduction and internal fixation to restore joint congruity.
Fracture of the scaphoid
History and examination
Caused by a fall onto the outstretched hand and, therefore, common in football, basketball, hockey, and rugby. These injuries may also occur in boxing.
Clinical findings include tenderness in the anatomical snuff box (always compare with the uninjured side) and over the palmar scaphoid.
There will be pain when an axial load is applied to the first metacarpal.
Common in sport and are important not to miss, as they have the potential for delayed or non-union, with subsequent avascular necrosis and long-term disability.
Investigations
Treatment
Fractures with a good potential to heal include incomplete, undisplaced fractures, and those involving the distal scaphoid.
Treatment is immobilization in a scaphoid cast for a period of 8-12 weeks (average time to union 9½ weeks). Physiotherapy should be commenced immediately post-immobilization to restore range of movement and function.
Those requiring surgery include displaced or proximal pole fractures and those with greater than 15° of angulation.
Non-union occurs in approximately 10-15% of cases—this complication is preventable by early recognition and appropriate treatment.
A diagnosis of a ‘sprained wrist’ can only be made by exclusion, and it is much better to err on the side of caution and immobilize all cases of suspected scaphoid fracture, even if the initial X-rays are negative.
Fracture of the hamate
History and examination
These fractures occur in racquet sports and golf, caused by the butt of the racquet or golf club forcibly impacting on the hypothenar eminence and hamate hook. In golf may be due to the club being gripped too close to the butt.
Fractures of the hook of the hamate comprise 2-4% of all carpal fractures. Stress fractures have been described in some sports, e.g. baseball.
Injury to the ulnar nerve may occur in this area and cause the patient to present with numbness and paraesthesia or weakness of the ulnar innervated muscles, as well as pain and tenderness to direct palpation.
Investigation
Diagnosis is confirmed on CT scan—fractures of the hamate are difficult to see on plain X-rays.
Treatment
Non-displaced fractures are treated conservatively with cast immobilization for 4-6 weeks.
Displaced fractures require open reduction and internal fixation, or excision of the fractured hook.
Fracture of the pisiform
History and examination
The pisiform may occasionally be fractured by a direct blow.
Treatment
Treatment is excision with preservation of the flexor carpi ulnaris tendon.
Fracture of the metacarpal bones
History and examination
Fractures of the neck of the 5th metacarpal are common in combat sports (hence, the term ‘boxer’s fracture’).
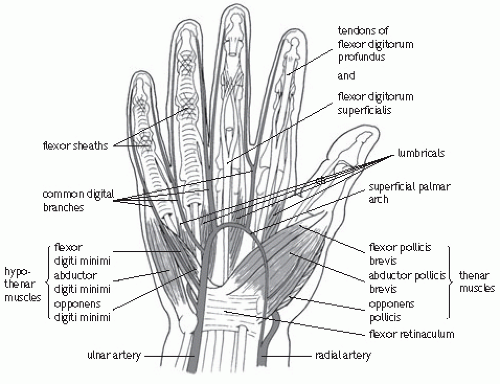
See Fig. 19.2 for anatomy.
Investigations
X-ray: fractures of the metacarpal bones may be transverse, oblique, or comminuted.
It is important to check for malrotation (best observed by asking the patient to make a clenched fist).
Treatment
Non-displaced fractures should be treated conservatively with cast immobilization—any displacement should be managed surgically.
Return to sport depends on the need for hand function, but can be expected after approximately 2 weeks in stable, non-displaced fractures.
Angulation is common, but if greater than 60° then the fracture should be reduced and immobilized in a metacarpal splint.
Shortening may occur and percutaneous pinning should be considered in the competitive boxer.
Bennett’s fracture
A fracture/dislocation of the base of the first metacarpal.
The pull of abductor pollicis longus causes displacement of the metacarpal shaft.
Treatment is by closed or open reduction and pinning, followed by 4-6 weeks cast immobilization.
A further period of splinting is necessary on return to sport.
Phalangeal fractures
It is very important to check for malrotation (most common in spiral fractures of the proximal phalynx)—ask the patient to make a clenched fist and any rotational deformity should become obvious.
Also assess for any tendon or volar plate injury.
Stable fractures can be managed conservatively by ‘neighbour’ splinting for 3-4 weeks, but careful follow up of all injuries is advised to ensure return of full function.
Dislocation of the carpal bones
History and examination
Acute dislocations of the lunate may occur following a fall.
The lunate dislocates anteriorly and may cause compression of the median nerve.
More common than an acute dislocation is the development of scapholunate dissociation following a tear of the scapholunate ligament.
There is tenderness over the radial side of the lunate and Watson’s test will be positive (pressure over the scaphoid tuberosity as the wrist is moved from ulnar to radial deviation will result in the scaphoid being felt to sublux dorsally).
Investigation
A clenched fist postero-anterior (PA) X-ray will demonstrate a gap between the scaphoid and the lunate in cases of scapholunate dissociation (the ‘Terry Thomas’ sign).
Treatment
Treatment of lunate dislocation is by open reduction and repair of the torn ligaments followed by eight weeks cast immobilization.
Treatment of dissociation following a tear is surgical with open reduction internal fixation (ORIF) and repair of the damaged ligament.
Dislocation of the 1st metacarpophalangeal joint
Investigation
X-ray.
Treatment
This requires open reduction as the metacarpal head becomes button holed between the lumbrical and long flexor tendons.
Following reduction a splint should be worn to prevent the terminal 30° of extension at the MCP joint for 6 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree