Abstract
Subcutaneous rupture of the tibialis anterior tendon is rare. Diagnosis is usually clear. The essential clinical symptoms are progressively: footdrop gait, loss of ankle flexion strength, ankle foot pain and claw toes. But the occurrence of an asymptomatic time period between the injury and the onset of clinical signs can make the diagnosis more difficult. MRI is the gold standard examination for tendons injuries and associated bone and joints damages. Surgical exploration confirms MRI findings. It constitutes the treatment of choice for tibialis anterior tendon rupture. Surgical or functional techniques used have an impact on the design of the rehabilitation program, essential step in the care management of these injuries. It avoids postoperative tendon adhesions and their functional consequences. We report here a case of a man presenting with footdrop gait as the only clinical symptom.
Résumé
La rupture sous-cutanée du tendon du tibialis anterior est rare. Son diagnostic ne pose souvent pas de difficulté. Les signes cliniques sont parlants et consistent en l’installation d’un steppage, d’un déficit de la flexion dorsale de la cheville, de douleurs de la face antérieure de la cheville et du pied et d’une attitude des orteils en griffe. Cependant, la survenue d’un intervalle libre entre le traumatisme et l’installation des signes cliniques peut amener à une discussion diagnostique. Dans ce cas, l’IRM constitue un excellent examen pour poser le diagnostic de la lésion tendineuse et rechercher d’éventuelles lésions associées des structures osseuses et articulaires. L’exploration chirurgicale confirme les données de l’IRM et permet de traiter la rupture du tendon du tibialis anterior. La technique utilisée conditionne la rééducation fonctionnelle qui reste fondamentale dans la prise en charge de cette lésion. Elle permet d’éviter les adhérences et les conséquences fonctionnelles. Nous rapportons ici le cas d’un patient se présentant pour l’exploration d’un steppage isolé.
1
English version
1.1
Introduction
Tendon ruptures of the tibialis anterior (TA) are not very common and often occur in young people as a result of open trauma. In this case, the diagnosis is usually quite an easy one with clear symptoms . However, footdrop gait secondary to a partial injury resulting from closed trauma is rare. We report here a case of one man presenting with footdrop gait as the only clinical symptom.
1.2
Observation
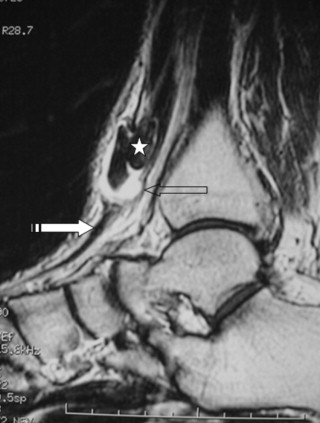
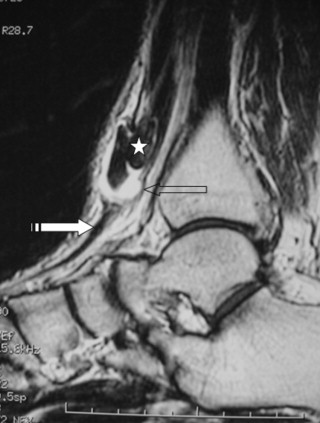
Mr. A, a 40-year-old construction worker, with no significant medical history, presents with footdrop gait on his right side. We find a history of direct trauma to the lower part of his right leg 2 months ago. After a three-week asymptomatic period, this footdrop gait progressively appeared without any pain. The examination found moderate swelling on the injured area. At palpation, we found a tender lump measuring about 1 cm in diameter, adhering to deep and superficial plans. A carefully orthopedic examination of the ankle showed a limitation of active and passive plantar flexion (10°) as well as active dorsal flexion (5°). The neurological examination and ankle radiographic imaging results were normal. MRI was scheduled to explore musculotendinous structures. It showed a myotendinous TA injury with a partial discontinuous aspect as well as effusion in the tendon sheath and peritendinous space ( Fig. 1 ). This evoked a partial rupture of the TA at its myotendinous insertion. The surgical exploration revealed a myotendinous partial rupture estimated at 50% of the tendon. It also showed a thickening of the sheath, inflammation and multiple adhesions which were surgically removed and the tendon was repaired. The foot was immobilized in a cast. Afterwards an intensive rehabilitation program was implemented (three sessions per week for a total of 6 weeks) to maintain tendon freedom against superficial and deep plans, recover ankle range of motion (ROM) and strengthen dorsiflexion muscles. The rehabilitation session always began by ultrasound therapy, either with the pulsed or continuous mode (respectively for defibrosis through a mechanical defibrinating action and pain relief), electrotherapy, ending by deep transverse massages next to the scarred tendon. Passive and active mobilization of the ankle was achieved by performing strengthening exercises against manual resistance. Proprioceptive training was also performed to achieve proprioception ankle muscle control. Six months later, the patient had regained a normal walk without any footdrop gait or pain and was able to resume work.
1.3
Discussion
TA is the main dorsiflexion muscle of the ankle. Tendon rupture is often secondary to open and sometimes closed trauma, usually associated to tibial fracture . More rarely, it can occur spontaneously under medication (fluoroquinolones and statins), or because of psoriasis and gout . In addition, there was an avascular area in the front middle-half of the TA, considered as an important risk factor of the degenerative process. Indeed, it increases the risk of tendon rupture injury and could explain this spontaneous occurrence of TA rupture . Regarding untreated TA ruptures, the most frequently reported symptoms in the literature are: a progressive footdrop gait, loss of ankle dorsiflexion strength, pain on the front of the ankle, pain and claw toes . The specificities of our case are first a TA partial rupture secondary to closed trauma of the lower third of the tibia and second, the presence of an asymptomatic time period between injury and onset of footdrop gait, which was the only functional symptom. For our patient, TA impairments at the wheelbase of the tendon sheath and adhesions to the adjacent tissues were a real hindrance to the foot flexor muscles. MRI, as sensitive as ultrasound imaging , is an excellent investigating examination for analyzing tendon structures and discarding any associated bone or joint injuries. It permits to easily differentiate between a tendinopathy and partial or total TA ruptures . The treatment is surgical. When the tendon rupture is complete, the tendon is desinserted from the bone and becomes necrotic, the suture is thus impossible. The solution is to bridge the entire lacerated area with the third toe extensor tendon. The proximal and distal tendons of the TA are sutured to the third toe extensoris tendon, cut beyond the suture zone into the third tendon. The distal fragment of the third toe extensor is sutured onto the second extensor. The flexor tendon pulleys are incised on the medial edge very close to the tibia preserving sufficient tissue for closure. In case of distal rupture, the tendon is ruptured very close to the bone, sometimes with a piece of bone stuck to it, there are no lacerations and surgical repair is easier. The technique is to braid the tendon and reinsert it onto the bones anchored on two points. In case of partial tendon rupture, as seen in our patient, the tendon sheath is incised close to the tibia, the lesion is then revived, the pathological tissue is resected and the tendon is sutured longitudinally and the sheath is finally closed down. In all cases, the ankle is immobilized in a cast . Table 1 lists the different cases of TA tendon rupture reported in the literature.
| Author | Sex/ Age (year) | Mechanism | Ultrasound | MRI | Surgical treatment | Retreat |
|---|---|---|---|---|---|---|
| Neumayer & al (2009) | Man 57 | Forced plantar flexion | Partial rupture of the TA | Complete rupture of the TA | Reinsertion of the proximal tendon stump inside the distal stump | 2 years |
| Woman 77 | Corticosteroid injection into the ankle | Distal rupture of the TA | – | Suture of the tendon and tenodesis of the TA to the extensor retinaculum | 1 year | |
| George et al. (2009) | Woman 68 | Twist of the ankle during dance | Rupture of the TA with proximal retraction | – | The proximal retracted tendon was split longitudinally and the free end flipped over and sutured to itself after passing the tendon through a hole in the first metatarsal | 6 months |
| El Maraghy et al. (2009) | Man 76 | Slip on the ice, foot caught in a hole | Complete distal rupture of the TA | – | Reinsertion of the TA in the cuneiform | 6 months |
| Our case (2011) | Man 40 | Direct traumatism | – | Partial rupture | Remove of the adhesions and tendon repair | 6 months |
During the course of a TA injury, we must insist on rehabilitation even after closed trauma with no clear symptoms. Indeed, the local inflammatory reactions are important, especially during the first week post-injury with a risk of adhesions and functional consequences. These adhesions can be prevented by Cyriax deep transverse massage, which must be delivered precisely at the exact location of the tendon injury . Early mobilization after surgery helps tendon remodeling and reduces the risk of adhesions . Other therapies, like ultrasound therapy, are also used. Their effects depend on the delivering modalities. Pulsed ultrasounds have a defibrinating action on soft tissues and enhance the remodeling of scar tissues to make them more flexible and compatible with joint functions. Continuous ultrasounds have an analgesic effect . Electrotherapy is also an interesting treatment for pain and speeding up the healing process . The design of the rehabilitation program depends on the surgical technique used. In case of trauma tendon rupture with avulsion of the TA, surgical repair consists in the reinsertion of the tendon into the cuneiform. Loading on the repaired limb is forbidden during 6 weeks; during that time, the ankle is immobilized in a protective splint to maintain it in a neutral position. In our case, the patient was allowed to walk with crutches loading on the injured ankle, if tolerated, with his foot flat on the floor. Heel-striking gait requiring dorsiflexion of the TA tendon to lift the foot was not allowed. At 8 weeks postoperatively, a more normal gait pattern was initiated along with muscle strengthening training that progressed from isometric exercises to resistant eccentric and concentric training exercises . In our case, the rupture was partial, the tendon was repaired and the rehabilitation begun 6 weeks after the surgery, when the cast was removed. Passive exercises to regain ROM and active strengthening of the TA were implemented. Gait rehabilitation started right away with full loading on the ankle.
1.4
Conclusion
TA tendon injury is a rare etiology for footdrop gait. The asymptomatic time period after closed trauma of the lower leg can be a telltale sign of partial TA tendon injury complicated by adhesions. Surgery confirms ultrasound or MRI findings and permits the release of tendon adhesions. Rehabilitation program is an essential part of the care management of these injuries, regardless of the initial treatment: functional or surgical. In both cases, it avoids significant functional consequences.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
Les ruptures du tendon du tibialis anterior (TA) surviennent souvent chez les sujets jeunes et résultent de traumatismes ouverts. Dans ces cas le diagnostic est facile. Mais le steppage secondaire à une lésion partielle dans le cadre d’un traumatisme fermé est rare. Nous rapportons le cas d’un patient qui présente un steppage comme seul signe clinique.
2.2
Observation
M. A, âgé de 40 ans, ouvrier maçon sans antécédents pathologiques notables consulte pour un steppage du côté droit. Nous trouvons la notion d’un traumatisme fermé, direct du tiers inférieur de la jambe droite (chute d’une brique) remontant à deux mois. Après un intervalle libre de trois semaines du traumatisme initial, un déficit de la flexion dorsale de la cheville droite est apparu progressivement entraînant un steppage à la marche sans autres signes, notamment pas de douleur. L’inspection montre une tuméfaction modérée en regard de la zone du traumatisme. La palpation objective la présence d’un nodule sous-cutané sensible de forme ovalaire de 1 cm de grand axe et adhérent aux plans superficiels et profonds. Le bilan articulaire de la cheville droite trouve une limitation de la flexion plantaire active et passive (10°) et de la flexion dorsale active (5°). Le reste de l’examen physique, notamment neurologique, ainsi que la radiographie de la cheville sont sans anomalies. Pour explorer les parties molles, nous avons pratiqué une IRM qui a montré une lésion de la jonction myo-tendineuse du TA avec un aspect partiellement discontinu et un épanchement de la gaine tendineuse et de l’espace péri-tendineux ( Fig. 1 ). Cet aspect évoque une rupture partielle de la jonction myo-tendineuse du TA. L’exploration chirurgicale a confirmé le diagnostic en objectivant une rupture évaluée à 50 %, un épaississement de la gaine tendineuse, une inflammation locale et de multiples adhérences. Ces dernières ont été soigneusement libérées et le tendon a été suturé. La cheville a été ensuite immobilisée par une botte plâtrée durant six semaines. La rééducation fonctionnelle (trois séances hebdomadaires pendant six semaines) postopératoire a visé le maintien de la liberté du tendon du TA par rapport aux plans superficiels et profonds, le gain des amplitudes articulaires de la cheville et le renforcement des releveurs. La séance de rééducation a débuté par des moyens physiques : application d’ultrasons pulsés et continus (respectivement pour leur action défibrosante et antalgique), de l’électrothérapie, suivis par des massages transverses profonds en regard de la cicatrice tendineuse. Un travail passif et actif de la mobilité articulaire est réalisé couplé à des exercices de renforcement musculaire contre résistance manuelle. Le travail du contrôle proprioceptif d’abord en décharge, puis en bipodal et enfin en unipodal du coté de la lésion sur plan stable, puis sur plateau de Freeman a complété le programme de rééducation. Après un recul de six mois, le résultat fonctionnel était satisfaisant et le patient a retrouvé une marche sans steppage et a repris son travail.