Abstract
Objective
Evaluate the place and level of proof of physical therapeutics for treating neuropathic pain in spinal cord injury (SCI) patients.
Method
Literature review from three databases: PubMed, Embase, Pascal. The following keywords were selected: chronic neuropathic pain/non-pharmacological treatment; transcutaneous electrical nerve stimulation, physiotherapy, acupuncture, physical therapy, transcranial magnetic stimulation, heat therapy, ice therapy, cold therapy, massage, ultrasound, alternative treatment, complementary treatment, occupational therapy. The articles were analyzed using the double-reading mode.
Results
Three techniques emerge from the literature: magnetic or electrical transcranial stimulation, transcutaneous electrical nerve stimulation and acupuncture. Even though the first method is not easily accessible on a daily basis it is the one that yields the most promising results validated by Grade B studies. Healthcare professionals remain faithful to pain-relieving transcutaneous neurostimulation for both segmental neuropathic pain and below-level central neuropathic pain. Acupuncture is advocated by Canadian teams and could offer some interesting options; however, to this day, it does not have the methodological support and framework required to validate its efficacy. All other physical therapies are used in a random way. Only below-level massages are advocated by the patients themselves.
Conclusion
To this day, no study can validate the integration of physical therapy as part of the array of therapeutics used for treating neuropathic pain in SCI patients. In the future, it will require controlled and randomized therapeutic studies on homogenous groups of SCI patients, to control the various confusion factors.
Résumé
Objectif
Étudier la place et le niveau de preuve des thérapies physiques dans le traitement des douleurs neuropathiques chez le blessé médullaire.
Méthode
Revue de la littérature à partir de trois bases de données : PubMed, Embase, Pascal. Les mots clés suivants ont été choisis : chronic neuropathic pain/non-pharmacological treatment ; transcutaneous electrical nerve stimulation, physiotherapy, acupuncture, physical therapy, transcranial magnetic stimulation, heat therapy, ice therapy, cold therapy, massage, ultrasound, alternative treatment, complementary treatment, occupational therapy . Les articles ont été analysés en double lecture.
Résultats
Trois techniques dominent la littérature : la stimulation magnétique ou électrique transcrânienne, la neurostimulation transcutanée antalgique et l’acupuncture. Si la première est d’application difficile au quotidien, c’est celle qui offre les résultats les plus prometteurs, soutenus par des études de grade B. Les professionnels de santé restent attachés à la neurostimulation transcutanée antalgique aussi bien pour les douleurs lésionnelles que sous-lésionnelles. Quant à l’acupuncture, promue par les équipes canadiennes, elle offre des promesses d’efficacité sans bénéficier, pour l’instant, du support méthodologique qui s’impose. Toutes les autres thérapies physiques sont utilisées de manière aléatoire. Seuls les massages en territoire sous-lésionnels sont défendus par les patients eux-mêmes.
Conclusion
Aucune étude ne permet à ce jour d’inscrire une quelconque thérapie physique dans l’arsenal du traitement des douleurs neuropathiques du lésé médullaire. La nécessité d’essais thérapeutiques contrôlés et randomisés, sur des groupes homogènes de patients lésés médullaires, maîtrisant les nombreux facteurs de confusion est une exigence pour années futures.
1
English version
1.1
Introduction
Physical therapy is an entity with a badly defined and non-consensual framework. It involves medical and physiotherapy teams. Largely based on experience, it encompasses a group of techniques with a therapeutic aim based on physical contact using tactile stimuli, electrical or magnetic stimulation.
For pain-relieving treatment, physical therapies are based on joint mobilization and massages as well as electrophysiotherapy. The latter combines transcutaneous electrostimulation (TENS), cold or hot applications, thermotherapy, electrotherapy, electromagnetic waves therapy, laser phototherapy, vibrations, ultrasound therapy.
For spinal cord injury (SCI) patients, their daily routine leaves very little room for physical therapy in treating their central neuropathic pain.
The aim of this literature review is to assess the real place of these therapies within the therapeutic array available for treating central neuropathic pain in chronic SCI patients.
1.2
Methods
1.2.1
Material
The inclusion criteria for the selected studies reviewed are based on the Sofmer recommendations . For the selected studies, we gave priority to clinical studies free or controlled (randomized or not) as well as synthesis articles (meta-analysis and literature review). The targeted population is mainly an adult SCI population. Publications regarding non-traumatic SCI patients, when they were associated in the same cohort with traumatic SCI patients were also included.
The exclusion criteria included all experimental or fundamental studies (mainly neurophysiological) since our aim was to focus our literature review on clinical practice recommendations. The studies on children were also excluded. Articles that were too general and only reported physical therapies in a descriptive or qualitative manner as well as articles focusing on above-level neuropathic pain with a musculoskeletal predominance were also excluded.
1.2.2
Bibliographical research modalities
The selection criteria common to all publication is the variable “physical therapy”. To the physical therapy definition mentioned above, we have associated acupuncture and transcranial magnetic cortical stimulation (TMS).
Keywords used were:
- •
in English: chronic neuropathic pain/SCI/human/adult/non-pharmacological treatment, transcutaneous electrical nerve stimulation, physiotherapy, acupuncture, hypnosis, physical therapy, transcranial magnetic stimulation, self management approaches.
The following keywords were associated to those recommended by the scientific committee: heat therapy, ice therapy, cold therapy, massage, ultrasound, alternative treatment, complementary treatment, occupational therapy.
- •
in French: douleur neuropathique chronique/blessé médullaire traumatique/humain/adulte/traitement non pharmacologique/stimulation nerveuse périphérique/physiothérapie/TENS/acupuncture/hypnose/kinésithérapie/stimulation magnétique transcrânienne .
The following keywords were also associated to those recommended by the scientific committee: thermothérapie chaude, thermothérapie froide, massage, ultrasons, traitements alternatifs, traitements complémentaires and ergothérapie .
We also conducted a search on each consulted publication’s bibliography. In the same way, the Pubmed weblinks were also searched. The results of these researches were added to those obtained by the scientific committee.
During our second lecture, we discarded hypnosis and self-management techniques as they are not listed as part of the array of physical therapies but rather belong to behavioral therapies and therapeutic learning.
1.2.3
Identification modalities for common professional practices
These practices were selected by specialists through a vote that took place during the Experts Conference and via Internet. Specialists had to vote on two questions:
- •
which of the following physical therapy (one or more) would you prescribe for treating chronic below-level central neuropathic pain?
- •
which of the following physical therapy (one or more) would you prescribe for treating chronic segmental pain (at injury level)?
The potential answers were:
- •
pain relief transcutaneous neurostimulation;
- •
acupuncture;
- •
electrical or magnetic transcranial stimulation;
- •
thermotherapy;
- •
massage;
- •
electrotherapy;
- •
vibrations;
- •
electromagnetic waves;
- •
ultrasounds;
- •
other;
- •
none.
1.3
Results
The bibliographical search conducted by the scientific committee found 71 articles. The full-text analysis, the analysis of the references of the selected articles as well as personal research led to isolating 39 articles that met the above-mentioned inclusion criteria.
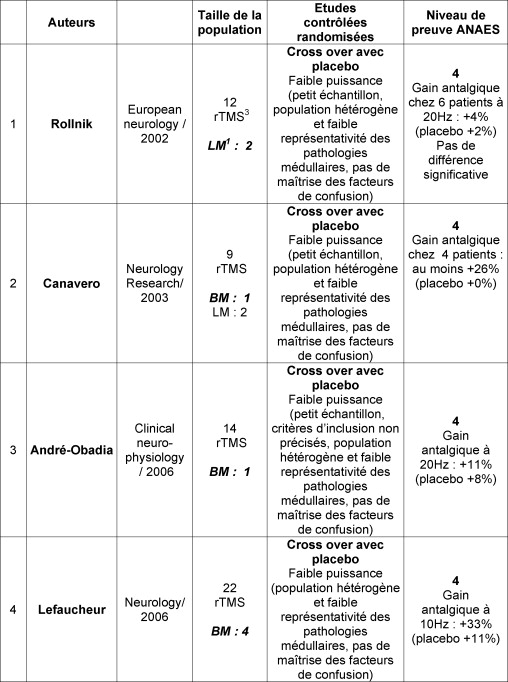
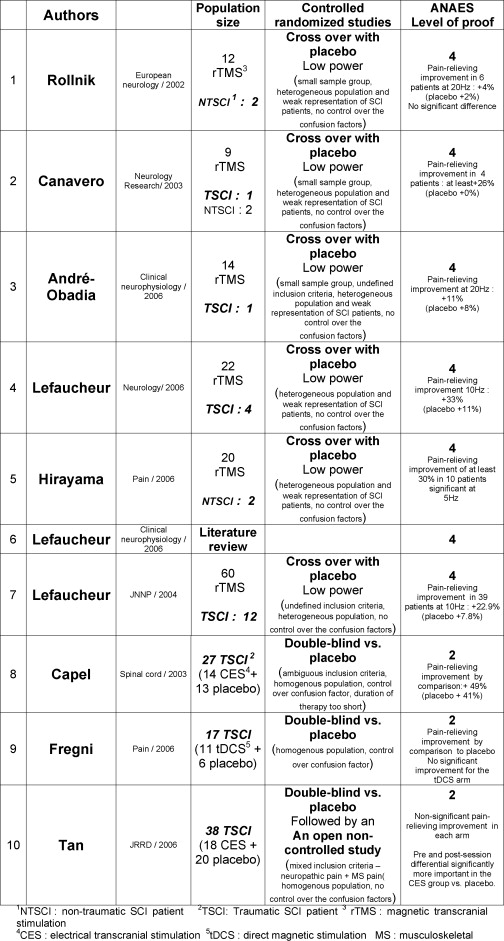
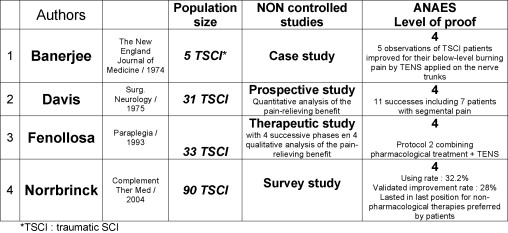
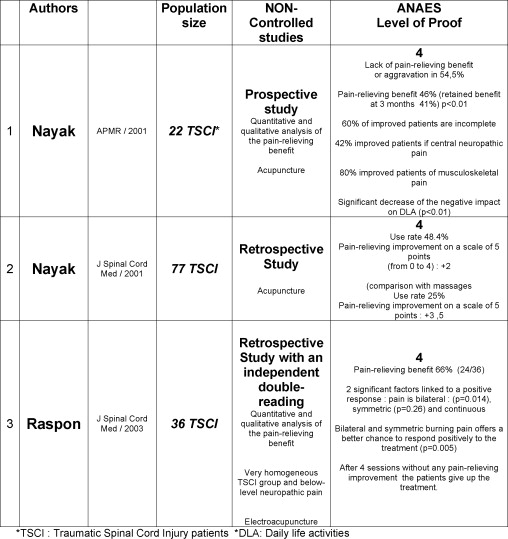
The final selection combined methodological criteria-controlled study, randomized vs. placebo or crossover study or non-randomized study, cohort size criteria or singularity of the obtained results. Finally, 17 studies made the final cut. Ten studies directly focused on magnetic or electrical transcranial stimulation ( Fig. 1 ), four studies were on pain-relieving transcutaneous neurostimulation ( Fig. 2 ), and three on acupuncture ( Fig. 3 ). The presentation in each table lists the cohort size, study methodology, control level for the confusion factors and level of scientific proof. The other physical therapies were only brought up, in an anecdotic manner, in so-called “general” articles on neuropathic pain in SCI patients. An inadequate or even lack of methodology and/or the lack of references to a therapeutic study and/or a very small sample group of patients did not yield any article on all other physical therapies.
No discordance was noted between the two experts for establishing the level of scientific proof. In spite of their rigorous clinical study methodology, some articles were downgraded from level 2 to level 4 due to major biases among which we find the weak representation of SCI patients within an heterogeneous group of patients and not taking into account the confusion factors .
Only one literature review was selected because it was conducted by one of the most specialized team in this field of expertise .
For pain-relieving transcutaneous neurostimulation, the dearth of publications combining “neuropathic pain” and “SCI patients” led to keeping only articles that strongly suggested a therapeutic impact either because the number of included patient was high, or because the effects were spectacular for some patients.
Regarding professional practices, 166 individuals (116 who attended the Experts Conference and 50 who answered via Internet) gave their opinion on using physical therapy for treating chronic neuropathic pain ( Appendix 1 ). The answers highlighted the predominance of pain-relieving transcutaneous neurostimulation as the main option for treating below-level central neuropathic pain and segmental neuropathic pain (at the level of injury).
1.4
Discussion
1.4.1
Magnetic and electrical transcranial stimulation
Six controlled studies, randomized, in “crossover”, stimulation vs. placebo and three other double-blind vs. placebo as well as a complete literature review focused on this topic for SCI patients ( Fig. 1 ). Three studies emerge from the group because they were conducted on relatively important sample groups of SCI patients .
The first one comes from the French team most specialized in this field . It is a controlled, randomized, crossover (rTMS vs. placebo) study reporting the impact of rTMS on neuropathic pain refractory to a pharmacological treatment. The sample group was made up of 60 patients suffering from refractory chronic unilateral pain including 12 SCI patients. They benefited from rTMS stimulation (10 Hz) – two successive sessions separated by a 3-week rest period – their pain was assessed using a visual analog pain scale (VAS) before stimulation and at 5′ and 20′ after stimulation. The improvement was obvious for 39 patients, estimated at + 22.9% (7.8% for the placebo group). The worst result was obtained in the ischemic stroke patients group but the “SCI” group was not correctly singled out in terms of pain-relieving efficacy. No comment was formulated on the postsession lingering effects. Finally the study is also biased by unspecified inclusion criteria, a heterogeneous population and the lack of control over the confusion factors.
The second publication is also a controlled, randomized vs. placebo, double-blind study and focused on the impact of cortical electrical stimulation (CES) on the neuropathic pain of 27 SCI patients divided in two arms: one arm of 14 SCI patients benefiting from CES 2hrs × 2 per day for 4 days and an arm of 13 SCI patients receiving a placebo stimulation 2 h × 2 per day for 4 days.
The relevance of this study was a survey of all potential confusion factors by assessing: first the level of pain using a VAS and the McGill Pain Questionnaire (MPQ), then the psychological factors with the anxiety score, the Beck Depression Inventory (BDI) and personality tests and finally the neuroanalgesics medication consumption and hormonal dosages.
Before stimulation, no significant pain difference was noted between the two arms. The active arm reports a decrease in the pain intensity and analgesics pain-relief medication consumption during and immediately after CES. The placebo arm does not report any changes. An 8-week wash-out period was enforced before the two arms could benefit again from CES stimulation 2 h × 2 per day for 4 days. The patients from the initial placebo arm revealed a more significant improvement after this second stimulation therapy. In both cases, no correlation was found between mood evolution and pain evolution, meaning that the pain-relieving impact of the stimulation does not have any functional support. Finally, hormonal and metabolic changes do not differ in any point from those of the control group.
The inclusion criteria in this study are ambiguous – apparently, we are faced with different types of pain (neuropathic pain, musculoskeletal pain). The session length is relatively long (4 h) but the protocol duration, comparatively, is very short (4 days).
Lastly, a recent publication is reported by Tan et al. . It is a controlled, randomized, double-blind vs. placebo study followed by an open, non-controlled study on the efficacy of CES on neuropathic pain in SCI patients. In that case, the electrical current is transmitted by ear electrodes in 38 adult SCI patients with an initial injury dating back at least 6 months. Patients were suffering from chronic neuropathic pain for at least the past 3 months and the intensity is reported with a VAS greater than 6/10. The active arm benefits from CES stimulation for 1 hour per day at a minimum threshold of 100 μA during 21 days. Secondly, all patients were invited to participate in an open study based on CES stimulation of 1 hour per day with a recording of the pain level before and after each daily session. The patients were allowed to adjust the current intensity without increasing its level.
Out of the 38 patients, 18 were included in the CES arm (12 suffering from neuropathic pain and musculoskeletal pain) and 20 in the placebo arm (11 suffering from neuropathic pain and nine from musculoskeletal pain). Before and after inclusion, the participants from the two arms could not be significantly differentiated in terms of pain. However, in the CES arm, the improvement in pain intensity before and after the treatment was more important than in the placebo group. This improvement is quite significant. It is immediate and not validated over time.
Among the 20 placebo arm patients, 17 integrated the open study and 17 reported an improvement. The pain intensity decrease is recorded as 0.73 ± 1.15 vs. placebo (0.08 ± 0.38). Nothing is said about the postsession lingering effects. During the open study, the pain-relieving efficacy is found at a lesser degree in all patients included (decrease of 0.46 ± 0.38). This study’s methodology suffers from a bias frequently found in this type of study : mixed inclusion criteria (neuropathic pain, musculoskeletal pain) and sometimes a lack of sufficient control over the various confusion factors. However, at this stage we can admit that cortical stimulation has a real potential pain-relieving efficacy. For the authors, the most sensitive profile would be the non-traumatic SCI patient with a low level of injury or an incomplete injury and finally with a weak to moderately intense neuropathic pain. The pain-relieving effects remain quite short lasting and the relationship between the stimulation intensity and the pain-relieving effects has still not been clearly demonstrated.
1.4.2
Transcutaneous electrostimulation
Four publications dominate the literature without offering a sufficient level of proof to validate the use of TENS for treating neuropathic pain in SCI patients.
The first one dates back to 1974 and is relevant for three reasons:
- •
it is the first publication on this topic;
- •
it was published in a widely distributed scientific journal;
- •
the impact of TENS on below-level central neuropathic pain spectacular.
In reality, we are faced with a simple letter reporting the case of five SCI patients suffering from below-level central neuropathic pain. The pain-relieving transcutaneous neurostimulation is applied on the nerve pathway deserving the painful areas. The pain-relieving effect on the below-level neuropathic burning pain was complete for all patients and lasted for 8 to 10 h.
It is however another publication from Davis and Letini that emerges as the first large SCI cohort included in a prospective study but not controlled. This article is a reference since it is listed in almost all articles focusing on TENS in SCI patients in spite of its methodological faults. The target population is made up of 31 SCI patients taking neuroanalgesics medication. Twenty-four patients have a type 1 unequivocal pain (segmental pain – transitional zone pain) or type 2 (radicular pain) or type 3 (below-level central neuropathic pain). Seven patients accumulated type 2 and 3 pain. The neurostimulation is applied on the painful areas during 1 month; at the end of this stimulation course, the authors reported 18 failed cases out of 31 patients (no improvement in pain intensity or neuroanalgesics consumption). We find two partially successful cases yet insufficient to motivate the patients to use TENS and 11 completely successful cases for type 1, 2 or 3 pain with a clear majority of patients with type 1 pain (seven cases of 11 successful cases). Nothing is reported on the long-term effect or benefit–risk ratio.
All the other articles dealing with TENS are based on questionnaires and surveys. For example, we found a large cohort survey study on the use of non-pharmacological treatments for treating all types of pain in SCI patients . The study evaluated how many patients used or were still using non-pharmacological treatments and what were their efficacy. It also aims to identify the characteristics for the population not using non-pharmacological treatments.
Out of 123 questionnaires sent to SCI patients, 100 were analyzed. Ten percent of patients reported that they were not suffering from neuropathic pain and thus were excluded from the study. Ninety patients were included and they reported nociceptive, neuropathic or mixed pain.
Of patients, 63,3% used at least one of the following non-pharmacological treatments: TENS, acupuncture, massage, thermotherapy, mental imagery and physical training; 35.6% used acupuncture with an efficacy validated by 28% of patients; 34.4% and 32.2% used, respectively, massages and TENS with an efficacy validated, respectively, by 87% and 28% of them; 24.4% used hot thermotherapy and 77% validated its improvement on their pain.
Thus the techniques deemed the most efficient are massages and hot thermotherapy but the patients’ preference goes to, in decreasing order, pain-relieving drugs, hot thermotherapy, physical therapy, massages, mental imagery, sleep, acupuncture and TENS. The authors reported no difference between the two sexes.
The predictive factors for using pharmacological treatments are the following: high intensity of the pain, muscular aches, sharp stabbing-like pain. A profile for the improved patients could not be established due to the weak sample groups of patients.
According to the literature and the results of this questionnaire, the author suggest that massages, hot thermotherapy, TENS and acupuncture should be used until their efficacy is validated.
Associating a pharmacological treatment to non-pharmacological therapies is highly recommended. The positive impact of pharmacological treatments on the patients’ sleep and psychological state is strongly suggested by several studies. The tendencies reported in this survey justify their integration in future randomized controlled studies.
Finally, a publication adopted a mixed, “step-by-step” approach, combining a pharmacological treatment and physical therapy by TENS . Thirty-three SCI patients with chronic pain were included in a four-phase study. The four phases were conducted successively until an efficacy to the administered protocol was reached:
- •
amitriptyline + clonazepam + non-steroidal antiinflammatory drugs (NSAID);
- •
amitriptyline + clonazepam + 5-OH tryptophane + TENS;
- •
amitriptyline + clonazepam + spinal cord stimulation;
- •
intrathecal morphine delivery.
The time length of the TENS sessions introduced at phase 2 varied from 3 to 6 h per day. The mandatory rest interval between each phase went from 15 to 90 days (mean 35 days). The phase 2 generated the most improvements among the studied population (16 patients). Of course, this study, itself, only suggest the hypothesis of the pain-relieving impact of TENS on segmental deafferentation pain in SCI patients without validating the results.
1.5
Acupuncture
We found only non-controlled, prospective or retrospective studies coming from two different authors and dominated by two techniques: Nayak et al. (regular acupuncture) and Rapson et al. (electroacupuncture).
The only prospective study is Canadian . It is a non-controlled study on the efficacy of acupuncture on chronic pain in SCI patients and thus on their physical and social behavior as well as their mood and psychological state. The study also aimed to identify the predictive factors for a positive response to acupuncture in 31 SCI patients with an injury dating back at least 6 months who report a pain intensity above or equal to 5/10 for at least the past 6 months. The treatment was administered during 7,5 weeks over 15 sessions and the multidimensional evaluation associated a numeric rating pain scale, a global medical check up, an overview of the patients’ social activities, mood assessment, psychological check-up as well as an evaluation the patients well-being and their expectations regarding the treatment.
This evaluation was done prior to the treatment ( t 0 ), during the treatment ( t 0 + 7,5 weeks), after treatment ( t + 15 weeks) and ( t + 28 weeks). Among the 31 patients included, 22 completed the study. The mean time since injury was estimated at 8,49 years and mean duration of pain at 8,46 years. The decrease in pain intensity is significant and lingers on for 3 months. Eighteen percent of patients reported a decrease of more than 3 points on the numeric rating scale (NRS), 27% between two and three points, 37% between zero and two points and 18% report a pain increase.
Overall, almost 54,5% of patients (i.e., 12 patients) judged acupuncture useless or with a minimal or even worsening action on their pain. But, 46% of patients benefited from this treatment and for 41% of them the positive impact lasted up to 3 months ( p < 0.01). However, in this group, the patients with below-level central neuropathic pain did not respond positively to the treatment ( p < 0.01). No significant clinical or demographical difference distinguishes the improved group from the non-improved group.
This study suggests that the incomplete patients (60% of surveyed patients) are more likely to belong to the improved group. (33% in complete patients) and the best response level is obtained for musculoskeletal pain (42% of surveyed patients) rather than below-level central neuropathic pain. The only significant difference observed between the improved and non-improved group is the level of pain intensity before treatment. The best results were for patients with a low intensity pain. There are no reported significant changes on the patients’ mood, anxiety level or depressive state. Finally, the negative impact of pain on daily life activities significantly decreases in the improved group after treatment ( p < 0.01). The lack of a control group makes it impossible to discard the placebo effect.
Two retrospective studies are associated to this first publication they are both selected for our review since the first one is based on a cohort of 77 SCI patients and the second one is conducted with a strict methodology and an independent double-reading of the results.
The first one is a retrospective study on the framework and guidelines for complementary and alternative medicine (CAM) used for treating chronic pain in SCI patients .
From an initial sample group of 135 patients, 77 SCI patients were contacted by phone (response rate 57%). Among these patients, 15 had already been involved in a therapeutic clinical study on acupuncture but no demographical and clinical data could differentiate them from the other 62 patients. The phone conversation focused on demographics, type of pain and duration of pain, use of conventional therapies as well as CAM during the survey or prior to it, the reasons for selecting CAM, the cost of these therapeutics, the insurances financial support, the type of CAM and their treatment details (duration, frequency, benefit received, adverse events).
Forty-three patients (56%) had already benefited from CAM (25 had given up at the time of the survey, 18 were still involved in CAM). Among these 43 patients, we account for 1 patients included in the acupuncture clinical study, but for 12 of these 15 patients, it is their first and only CAM experience. No differences were reported regarding sex, ethnic origin, age or educational level between users and non-users. No difference was reported in terms of pain severity. We can differentiate the users through some characteristic traits, better income, the time since injury is longer and their pain is twice more important than others. The time spent on CAM varies from 4 to 18 months (mean 3,64 years). Most patients have been users for the past 1 to 2 years. Among the users, the reasons for turning to CAM were, in decreasing frequency order, inefficacy of conventional treatments (88,9%), the desire for a treatment taking into account the relationships between mind, body and soul (66,7%), the desire to better control their therapeutic care (55,6%), the desire to explore all existing therapeutic possibilities (38,9%), recommended by a physician. Among the non-users, the reasons for not using CAM were, in decreasing frequency order: never considered CAM as a valid therapeutic option (41,2%), no easy access to CAM or no info on CAM (14,7%), unable to afford CAM (11,8%), not reimbursed by their medical insurance (8,8%), physician did not recommend CAM (8,8%), does not believe in CAM (8,8%). Among the users who gave up CAM, the reasons for giving up were, in decreasing frequency order: inefficacy of CAM, unable to continue affording CAM, not reimbursed by medical insurance, no noticeable improvement. The demographical and clinical data analysis was done by logistical regression. It appears that only the age of the injury and the use of conventional pharmaceutical treatments are predictive factors for using CAM.
Meaning that, for each additional decade, the odds of turning to CAM are three times more important. Those who never used conventional medications are 6,5 times more likely to turn to CAM.
Among the users, the wide use of conventional pharmaceutical drugs is a predictive factor for a scale-down use of CAM.
The CAM used in decreasing frequency order are acupuncture (15/31, 48.4%), massages (8/31, 25.8%), chiropractic (7/31, 22.6%) and phytotherapy (6/31, 19.4%).
Two techniques emerge but in different ways: acupuncture is the most used CAM but the one deemed less efficient and massage is the least used CAM but the one deemed the most beneficial. This issue is still being debated. The CAM utilization rate in this population seems similar to that of the general population. The authors underline one more time. the need for controlled clinical trials.
The other publication is also a retrospective study on the painful future of SCI patients (traumatic and non-traumatic SCI) treated by electroacupuncture for below-level central neuropathic pain . The aim was to identify the improved and non-improved profiles.
The patients were treated by electroacupuncture while continuing to take their usual medications. They were evaluated with a double reading, in case of disagreement, a third independent reader settled the issue. Thirty-six patients with duration of pain ranging from 2 weeks to 15 months were included. Twenty-four patients reported an improvement on their pain intensity. Twelve patients reported no improvement. The difference is quite significant.
Among the 24 patients, the significant factors for responding positively to the treatment were:
- •
bilateral nature of the pain;
- •
symmetrical nature of the pain.
Patients with isolated burning pain were the most likely to improve.
The continuous nature of the pain did not significantly differentiate the patients who reported an improvement from those who did not. But when it is associated to the two factors mentioned above, it increases the discriminative power between improved and non-improved patients.
No adverse events were reported (no bleeding, infection or autonomic dysreflexia).
This study suggests the potential pain-relieving action of electroacupuncture by targeting its action on below-level central neuropathic pain in SCI patients. It is proposed as a secondary therapy in case of lack of responses to conventional medications.
No indication on the lingering postsession effect is reported.
1.6
Other physical therapies
When conventional physical therapies (massages, joint mobilization, thermotherapy, etc.) are found in the literature they are part of retrospective studies to evaluated the place of these therapies in treating central neuropathic pain in SCI patients.
If in the Norrbrink and Lundeberg publication , the massages and hot thermotherapy are validated as efficient by, respectively, 87 and 77% of patients, it is impossible to know which pain is targeted (nociceptive, central neuropathic or mixed). The authors recommend to continue using these therapies until the proof of their efficacy is validated.
The conclusions are quite similar for Cardenas and Jensen . The authors, after analyzing the results of a survey of 336 SCI patients, established for 117 of them suffering from chronic central neuropathic pain, a hierarchical ranking of efficient alternative treatments. Regarding physical therapies we find massages (55% of efficacy). Chiropractic (27% of efficacy) and biofeedback (23% of efficacy) are found at the bottom of the list with short postsession lingering positive effects.
In an another survey conducted by Nayak et al. , massages appear once again among the most efficient therapies without any possibilities to determine what type of pain is targeted.
Finally, a last publication is relevant because it underlines the risk of using poorly-indicated physiotherapy in treating central neuropathic SCI pain, aggravated by effort and that evokes the diagnosis of arachnoiditis .
It is also important to mention a study that underlines that acupuncture is not risk-free in quadriplegic patients with a neurovegetative risk and that autonomic dysreflexia episodes can occur between sessions .
Healthcare professionals recommend choosing pain-relieving transcutaneous neurostimulation as the first therapeutic option for treating central neuropathic pain. We have to agree that besides massages restricted to below-level areas and electrotherapy proposed for two types of pain, the other physical therapies remain quite confidential (less than 5% of users). We will note, however, that transcranial stimulation is now the choice of 3.49% of prescribing physicians for below-level central neuropathic pain.
1.7
Recommendations and conclusion
This literature review focusing on the impact of physical therapies on central neuropathic pain in patients, and more largely in SCI patients, shows how very few publications are available on these therapies used in SCI patients and how difficult and insufficient it is to implement a rigorous methodology in this context. Our review reports that three therapies dominate the literature: magnetic or electrical transcranial stimulation, pain-relieving transcutaneous neurostimulation and acupuncture.
Only the first one offers a literature rich in controlled randomized studies, either double-blind or crossover. Unfortunately some negative methodological aspects reduce the impact of their conclusions: insufficient characteristics regarding the type of pain, heterogeneous groups of patients, sample groups of traumatic or non-traumatic SCI patients that are too small, lack of control over the confusion factors (mainly those related to the patients mood and psychological state).
The clinical practices recommendations are labeled as grade B relative to randomized, low-power studies and underline the need to expand the studies in a more homogenous manner to SCI patients with a better control over the best known confusion factors, i.e. depression and anxiety.
Regarding acupuncture and pain-relieving transcutaneous neurostimulation, both techniques seem “promising” in terms of pain-relieving efficacy: for acupuncture on segmental neuropathic pain as well as below-level central neuropathic pain and for transcutaneous neurostimulation on segmental pain (at the injury level).
No controlled, randomized study can validate a preference. The harmlessness of these therapies is quite relative since transcutaneous neurostimulation is not recommended for allodynia and some cases of autonomic dysreflexia were reported during acupuncture sessions. However, these techniques if they are correctly administered only report some rare incidents and can be used daily. The publications on acupuncture and transcutaneous neurostimulation are labeled as grade C.
For all other techniques there are no potential application perspectives for treating neuropathic pain in SCI patients. Massages are defended by patients themselves without any physiological validation or clinical arguments (prospective or retrospective studies) to suggest further controlled clinical studies.
Appendix 1
Vote results (116 attendees from the Experts Conference + Internet 50 voters)
| Which physical therapy (one or more) would you prescribe for chronic below-level neuropathic pain? |
| Pain-relieving transcutaneous neurostimulation: 66,46% |
| Acupuncture: 1,40% |
| Electrical or magnetic transcranial stimulation: 3,49% |
| Thermotherapy: 1,40% |
| Massages: 12,70% |
| Electrotherapy: 9,20% |
| Vibrations: 2,70% |
| Electromagnetic waves: 1,40% |
| Ultrasounds: 1,81% |
| Others: 1,20% |
| None: 4,22% |
| Does not know : 2,41% |
| Which physical therapy (one or more) would you prescribe for chronic segmental (level of injury) neuropathic pain? |
| Pain-relieving transcutaneous neurostimulation: 75,16% |
| Acupuncture: 0,70% |
| Electrical or magnetic transcranial stimulation: 0,00% |
| Thermotherapy: 1,30% |
| Massages: 4,51% |
| Electrotherapy: 6,51% |
| Vibrations: 3,40% |
| Electromagnetic waves: 0,70% |
| Ultrasounds: 2,41% |
| Others: 0,00% |
| None: 3,01% |
| Does not know: 3,01% |
2
Version française
2.1
Introduction
La thérapie physique est une entité dont les contours sont mal définis et non consensuels. Elle concerne aussi bien des actes médicaux que kinésithérapiques. On y regroupe par expérience toutes les techniques à vocation thérapeutique fondées sur un contact physique et faisant appel à l’application de stimuli tactiles, de courants électriques ou de courants magnétiques.
Dans le traitement de la douleur, les thérapies physiques relèvent, en pratique courante, de la mobilisation articulaire et des massages ainsi que de l’électrophysiothérapie antalgique. Cette dernière associe l’électrostimulation transcutanée (TENS), l’application de froid ou de chaud, la thermothérapie, l’électrothérapie, le traitement par ondes électromagnétiques, l’énergie lumineuse, les vibrations, l’application d’ultrasons.
Chez le blessé médullaire, la pratique quotidienne réserve peu de place aux thérapies physiques pour traiter les douleurs neuropathiques.
Le but de la revue de la littérature est de faire le point sur la place réelle de ces thérapies dans l’arsenal thérapeutique de la douleur neuropathique chronique chez le blessé médullaire en phase séquellaire.
2.2
Méthodes
2.2.1
Matériel
Les critères d’inclusion des études sélectionnées pour cette revue de littérature se sont appuyés sur les recommandations de la Sofmer .
Les études sélectionnées sont prioritairement les essais cliniques libres ou contrôlés (randomisés ou non) ainsi que des articles de synthèse (méta-analyses et revues de littérature). La population concernée est une population adulte, de blessés médullaires principalement. Les publications concernant des patients affectés d’une lésion médullaire de nature médicale, lorsqu’ils étaient associés dans la même série à des blessés médullaires, ont été inclues.
Les critères d’exclusion ont trait à toutes les études expérimentales ou fondamentales (notamment neurophysiologiques) puisqu’il s’agit de dégager de cette revue de littérature des recommandations de pratique clinique. Les études chez l’enfant n’ont pas fait partie de cette revue. Les articles « généralistes » qui ne faisaient état des thérapies physiques que de manière descriptive ou qualitative, ainsi que ceux se rapportant exclusivement aux douleurs du secteur sus-lésionnel à dominante musculosquelettique ont été écartés.
2.2.2
Modalités de recherche bibliographique
Le critère de choix commun à toutes les publications est la variable « thérapie physique ». À la définition de thérapie physique, mentionnée ci-dessus, on a associé l’acupuncture et la stimulation corticale transcrânienne.
Les mots clés utilisés étaient :
- •
en langue anglaise : chronic neuropathic pain/SCI/human/adult/non-pharmacological treatment, transcutaneous electrical nerve stimulation, physiotherapy, acupuncture, hypnosis, physical therapy, transcranial magnetic stimulation, self management approaches .
Ont été associés à ceux recommandés par le comité scientifique, les mots clés suivants : heat therapy, ice therapy, cold therapy, massage, ultrasound, alternative treatment, complementary treatment, occupational therapy .
- •
en langue française : douleur neuropathique chronique/blessé médullaire traumatique/humain/adulte/traitement non pharmacologique/stimulation nerveuse périphérique/physiothérapie/TENS/acupuncture/hypnose/kinésithérapie/stimulation magnétique transcrânienne.
Ont été associés à ceux recommandés par le comité scientifique, les mots clés suivants: thermothérapie chaude, thermothérapie froide, massage, ultrasons, traitements alternatifs, traitements complémentaires et ergothérapie.
Une recherche au sein des bibliographies propres à chaque publication consultée, a également été effectuée. De la même manière, les liens Pubmed ont été consultés. Les résultats de ces recherches ont été associés à ceux du comité scientifique.
L’hypnose et les techniques d’autorééducation ( self-management ) n’ont pas été prises en considération, en deuxième lecture, car elles ne sont pas répertoriées dans le champ des thérapies physiques et relèvent plutôt de thérapies comportementales et d’éducation thérapeutique.
2.2.3
Modalités d’identification des pratiques professionnelles courantes
Ces pratiques ont fait l’objet d’une consultation par vote au cours de la Conférence d’experts et via Internet. Ce vote s’est prononcé sur deux questions :
- •
ou lesquelles des thérapies physiques suivantes prescrivez-vous dans le traitement des douleurs neuropathiques chroniques de type sous-lésionnel ?
- •
ou lesquelles des thérapies physiques suivantes prescrivez-vous dans le traitement des douleurs neuropathiques chroniques de type lésionnel ?
Les niveaux de réponses étaient les suivants :
- •
neurostimulation transcutanée antalgique (TENS) ;
- •
acupuncture ;
- •
stimulation transcrânienne électrique ou magnétique ;
- •
thermothérapie ;
- •
massage ;
- •
électrothérapie ;
- •
vibrations ;
- •
ondes électromagnétiques ;
- •
ultrasons ;
- •
autre ;
- •
aucune.
2.3
Résultats
La recherche bibliographique réalisée par le comité scientifique a retrouvé 71 articles. L’examen en texte entier et l’analyse des références des articles sélectionnés ainsi que la recherche personnelle ont permis d’isoler 39 articles éligibles sur la base des critères d’inclusion précités.
En associant des critères méthodologiques – étude contrôlée, randomisée contre placebo ou en crossover ou non randomisée – des critères de taille d’échantillon ou de singularité des résultats obtenus, 17 études ont été retenues. Dix études sont directement focalisées sur la stimulation magnétique ou électrique transcrânienne (Fig. 1) , quatre études concernent la TENS (Fig. 2) , et trois portent sur l’acupuncture (Fig. 3) . La présentation des publications dans chacun des tableaux fait état de la taille de l’échantillon représenté, de la méthodologie de l’étude, du niveau de contrôle des facteurs de confusion et du niveau de preuve scientifique. Les autres thérapies physiques n’ont été abordées que de manière anecdotique dans des articles dits « généralistes » sur la douleur neuropathique chez le blessé médullaire. L’insuffisance, voire l’absence de méthodologie et/ou l’absence de référence à un essai thérapeutique et/ou un échantillon de patients très petit, n’ont permis de ne retenir aucun écrit portant sur toutes les autres thérapies physiques.