Abstract
Background
Clinical outcomes and socioeconomic consequences after a stroke may differ between regions.
Methods
One cohort was established prospectively in Kunming (China) to compare with a cohort of 156 stroke patients included in Limoges (France). During 1 year, patients hospitalized within 48 hours for a first-ever hemispheric stroke were included. Demographic data and neurocardiovascular risk factors were registered. Hemiplegia was evaluated. Functional outcome was assessed using the Barthel Index (BI) after 3 months.
Results
One hundred and eighteen patients were included in Kunming. Patients of Kunming were younger (61.4 ± 13.4 vs 72.3 ± 14.6 years in Limoges, P < 0.0001), more involved in professional activity (36.4% vs 12.8%, P < 0.0001). Survival analysis indicated that mortality did not differ between cohorts, but independently predicted by coma at the 2nd day (HR = 9.33, 95% CI [4.39, 19.78]) and age > 70 years (HR = 6.29, 95% CI [2.36, 16.59]). Despite a better baseline BI for patients of Kunming (50.0 ± 34.9 vs 37.4 ± 34.2, P = 0.0031), after adjustment for confusing, patients in Limoges had a 2.11 OR 95% CI [1.03, 4.31]) to reach a BI > 80 at 3 months.
Conclusions
Functional recovery for patients of Kunming was not as good as expected. The socioeconomic consequences of stroke in Kunming are significant as they involved younger subjects who were still in work.
Résumé
Les conséquences fonctionnelles et socioéconomiques après accident vasculaire cérébral (AVC) peuvent variées d’un pays à l’autre.
Méthode
Nous avons comparé une cohorte d’AVC constituée prospectivement à Kunming (Chine) à une cohorte de 156 patients AVC suivie à Limoges (France). Durant un an, les patients hospitalisés dans les 48 heures suivant un AVC hémisphérique ont été inclus. Les données démographiques et les facteurs de risque neuro-cardiovasculaires ont été notés. Les hémiplégies ont été évaluées avec des échelles validées. Le devenir fonctionnel était évalué avec l’index de Barthel à trois mois.
Résultats
Cent dix-huit patients ont été inclus à Kunming. Les patients de Kunming étaient plus jeunes (61,4 ± 13,4 vs 72,3 ± 14,6, p < 0,0001), plus souvent en activité professionnelle (36,4 % vs 12,8 %, p < 0,0001). L’analyse de survie montrait que la mortalité ne différait pas entre les deux cohortes et était liée de façon indépendante à l’existence d’un coma au second jour (HR = 9,33, 95 % IC [4,39, 19,78]) et à un âge supérieur à 70 ans (HR = 6,29, 95 % IC [2,36, 16,59]). Malgré un score de Barthel initial plus bas (50 ± 34,9 vs 37,4 ± 34,2, p = 0,0031), après ajustement, les patients de Limoges avaient une meilleure récupération fonctionnelle à trois mois (OR 2,11, 95 % IC [1,03, 4,31]).
Conclusion
La récupération fonctionnelle pour les patients de Kunming n’était pas aussi bonne qu’espérée par le pronostic initial. Les conséquences socioéconomiques des AVC à Kunming sont plus importantes car concernent des sujets plus jeunes, en activité professionnelle.
1
English version
1.1
Introduction
Stroke is a major public health problem throughout the world, associated with a high mortality, disability rate and financial costs. At the present time, stroke is the second leading cause of death, representing 10% of all deaths worldwide , and half of the survivors suffer sequelae of various extents , which causes a high indirect socioeconomic burden after stroke .
The profiles and trends of stroke vary between countries . Of 5.7 million deaths of stroke in 2005, 87% were in low- and middle-income countries . Socioeconomic changes have led to the emergence of neurocardiovascular disease, especially in countries in transitional disease pattern . China is in regions of the highest incidence rate which attained around 210 per 100 000 per year , and mortality rate of stroke persisted in increasing, doubled from 1985 to 2005 . Some studies point out that age of first-ever stroke becomes younger . By contrast, benign trends have been observed in industrialized countries : retard in age of first-ever stroke, reduction in incidence of disabling or fatal stroke, and reduction in the proportion of modifiable risk factors . In France, incidence rate of stroke attains 145 per 100,000 per year, the French Dijon register study showed a stable incidence in spite of growth of population in risk, as well as the retard of age at first-ever stroke onset: 5 years in men and 8 years in women .
The goals of the management of acute stroke are to reduce the case fatality and dependent rate by 3 months after stroke onset . Studies of stroke prognostic can offer the predictors, which could serve as the targets of management. The present study aimed to compare the vital and functional outcomes by 3 months of first-ever hemispheric stroke, with consideration of epidemiological features, from a Chinese cohort established during the year from 2006 to 2007 with that of a French cohort constructed previously during 2002–2003.
1.2
Methods
1.2.1
Study design
This is an observational analytic longitudinal cohort study. Our study population consisted of patients of first-ever hemispheric stroke. The Chinese cohort was prospectively established from patients hospitalized in the Second Affiliated Hospital of Kunming Medical College of China (KM) during 2006–2007. The French cohort consisted of 156 first-ever stroke patients who were recruited prospectively in University Hospital of Limoges in France (LM). Same methodology was used in the establishment of these two cohorts. Patients were recruited over the course of 1 year with a follow-up period of 3 months. The study was approved by each local ethics committee and written consent was obtained from either the patient or their next of kin.
1.2.2
Sites of study and infrastructures
Kunming is a city of five million inhabitants, located in southwest of China. The Second Affiliated Hospital of Kunming Medical College is one of the main reference hospitals in this city, and covers essentially the Xishan District in which lives 448,000 inhabitants (census 2006). Limoges is a city in west central France. The University Hospital of Limoges covers the entire Limousine region, which has 725,000 inhabitants (census 2006). Both of the two cities are the capitals of their respective provinces, and are medium-sized cities in their respective countries.
For both of the two hospitals, the access to 24/24 hours cerebral computed tomography (CT) and magnetic resonance imaging (MRI) was available and none of them disposed a neurovascular unit during study period. In both sites, according the stroke etiology, medication treatment consisted of antiplatelet or anticoagulant drugs in ischemic stroke patients, and hypertonic agent for lowering intracranial pressure in hemorrhagic stroke patients. In LM, within the department of neurology, physiotherapy is provided from the second day after the stroke, when necessary, patients can then be transferred to a more suitable physical medicine and rehabilitation (PMR) department. While in KM, the access to the rehabilitation was limited by the finances of patients and the insurance coverage during the study period.
1.2.3
Inclusion criteria
All patients victim of a first hemispheric stroke with symptoms lasting at least 24 hours were included. We excluded patients with recurrent stroke and patients hospitalized after 48 hours of the onset of stroke symptoms. Patients with subarachnoid hemorrhage or subtentorial stroke were also excluded as well as patients who recovered completely within 24 hours without recent lesion on MRI.
1.2.4
Variable collections
The variables collected in this study consisted of sociodemographic information, risk factors and medical assessments. The socioeconomic information included age, sex, living situation, profession and employment status before stroke onset.
Key vascular risk factors assessments included arterial hypertension, current smoking, hypercholesterolemia, and diabetes mellitus as in validated studies . Hypertension was defined as recorded hypertension diagnosis in the medical history or the use of antihypertensive drugs or ≥ 160/90 mmHg during hospitalization post-stroke. Current smoking was considered present if a patient smoked daily prior to stroke, and was considered absent if the patient had never actively smoked or had stopped smoking for at least 1 year preceding the stroke. Hypercholesterolemia was considered if the total one plasma cholesterol value was equal or over 6.0 mmol/L before the stroke or at the time of admission. Diabetes mellitus was defined as a fasting plasma glucose level exceeding 110 mg/dl or the use of a blood sugar lowering drug before stroke.
Clinical assessments consisted of the stroke diagnosis, stroke subtype and hemispheric localization, level of consciousness, functional independence, and severity of limb paralysis, the presence of urinary incontinence, as well as medical complications and death.
Stroke was defined according to World Health Organization (WHO) criteria and classified into main types: ischemic stroke (IS), intracerebral hemorrhage (ICH) and stroke of undetermined pathological type, on the basis of clinical examination and radiological (CT or MRI) findings. Recurrent stroke was defined according the WHO Monica study , apparent onset of a new focal neurological deficit occurring more than 28 days after the index stroke. Level of consciousness was measured using the Glasgow Coma Scale , a score of 3 to 9 was defined as comatose. The functional independence was evaluated from the Barthel Index (BI) ; the higher the score the better the independence. A full score of 100 signifies complete independence in activities of daily living (ADL), a favorable functional outcome at 3 months was defined as BI > 80. The severity of limb paralysis was evaluated using the Demeurisse Motricity Index (MI) ; the higher the scores, the better the limb motor function. A full score of 100 means normal motricity, ≤ 1 means complete loss of motricity. Possible medical complications, such as pulmonary infection, urinary tract infection, shoulder pain, shoulder-hand syndrome, and pulmonary embolism were also collected.
1.2.5
Baseline assessment and follow-ups
Patients were examined daily by the corresponding doctors in the Emergency or Neurology Departments of each hospital. The baseline assessment was performed at the 2nd day (D2) after stroke onset by a neurologist investigator. A structured questionnaire was used to record relevant information of each patient.
The follow-ups consisted of medical assessment at the 15th day (D15) and end of the 3rd month (M3) after stroke onset. The score of BI at M3 was defined as the functional outcome. For the outpatients, the evaluations were carried out during a consultation organized for recruited patients. To guarantee the validity of data, the information available from each patient was checked weekly by the study group of neurologists and epidemiologists.
1.2.6
Statistical analysis
Database was established using EpiData 3.1 (EpiData Association, Denmark) with data controls. Quantitative variables were described as means with standard deviations. Qualitative variables were described as frequency and percentages. Continuous variables within groups were compared using Student t tests or Mann Whitney rank sum tests according to the distribution of variables. Comparisons between percentages were performed using Pearson’s Chi 2 test or Fisher’s exact test according the expected values.
Age was categorized as ≤ 70 versus > 70 years; MI at D2 was categorized as complete loss of motricity versus incomplete loss. The progress of independence function and motricity were assessed by calculating the difference of BI and MI between the M3 and the D2 after stroke onset. BI at M3 was dichotomized to ≤ 80 versus > 80.
Survival analyses used the Kaplan Meier and Cox proportional hazard models. Baseline time was time from date of stroke to death or censoring time. The Kaplan-Meier method was used to estimate the probability of survival 3 months after stroke onset, the two cohorts’ curves were compared using Peto-peto’s Wilcoxon test as the survival curves crossed. Estimates associated with cohorts were assessed by univariate followed by multivariate Cox model analyses. The hypothesis for proportional risks was checked by the log(−log S(t)) = f(t) curves. Variables with P -values < 0.20 in the univariate analysis were entered into the complete multivariate model, which was simplified in a stepwise descending manner. Differences in vital outcome were expressed as hazard ratios (HR); HR > 1 means association with a greater risk of decease than reference level.
A logistic regression model was used to assess adjusted estimates of favorable functional outcome (BI > 80) at M3 associated with cohorts. Univariate analysis was performed and variables with P -values < 0.20 were entered into the multivariate model, which was simplified in a stepwise descending manner. Differences in functional outcome were presented as odds ratios (OR); an OR > 1 means an association with a greater probability of getting a favorable functional outcome.
Confusion between variables were defined as variations in estimates > 20% when a variable was removed. Relevant interactions were tested in the final multivariate models.
P -values less than 0.05 were considered as statistically significant. Analyses were performed with SAS ® V9.1 (SAS Institute, Cary, NC) and STATA statistical analysis package (Stata Corp, Texas).
1.3
Results
1.3.1
Constitution of cohorts
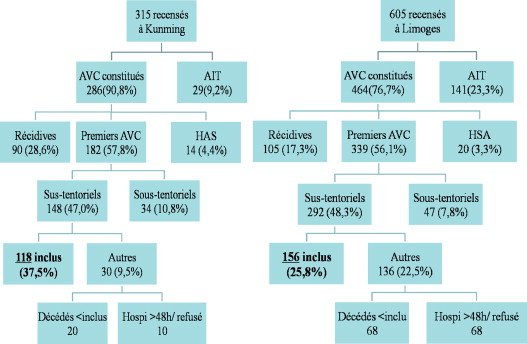
Three hundred and fifteen patients in Kunming and 605 patients in Limoges were hospitalized for all stroke subtypes during respective study period. The inclusion and non-inclusion process is displayed in Fig. 1 .
Patients in the cohort of KM were younger (61.4 ± 13.4) as compared to LM cohort (72.3 ± 14.6, P < 0.0001); more involved in profession activities, and usually had more cardiovascular risk factors. On the 15th day after stroke onset, they had more shoulder pain. Other main characteristics of the two cohorts were presented in Table 1 .
| Variables | Cohorts | P | |
|---|---|---|---|
| Kunming ( n = 118) Percent (%) | Limoges ( n = 156) Percent (%) | ||
| Age > 70 years | 27.1 | 62.8 | < 0.0001 |
| Male sex | 63.6 | 51.3 | 0.0423 |
| Living alone | 3.4 | 48.7 | < 0.0001 |
| In professional activities | 36.4 | 12.8 | < 0.0001 |
| Hypertension | 78.0 | 66.0 | 0.0307 |
| Hypercholesterolemia | 44.1 | 32.7 | 0.0542 |
| Current smoking | 38.1 | 27.6 | 0.0635 |
| Diabetes | 17.0 | 14.1 | 0.5172 |
| Hemorrhagic stroke | 39.8 | 15.4 | < 0.0001 |
| Localization in right hemisphere | 44.9 | 41.0 | 0.5192 |
| Initial coma | 16.1 | 11.5 | 0.2738 |
| Urinary incontinence at D2 | 17.0 | 41.7 | < 0.0001 |
| Pneumonia at D2 | 7.6 | 5.8 | 0.5388 |
| Shoulder pain at D15 | 31.2 | 19.2 | 0.0236 |
1.3.2
Mortality
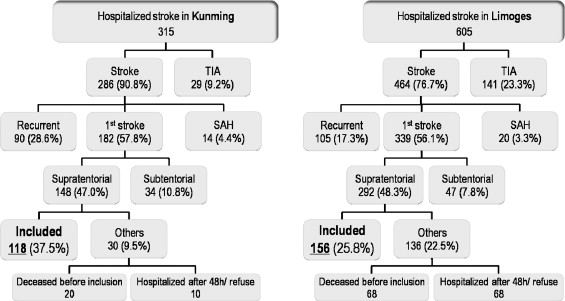
The mortality at M3 was 14.1% in the LM cohort and 9.3% in the KM cohort (Peto-peto’s Wilcoxon test, P = 0.37). As shown by Kaplan-Meier survival curve ( Fig. 2 ), the mortality in the KM cohort occurred mainly within the first 10 days, while death in the LM cohort occurred more after 15 days.
The univariate Cox proportional hazard model identified six variables associated with survival with P -values < 0.20: age (≤ 70 vs 70), living situation (with company vs alone), professional situation (inactive vs active), hypercholesterolemia (normal vs hypercholesterolemia), coma at D2 (absent vs present), and baseline MI (incomplete vs complete loss). In the final multivariate model, due to confusion, two non-significant variables (living situation and baseline MI) were maintained in the final model ( Table 2 ). The LM cohort was associated with a 0.47 adjusted HR, 95% CI [0.18–1.23]. Variables independently and significantly associated with death were presence of coma at D2 (HR: 9.33, 95% CI [4.39–19.78]) and age over 70 (HR: 6.26 [2.36–16.59]).
| Variables | Adjusted hazard ratio | 95% CI | P |
|---|---|---|---|
| Coma at D2 | |||
| Absence | RL | ||
| Presence | 9.33 | [4.39, 19.78] | < 0.0001 |
| Age | |||
| ≤ 70 years | RL | ||
| > 70 years | 6.26 | [2.36, 16.59] | 0.0002 |
| Loss of motricity at D2 | |||
| Incomplete | RL | ||
| Complete | 0.52 | [0.25, 1.09] | 0.0828 |
| Living situation | |||
| Living with company | RL | ||
| Living alone | 1.61 | [0.67, 3.89] | 0.2885 |
| Cohort | |||
| KM | RL | ||
| LM | 0.47 | [0.18, 1.23] | 0.1239 |
1.3.3
Functional outcome
As shown in Table 3 , the baseline BI was significantly higher in KM as compared to LM. However, BI outcome at M3 no longer differed between cohorts, while the MI remained better in KM. The progression of MI was parallel in the two cohorts, although there was greater progression of BI in LM.
| Variables | Cohorts | P a | |||
|---|---|---|---|---|---|
| Kunming | Limoges | ||||
| n | Mean ± SD | n | Mean ± SD | ||
| Baseline | |||||
| Barthel at D2 (/100) | 118 | 50.0 ± 34.9 | 156 | 37.4 ± 34.2 | 0.0031 |
| Motricity Index at D2(/100) | 118 | 58.2 ± 33.7 | 156 | 48.6 ± 36.4 | 0.0246 |
| Outcomes | |||||
| Barthel at M3 (/100) | 103 | 86.0 ± 20.2 | 114 | 79.6 ± 29.4 | 0.0608 |
| Motricity Index at M3(/100) | 103 | 88.6 ± 17.9 | 114 | 75.8 ± 30.6 | 0.0002 |
| Progress | |||||
| Progress in Barthel (D2 to M3) | 103 | 31.6 ± 26.5 | 114 | 43.9 ± 46.0 | 0.0185 |
| Progress in motricity (D2 to M3) | 103 | 24.6 ± 21.0 | 114 | 27.9 ± 48.4 | 0.5127 |
To adjust estimates associated with cohorts for functional outcome at M3, we used a logistic regression model. In the univariate analysis, the following seven variables were associated with better functional outcome (BI > 80 vs ≤ 80) with P -values < 0.20: age, sex, current smoking, coma at D2, urinary incontinence at D2, baseline BI and baseline MI. The final model ( Table 4 ) showed that cohort of LM was associated with a 2.11 OR, 95% CI [1.03, 4.31] to attain a BI > 80 at M3.
| Variables | Adjusted odds ratio | 95% CI | P |
|---|---|---|---|
| Age | |||
| ≤ 70 years | RL | ||
| > 70 years | 0.37 | [0.19, 0.73] | 0.0044 |
| Coma at D2 | |||
| Absence | RL | ||
| Presence | 0.21 | [0.07, 0.63] | 0.0054 |
| Loss of motricity at D2 | |||
| Incomplete | RL | ||
| Complete | 0.36 | [0.16, 0.83] | 0.017 |
| Urinary incontinence at D2 | |||
| Absence | RL | ||
| Presence | 0.43 | [0.21, 0.88] | 0.0203 |
| Sex | |||
| Female | RL | ||
| Male | 2.08 | [1.10, 3.94] | 0.0243 |
| Cohort | |||
| KM | RL | ||
| LM | 2.11 | [1.03, 4.31] | 0.0401 |
1.4
Discussion
Rapid socioeconomic progress, demographic and life style changes have taken place in China over the past decades, which conduct an epidemiological transition. As evidence of this transition, vascular disease has emerged as a leading cause of death among Chinese adults and stroke is responsible for over 40% of the total mortality . Comprehensive management strategies are urgently required in the primary prevention as well as in the acute and subacute phases to reduce the increasing burden of stroke in China.
In this study, the average age of 61 years of first-ever stroke found in the cohort of Kunming was comparable to that found by Wu et al. in a survey in 16 cities in the 1990s and a more recent multiple centre studies , almost 10 years younger than patients in the cohort of Limoges, so that patients in KM were more involved in professional activities. The predominance of male patients in KM may be also stem from this disparity in age. Our study also found a higher prevalence of modifiable risk factors in KM. Concurrence of multiple risk factors has potentiating effect , which may account for the younger age of stroke onset.
The case-fatality was independently prognosticated by age (> 70 years) and the presence of coma at D2. ICH was not found in the final model, but as ICH is more fatal in the early phase , it might account for the high early phase mortality in KM. After adjustment for prognostic factors, the LM cohort was associated with a 0.47 HR, not statistically significant ( P = 0.1239), but suggesting a decreased risk of death in LM, which accounted for the younger age of stroke onset in KM.
With respect to functional outcome, studies of stroke prognosis show that the motricity is the most important factor in functional independence , initial function is correlated with outcome , and initial urinary incontinence is a robust predictor . Patients in KM had better motricity at M3, better initial independence and less urinary incontinence, would thus be expected to have a better functional outcome. However, at M3, there was no univariate difference in BI between the two cohorts. Conversely, in the final multivariate model, patients in LM were associated with a 2.11 OR to attain a BI > 80 at M3. Notice that the recovery in motricity was parallel in both cohorts and motricity function always better in KM than in LM. Taken together, these results suggested that during the 3 months, patients in KM had insufficiently explored their independence function. This could partly be explained by the lack of rehabilitation training. Further, the complaint of shoulder pain was also more common in KM, while the incidence of shoulder pain is correlated with the severity of the motricity impairment . A higher motricity but more shoulder pain could be explained by the lack of facilities for postural care in bed, in manual handing, as well as in the access to rehabilitation in KM during early phase.
Several aspects restrict the access to rehabilitation in China. The first obstacle consists of a large gap of qualified rehabilitation professionals. An investigation estimated that in 2002 only 5640 qualified physiotherapists available in China, namely a density of 0.4 per 100,000 population , comparing with 55,800 physiotherapists in activities the same year in France, so a density of 93 per 100,000 . Besides the limited rehabilitative resources, finances are another limitation. Rehabilitation is often considered to increase the economic charge of patients, with knowing that 79% of rural residents and 45% of urban citizens in China have no health insurance . While in France, stroke is listed among the long-lasting affections for which 100% reimbursement is available through the French State Healthcare scheme. The proportion of stroke rehabilitation costs in China is just half of that in industrialized countries . Benefits of rehabilitation in stroke have been recognized: it improves not only the deficiencies, but especially the adaptation in ADLs . Recent health economic studies in China have shown a good costs/effectiveness for rehabilitation training . It would be interesting to continue this kind of health economic research to promote rehabilitation, in view of the resumption of professional activities in the younger patients.
1.4.1
Limitation and strengths
The limitations in this study stem from the fact that it was hospital-based and representations of whole regions were thus limited, patients with mild stroke not seen in hospital may have been overlooked. Then this study was a descriptive one, which compared between two very different regions at two periods with different healthcare systems. However, just as well, it reflected the real situations. The strength of this study stems from the survey of two large cohorts over a relatively long time using the same methodology. This latter point allowed us to perform multivariate analyses for survival and functional status resulting in adjusted estimates for cohorts.
1.5
Conclusion
Our results showed less functional recovery in the KM cohort, possibly due to the limited access to rehabilitation training caused by the limited healthcare resources. The consequences would have more impact as these patients were younger and more engaged in professional activities than were the LM patients.
2
Version française
2.1
Introduction
Les accidents vasculaires cérébraux (AVC) sont un problème majeur de santé publique à travers le monde avec une forte morbimortalité. Actuellement, les AVC sont la seconde cause de décès représentant 10 % des décès à travers le monde et la moitié des survivants ont des séquelles importantes, ce qui entraîne des conséquences socioéconomiques importantes .
Les caractéristiques épidémiologiques des AVC varient à travers les différents pays . Sur 5,7 millions de décès par AVC en 2005, 87 % ont eu lieu dans des pays à faible niveau économique . Les modifications socioéconomiques des pays en développement a fait accroître le poids des pathologies neuro-cardiovasculaires . La Chine est une région de forte incidence qui atteint 210 pour 100 000 par an avec un taux de mortalité croissant qui a doublé entre 1985 et 2005 . Certaines études en Chine ont souligné le fait que le premier AVC survient chez des sujets de plus en plus jeunes . Au contraire, certains éléments encourageants ont été observés dans les pays industrialisés : recul de l’âge du premier AVC, réduction de l’incidence, des séquelles, du taux de décès et réduction d’un certain nombre de facteurs de risque modifiables . En France, l’incidence est estimée aux alentours de 145 pour 100 000 par an et le registre de Dijon montre une incidence stable malgré l’augmentation des facteurs de risque ainsi qu’un recul de l’âge de survenue du premier accident, de cinq ans chez les hommes et huit ans chez les femmes .
L’objectif de la prise en charge aiguë est de réduire le taux de mortalité et de dépendance à trois mois . Notre étude avait pour but de comparer le devenir vital et fonctionnel à trois mois après un premier AVC hémisphérique entre une cohorte chinoise établie entre 2006 et 2007 et une cohorte française suivie précédemment entre 2002 et 2003.
2.2
Méthodes
2.2.1
Schéma de l’étude
Il s’agit d’une étude observationnelle, prospective, de suivi longitudinal de cohorte. Les sujets étudiés étaient des patients victimes d’un premier AVC hémisphérique. La cohorte chinoise a été constituée de façon prospective à partir des patients hospitalisés dans le Second Affiliated Hospital of Kunming Medical College of China (KM) entre 2006 et 2007. La cohorte française était constituée de 156 premiers AVC hémisphériques recrutés prospectivement à l’hôpital universitaire de Limoges en France (LM). La même méthodologie a été utilisée pour les deux cohortes. Les patients ont été recrutés pendant un an et suivis pendant trois mois. L’étude a été approuvée par le comité éthique local des deux hôpitaux. Un consentement écrit a été obtenu.
2.2.2
Lieu d’étude et infrastructures
Kunming est une ville de cinq millions d’habitants localisée dans le Sud-Ouest de la Chine. Le Second Affiliated Hospital of Kunming Medical College est l’un des hôpitaux les plus importants de la ville et couvre essentiellement le Xishan District dans lequel vivent 448 000 habitants. Les deux villes sont les capitales respectives de leur province et sont des villes de moyenne importance dans leur pays respectif.
Pour les deux hôpitaux, il existe un accès 24 heures sur 24 à l’imagerie cérébrale par scanner ou IRM et aucune des deux ne disposait d’unité neurovasculaire pour la prise en charge initiale. Sur les deux sites, en fonction de l’étiologie de l’AVC, la prise en charge comprenait un traitement antiagrégant plaquettaire ou anticoagulant pour les AVC ischémique et un traitement de l’œdème cérébral par agent médicamenteux pour les AVC hémorragiques. À Limoges, dans le service de neurologie, la kinésithérapie était débutée dès le second jour post-AVC et si nécessaire, les patients étaient transférés dans un service de médecine physique et de réadaptation. Au contraire, à Kunming, l’accès à la rééducation était limité par les considérations financières liées au système d’assurance des patients : très peu avaient donc accès à la rééducation.
2.2.3
Critères d’inclusion
Tous les patients victimes d’un premier épisode clinique d’AVC hémisphérique avec des symptômes durant plus de 24 heures. Étaient exclus, les récidives d’AVC, les patients hospitalisés 48 heures après le début des symptômes, les patients avec hémorragie méningée ou sous-tentorielle ou pour lesquels il n’y avait pas eu d’imagerie cérébrale dans les 24 premières heures.
2.2.4
Les variables collectées
Les données socioéconomiques collectées comprenaient l’âge, le sexe, le mode de vie, la profession. Les facteurs de risque évalués étaient l’hypertension artérielle, le tabagisme actif, l’hypercholestérolémie, le diabète . L’hypertension était définie par un antécédent ou des chiffres tensionnels supérieurs à 160/90. Le tabagisme actif a été retenu si le patient fumait les jours précédents l’AVC ; il n’a pas été retenu si le patient n’avait jamais fumé ou avait stoppé de fumer depuis plus d’un an avant l’AVC. L’hypercholestérolémie a été considérée présente si le taux était supérieur ou égal à 6 mmol/l avant l’accident ou au moment de l’accident vasculaire. Le diabète était défini par un taux de glucose supérieur à 110 mg/dl ou par l’existence d’un traitement diabétique avant l’AVC.
L’évaluation clinique comprenait la confirmation du diagnostic d’AVC, le type d’AVC – ischémique ou hémorragique –, le niveau de conscience, l’autonomie fonctionnelle, la sévérité des déficiences, la présence d’une incontinence urinaire et les complications médicales.
L’AVC a été défini selon les critères de World Health Organisation (WHO) et classé en deux types : accident ischémique (IS) et accident hémorragique (ICH) sur la base de l’examen clinique et de l’imagerie cérébrale . La récidive d’AVC a été définie selon les critères de l’étude WHO Monica par l’apparition d’un nouveau déficit neurologique focal plus de 28 jours après un premier accident. Le niveau de conscience a été mesuré par l’échelle de Glasgow , un score de 3 à 9 définissant un coma. L’indépendance fonctionnelle a été évaluée par l’index de Barthel (IB) . Une évolution favorable a été définie par un score d’IB supérieur à 80. La sévérité de la paralysie des membres a été évaluée par l’index moteur de Demeurisse (IM) : plus le score est haut, moins la paralysie est importante ; un score à 100 signifie une motricité normale. Les possibles complications médicales, comme les infections pulmonaires, urinaires, douleurs d’épaule, embolie pulmonaire, ont été collectées.
2.2.5
Évaluation initiale et suivi
L’évaluation initiale a été réalisée le second jour post-AVC (j2) par un neurologue investigateur. Un questionnaire structuré a été utilisé pour recueillir les informations pour chaque patient.
Le suivi consistait en une évaluation médicale le 15 e jour et final à la fin du troisième mois après l’AVC (M3). Le devenir fonctionnel a été défini par le score de IB à M3. Pour les patients sortis de l’hôpital, l’évaluation a été réalisée durant une consultation à l’hôpital.
2.3
Analyse statistique
La base de données a été établie sur EpiData 3.1 (EpiData Association, Danemark) avec contrôle des données. Les variables quantitatives ont été exprimées par les moyennes et les déviations standards. Les variables qualitatives ont été exprimées par les fréquences et les pourcentages. Les variables continues ont été comparées en utilisant le test t de Student ou Mann Whitney selon la distribution des variables. La comparaison entre les pourcentages a été réalisée en utilisant les tests Pearson’s Chi 2 ou Fischer’s exact.
L’âge a été catégorisé en deux, inférieur ou égal à 70 versus supérieur à 70. Le score moteur a été également catégorisé en deux niveaux : déficit moteur complet versus déficit moteur incomplet à j2. La progression sur le score de l’IB et sur le mI a été calculée par la différence entre le résultat à M3 et l’évaluation initiale à j2.
L’analyse de survie a été réalisée à partir des modèles de Kaplan Meier et Cox proportional hasard model. La méthode de Kaplan Meier a été utilisée pour estimer la probabilité de survie à M3 et les courbes des deux cohortes ont été comparées avec le test Peto-peto’s Wilcoxon.
La différence dans le devenir vital entre les deux cohortes a été exprimée par le hazard ratios (HR) ; HR supérieur à 1 signifiant un plus fort risque de décès.
Une régression logistique a été utilisée pour ajuster les variables liées à une bonne récupération fonctionnelle (IB < 80) à M3. Les variables ont été étudiées en univariées et celles avec un p < 0,20 ont été entrée dans le modèle multivarié.
p < 0,05 a été considéré comme significatif sur le plan statistique. Les analyses ont été réalisées avec SAS V9.1 (SAS institute, Cary, NC) et STATA statistical analyis package (Stata Corp, Texas).
2.4
Résultats
2.4.1
Constitution des cohortes
Trois cent quinze patients à KM et 605 à LM ont été hospitalisés pour tout type d’AVC pendant la période respective d’inclusion. Le diagramme d’inclusion est représenté par la Fig. 1 .