Vascular Complications in Cervical Spine Surgery
Brian Kwon
Louis G. Jenis
INTRODUCTION
Vascular injuries occurring during cervical spine surgery can vary from relatively minor to catastrophic hemorrhage and death (1,2,3,4,5,6,7,8). Avoidance of these injuries requires a comprehensive understanding of the vascular anatomy surrounding the cervical spine, as well as the common mechanisms of iatrogenic injury. The consequences of vascular injuries may range from significant acute or delayed hemorrhage or ischemia to the brain and spinal cord, to pseudoaneurysm formation or thrombosis.
While the most effective treatment for these complications is avoidance, often these injuries can neither be anticipated nor predicted. Specific risk factors and anatomic anomalies have been described and studied (3,6,7,9,10), but because vascular injuries are so rare, a consensus on treating these injuries has not been established. The primary vascular structures of concern in cervical spine surgery are the vertebral and carotid vessels with their associated tributaries.
ANATOMY
The main vessels of the head and neck are the paired common carotids that ascend in the neck to the level of the thyroid cartilage where it divides into external and internal branches. The external carotid supplies the head, face, and majority of the neck, and the internal carotid supplies the cranial cavity. The common carotid arteries and veins lie in a deep-seated sheath on each side of the neck bordered by the transverse processes of the cervical vertebrae and attached muscles posteriorly, the pharynx, larynx, trachea, and esophagus medially, and the sternocleidomastoid and associated strap muscles anterolaterally. The common carotid typically does not have any branches.
The external carotid artery gives rise to the superior thyroid artery, among others, and traverses the anterior neck at the level of the C3 and C4 vertebral bodies where it ends within the thyroid gland and adjacent muscles. The superior thyroid artery often accompanies the superior laryngeal nerve.
The inferior thyroid artery arises from the thyrocervical trunk off the subclavian artery and ascends along the medial border of the anterior scalene muscle; it then descends along the longus coli muscle and into the inferior aspect of the thyroid gland at the level of the C6 or C7 vertebral bodies. The inferior thyroid artery is an important landmark in the neck as the recurrent laryngeal nerve often shares this anatomic course. There is a relatively avascular plane between the superior and inferior thyroid arteries from C3 to C6 that allows for ease of dissection during anterior approaches to the disc and vertebral bodies.
The vertebral artery (VA) arises from the first part of the subclavian artery at the level of the first thoracic vertebra and courses cranially behind the carotid artery between longus coli and scalenus anterior muscles. It ascends anterior to the C7 foramen transversarium in most individuals and enters the osseous foramen of the subaxial cervical vertebrae at C6, where it continues its ascent until it reaches the atlas. A fibroligamentous band at the level of the intertransverse space encases the VA and exiting spinal nerve (11,12). The VA lies anterior to the ventral rami of the cervical nerves from C2 to C6 and is surrounded by an extensive venous plexus and sympathetic nerve fibers. In the lower cervical spine the VA is located more anteriorly; at the C3 level it is located more posteriorly and is closer to the neuroforamen
at these levels. At the level of C1, the VA courses posteromedially over the arch and into the foramen magnum (13,14). Posteriorly, the VA is at risk primarily during dissection that courses too far laterally from the midline of the posterior ring of C1. Ebraheim et al. reported that the minimum distances notable for safe dissection were 12 mm from midline on the inferior aspect of the ring of C1 and only 8 mm from midline on the superior aspect (15).
at these levels. At the level of C1, the VA courses posteromedially over the arch and into the foramen magnum (13,14). Posteriorly, the VA is at risk primarily during dissection that courses too far laterally from the midline of the posterior ring of C1. Ebraheim et al. reported that the minimum distances notable for safe dissection were 12 mm from midline on the inferior aspect of the ring of C1 and only 8 mm from midline on the superior aspect (15).
Of importance for anterior decompression surgeries is that the VA is enclosed within the foramen transversarium at the level of the vertebral body, while at the disc space, it is relatively unprotected and passes only millimeters from the neuroforamen. In addition, during the passage from transverse foramen to transverse foramen, the VA lies in close contact to the lateral wall of the vertebral body in the midcervical spine.
Vaccaro et al. reported on measurements of various anatomical relationships of the foramen transversarium to the vertebral bodies (16) (Fig. 2.1). They evaluated computed tomography scans of patients aged 18 to 88 years (average 43 years) to evaluate trauma or degenerative disc disease. They measured the transverse distance between the outer cortices of the foramen transversarium (interforaminal distance) and from the posterior border of the vertebral body. They found that the interforaminal distance increased from the cranial (25.90 ± 1.89 mm at C3) to caudal (29.30 ± 2.70 mm at C6) vertebrae. In addition, the distance of the foramen transversarium from the posterior border of the vertebral body increased at the more caudal levels (2.16 ± 1.18 mm at C3 to 3.53 ± 1.56 mm at C6). They concluded that the risk of VA injury is greater in the more cranial vertebral levels due to these anatomic relationships.
Using dry cervical spine specimens, Ebraheim and colleagues measured parameters including interforaminal distance, interuncinate distance, and transverse vertebral body diameter. They also concluded that nearly all of the parameters decreased in the more cephalad vertebrae and agreed that the VA is at increased risk of injury during decompression of more cephalad levels, given the anatomic position of the artery to the area where neural decompression is required (11,17).
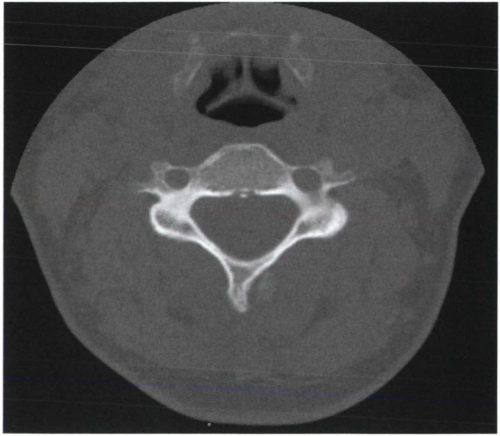 Figure 2.1 Axial CT scan at the level of the vertebral body. Note the intertransverse foramen distance and anatomic relationship of the artery to the lateral wall of the vertebral body. |
In addition to the normal anatomic relationships within the cervical spine, several studies have outlined relevant anomalies. A cadaveric and clinical case study published by Curylo et al. reviewed the incidence of anomalous vertebral arteries (3). They defined an anomalous VA pathway as existent when the foramen transversarium was medial to or less than 1.5 mm lateral to the uncovertebral joint. They found seven anomalous arteries in 222 total specimens (2.7%), and six of the seven were at C3 or C4. In addition, they noted that in most patients, the medial margin of the uncovertebral joint is, on average, 5.5 mm medial to the medial cortex of the foramen transversarium. Oga et al. used angiography to identify and classify tortuosity of the VA in patients with cervical myelopathy. They put forth a classification scheme and suggested an association between cervical spondylotic myelopathy and a tortuous or looped VA (9).
Finally, in the general population, hypoplasia and absence of the VA has been noted: The left was identified to be hypoplastic in 5.7% and absent in 1.8%, whereas the right was hypoplastic in 8.8% and absent in 3.3% (5).
INCIDENCE OF VACUSLAR INJURY WITH CERVICAL SPINE PROCEDURES
Anterior Decompression Surgery
The only incidence of direct common carotid injury is reported by Lesoin, in which one case was described in 800 anterior cervical operations (0.1%) (18). The mechanism of injury, treatment, or sequelae was not fully described. There have been at least two reports involving three patients with carotid artery thrombosis, both of which were attributed to retraction during cervical corpectomy (2,8). It was felt that the longer operative times required to perform these complex operations, as well as advanced age and presence of atherosclerotic disease, were risk factors for this complication. Two of the three patients were left with permanent hemiplegia. The authors suggest that preoperative carotid ultrasonography may be helpful to determine which side is more stenotic and, in severe cases, which approach (anterior or posterior) should be taken (2).
Injury to the traversing superior and inferior thyroid arteries is not uncommon during anterior cervical exposures, and is typically identified at the time and easily managed. A late presentation of an inferior thyroid artery pseudoaneurysm
has been reported and managed with noninvasive vascular techniques (19).
has been reported and managed with noninvasive vascular techniques (19).
Vertebral artery injuries may occur during anterior procedures on the subaxial spine (5,6,7,12,20). Golfinos et al. (5) reported on four VA injuries after 1,215 (0.3%) anterior discectomy or corpectomy procedures performed for myelopathy or myeloradiculopathy. The injury was caused by mechanized air drilling in two patients, screw tapping in one, and soft tissue retraction in one patient. Acute hemorrhagic blood loss ranged from 500 to 1,500 cc, and unsuccessful attempts at repair were made in all cases. No patients suffered permanent neurological sequelae (i.e., vertebrobasilar insufficiency).
Smith et al. (7) reported on 10 VA injuries during anterior decompressive procedures by several surgeons, for an incidence of approximately 0.5%. Most injuries occurred during vertebral corpectomy or hemicorpectomy procedures (9 of 10) using a mechanized burr or air drill. Blood loss ranged from 300 to 4,500 cc, and treatments varied. Six of 10 patients suffered neurologic sequelae ranging from cerebellar infarction to nerve root damage and radiculopathy from transosseus arterial ligation. Similarly, Eleraky et al. (21) experienced four VA injuries in 185 (2.2%) procedures during corpectomy. Three were caused by drilling and one by retraction in a patient with plasmacytoma (this patient was reported twice from the same institution) (5).
Daentzer and colleagues reported two VA injuries related to anterior neck surgery and a review of the literature where a total of 29 reported injuries were detailed (4). They concluded that incidence of VA injury varied from 0.05 to 0.95%. Consequently, among those 29 patients with VA injuries, there were five permanent neurological deficits and three morbidities, resulting in a permanent neurologic complication rate of 27.6% and a significant mortality rate of 13.8%. Fatal subarachnoid hemorrhage of a vertebral artery pseudoaneurysm 4 days after odontoid screw placement was the cause of one death, and information was not available on the other two.
Posterior C1-C2 Procedures
Posterior cervical procedures also place the vertebral artery at risk for injury during lateral exposure and instrumentation at the atlantoaxial joint (22,23). When exposing the posterior surface of the atlas ring, lateral dissection 1.5 cm beyond the midline in adults (1.0 cm in children) places the vertebral artery at risk of injury (23). This is especially evident along the superior aspect of the C1 ring, as the VA wraps from the foramen at C2 and then anterior to the high cervical spinal cord and into the foramen magnum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








