Abstract
We present the case of a 54 year-old man presenting with a right Brown-Séquard plus syndrome (BSPS) after a traumatic cervical spinal cord injury. After being operated on with selective tibial neurotomy and triceps surae lengthening because of a right spastic equinus foot, he developed a gait disorder at high speed. The patient complained about an instability of the right knee. Observational gait analysis exhibited an oscillating, flexion/extension motion of the right knee during stance, which was confirmed by gait analysis. Dynamic electromyographic recordings exhibited a clonus of the right rectus femoris (RF) during stance. The spastic activity of the RF and the abnormal knee motion totally reversed after a motor nerve block of the RF, as well as after botulinum toxin type A injection into the RF. We emphasize that complex, spastic gait disorders can benefit from a comprehensive assessment including gait analysis and nerve blocks.
Résumé
Nous présentons le cas d’un homme de 54 ans présentant un syndrome de Brown-Séquard plus (BSPS) droit séquellaire d’un traumatisme vertébromédullaire cervical. Au décours d’une chirurgie associant neurotomie tibiale sélective et allongement du triceps sural (TS) en raison d’un pied équin spastique, il a présenté un trouble de la marche survenant à vitesse rapide. Le patient s’est plaint d’une sensation d’instabilité du genou droit. L’analyse observationnelle de la marche a objectivé un mouvement anormal, oscillatoire, de flexion/extension pendant la phase d’appui du côté droit. Cette anomalie a été confirmée par une analyse quantifiée de la marche (AQM). L’enregistrement électromyographique (EMG) dynamique a mis en évidence un clonus du muscle rectus femoris (RF) droit pendant la phase d’appui. Cette activité spastique du RF et l’instabilité du genou ont totalement disparu après un bloc moteur du nerf du RF ainsi qu’après une injection de toxine botulique dans le RF. Nous discutons l’intérêt de l’utilisation combinée de l’AQM et des blocs moteurs dans l’exploration des troubles complexes de la marche chez les sujets spastiques.
1
English version
1.1
Introduction
The Brown-Séquard syndrome (BSS) has been first described in 1851 from a case report of a stab-wound spinal cord injury . It is a syndrome consisting of ipsilateral upper motor neuron paralysis (hemiplegia) and loss of proprioception with contralateral pain and temperature sensation deficits. In traumatic spinal cord injuries, the pure form of BSS is rarely observed . Recently, a derivative has been introduced with the term Brown-Séquard-plus syndrome (BSPS). BSPS is a spinal cord injury (SCI) with bilateral involvement of upper and/or lower extremities and is defined as an incomplete SCI syndrome with ipsilateral weakness and contralateral loss of pinprick and temperature sensation . The BSPS probably account for 2-4% of all traumatic spinal cord injuries . The evolution of BSPS allows independent walking in 75% of cases , but frequently BSPS patients exhibit a gait disorder due to spasticity in the more involved lower limb. These situations of complex gait disorders are worth a precise assessment, which allows targeted treatment procedures. When considering the benefit from a focal treatment of hypertonia in these patients, the use of transient nerve blocks, as well as quantitative gait analysis, appear as precious tools . We present a case of a BSPS patient illustrating the interest of combining these tools.
1.2
Patient and methods
A 53-year-old man underwent a traumatic spinal cord injury on December 8th 2008 (3-m high fall, occupational accident), causing an incomplete, AIS grade C spastic tetraplegia with right motor level C8, left motor level C5, right sensory level C6, and left sensory level C4. The initial ASIA upper limb motor score was 32 and the lower limb motor score 30 . The computed tomography scan exhibited a C7 fracture, and the patient underwent surgery (C7 corporectomy and osteosynthesis). The patient was admitted in our neurological rehabilitation department 6 weeks later. After 8 months, his neurological status had evolved towards an incomplete AIS grade D spastic tetraplegia with right motor level C8, left motor level C7, and sensory level C4. The ASIA upper limb motor score was 43 and the lower limb motor score 39. He was classified as a BSPS because of the right predominance of the weakness, spasticity and proprioceptive disorders and left predominance of the loss of pinprick. In September 2009, on discharge, he regained home being independent for all activities of daily life. He was able to walk at least 500 m with a cane. One year later, the patient complained of a worsening of his gait. The observational gait analysis noticed that the gait disorder consisted mainly in a spastic equinus varus foot and clawing toes of the right leg. The initial contact and the stance phase on the right side were performed on the forefoot, inducing knee-recurvatum. The physical examination exhibited a shortening of the right triceps surae (TS) muscle (ankle dorsiflexion was 0° with the knee flexed and −5° with the knee extended) as well as a spasticity of this muscle, with a modified Ashworth scale (MAS) score of 3 . The strength of the right tibialis anterior, extensor hallucis longus and extensor digitorum longus muscles was graded 3 on the Medical Research Council (MRC) scale . A motor nerve block of the nervus tibialis with lidocaine, targeting the soleus and tibialis posterior branches, was performed after the examination. The block allowed an improvement of the patient’s gait, as he recovered a plantigrade right foot during the stance phase. The knee-recurvatum was unchanged. After the block, the MAS of the TS was 1, the maximal ankle dorsi-flexion was 5° with the knee flexed and 0° with the knee extended.
Given the results of this evaluation, the patient was operated on his right leg on March 3rd 2011 (15 months post-trauma). The surgical procedure included a soleus lengthening (aponevrotomy) and a selective neurotomy of the following branches of the nervus tibialis: superior and inferior soleus nerves, tibialis posterior nerve. A partial muscular rupture of the soleus at the muscle/tendon junction was observed during the lengthening procedure.
After an immobilization period of 4 weeks, the patient was admitted in our outpatient rehabilitation unit in April 2011. His ankle dorsiflexion on the right side was 20° with the knee flexed and 15° with the knee extended. No spasticity was noticed in his TS, whereas moderate spasticity was noticed in his quadriceps femoris (MAS: 1+), adductors (MAS: 1+) and hamstrings (MAS: 1) . The strength of the muscles of the anterior compartment of the shank was 3 on the MRC scale and the strength of the TS was 1. The patient was able to walk, and the observational gait analysis findings were an increased ankle dorsiflexion and knee flexion during the stance phase on the right side. Four weeks later, the patient complained of sensation of instability of the right knee during fast gait. The observational gait analysis at fast speed revealed flexion/extension oscillations of the right knee during the stance phase and a stiff-knee gait (SKG). We hypothesized that the spasticity of the right rectus femoris muscle (RF), creating a clonus during stance, was responsible for the gait disorder in our patient. We tested this hypothesis by performing a motor nerve block of the right RF nerve and a botulinum toxin type A injection in the RF. Quantitative gait analysis was performed to assess each intervention.
A clinical and instrumental investigation (gait analysis) was performed three times for the patient:
- •
T1: on June 7th 2011;
- •
T2: on June 7th 2011, with the right RF nerve block;
- •
T3: on August 18th 2011, 6 weeks after the injection of botulinum toxin type A into the right RF.
Each investigation included the following assessments:
- •
clinical examination with observational gait analysis, manual muscle testing of the five pairs of lower limb ASIA/ISCOS score muscles as well as for the gluteus maximus and medial hamstrings, and spasticity assessment on the MAS for the gluteus maximus, adductors, vasti, RF (scaled by performing a Duncan-Ely test ) hamstrings, as well as for the ankle plantarflexors with the knee flexed and extended;
- •
kinematic study: after registration of the anthropometrics parameters, 16 retroreflective markers were placed on the patient’s pelvis and lower limbs skin following the Davis et al. protocol . A motion capture system with six optoelectronic cameras MX F40 (Vicon ® System, Oxford Metrics, Oxford, UK) was used. Following marker reconstruction, the 3D-angles of the lower limbs were calculated;
- •
electromyographic recordings (EMG): a wireless 10 channel EMG system (zero-wire, Aurion Ltd, Milan, Italy) was used for the dynamic muscular acquisition, which was simultaneous to the kinematic study. Five pairs of Ag/AgCl surface electrodes (Blue Sensor, Ambu ® , Denmark) were placed on each leg, with meticulous respect to the SENIAM recommendations . The RF, vastus medialis, medial hamstrings, tibialis anterior, and soleus muscles were recorded. The sample frequency of the EMG signal was 1000 Hz;
- •
gait protocol: during each session (T1, T2, and T3), 6 gait trials at the patient’s fastest walking speed with a cane were recorded;
- •
data analysis: the spatiotemporal parameters were obtained from the kinematic data using the method described by Desailly et al. . Regarding kinematic data, the mean curves driven from the cycles of the fastest walking trial were considered. The EMG signal recorded during the fastest cycle of the same trial was rectified and then analysed;
- •
gait variability assessment: the method described by Duhamel et al. was used to compute an intra-class correlation coefficient (ICC) for the hips, knees, and ankles’ flexion/extension kinematic curves of the different gait cycles of the analysed trial.
The RF nerve block was performed in the gait lab, with the patient lying supine. The cutaneous landmarks described by Sung et al. were used to determine the needle’s puncture point in the right thigh. An electrode needle (Stimuplex, B Braun ® , Germany), connected to a nerve stimulator (Stimuplex HNS 12, B Braun ® , Germany) was used. The precise targeting of the RF nerve was obtained through electrostimulation, with a specific, isolated contraction of the RF with a stimulation intensity lower than 0.5 mA as the target criterion. Three millilitres of 2% lidocaine were then injected around the RF nerve. The markers and surface electrodes were not removed during the block procedure.
The botulinum toxin type A injection into the right RF was performed 15 days after T1 and T2. Hundred units of onabotulinumtoxinA (Botox ® Allergan Inc, CA, USA) were injected in two points into the RF using an electrode needle (Ambu Neuroline Inject™, Ambu, Denmark) connected to a stimulator (Cefar Rehab X2 ® , DJO Global, CA, USA).
1.3
Results
The clinical examinations confirmed at T1 the abnormal, oscillating motion of the right knee with flexion/extension during the stance phase. Although to a lower extent, a similar motion was present in the left knee. These oscillations were suppressed at T2 and T3. The spasticity of the RF was rated 3 at T1, 1+ at T2 and 2 at T3, whereas the other muscles showed no change, neither for spasticity nor for strength, at the three different sessions. The clinical results are detailed in Table 1 .
| Pre-block | Post-block | Post-toxin | ||||
|---|---|---|---|---|---|---|
| R | L | R | L | R | L | |
| Spasticity (MAS) | ||||||
| Gluteus maximus | 1 | 0 | 1 | 0 | 1 | 0 |
| Adductors | 1 | 0 | 1 | 0 | 1 | 0 |
| Vasti | 1+ | 0 | 1+ | 0 | 1+ | 0 |
| Rectus femoris | 3 | 1 | 1 + | 1 | 2 | 1 |
| Hamstrings | 1 | 0 | 1 | 0 | 1 | 0 |
| Ankle plantar flexors (knee flexed) | 0 | 1 | 0 | 1 | 0 | 1 |
| Ankle plantar flexors (knee extended) | 0 | 1 | 0 | 1 | 0 | 1 |
| Strength (MRC testing) | ||||||
| Hip flexors | 3 | 5 | 3 | 5 | 3 | 5 |
| Gluteus maximus | 4 | 5 | 4 | 5 | 4 | 5 |
| Hamstrings | 3 | 4 | 3 | 4 | 3 | 4 |
| Knee extensors | 5 | 5 | 5 | 5 | 5 | 5 |
| Ankle dorsiflexors | 3 | 5 | 3 | 5 | 3 | 5 |
| Long toe extensors | 3 | 5 | 3 | 5 | 3 | 5 |
| Ankle plantar flexors | 1 | 5 | 1 | 5 | 1 | 5 |
The spatiotemporal gait parameters at T1, T2 and T3 are presented in Table 2 . The patient’s maximal gait speed increased between T1 and T2 and between T2 and T3, mostly because of an increase in step length, while the cadence was unchanged.
| Pre-block | Post-block | Post-toxin | |
|---|---|---|---|
| Speed (m/s) | 0.51 | 0.59 (+16%) | 0.71 (+39%) |
| Step length (m) | 0.73 | 0.87 (+19%) | 1.02 (+40%) |
| Cadence (steps/min) | 42.1 | 39.9 (−5%) | 41.9 (0%) |
Data from the EMG recordings of the right RF performed at T1, T2 and T3 are shown in Fig. 1 . At T1, the right RF exhibited a clonus (repetitive bursting activity) during the stance phase. Besides, an inappropriate activity of the RF in mid-swing was present. At T2 and T3, no burst was observed, but a prolonged activity during the stance phase. The abnormal RF activity in the swing phase was reduced. The same data were noticed for the left RF ( Fig. 2 ).
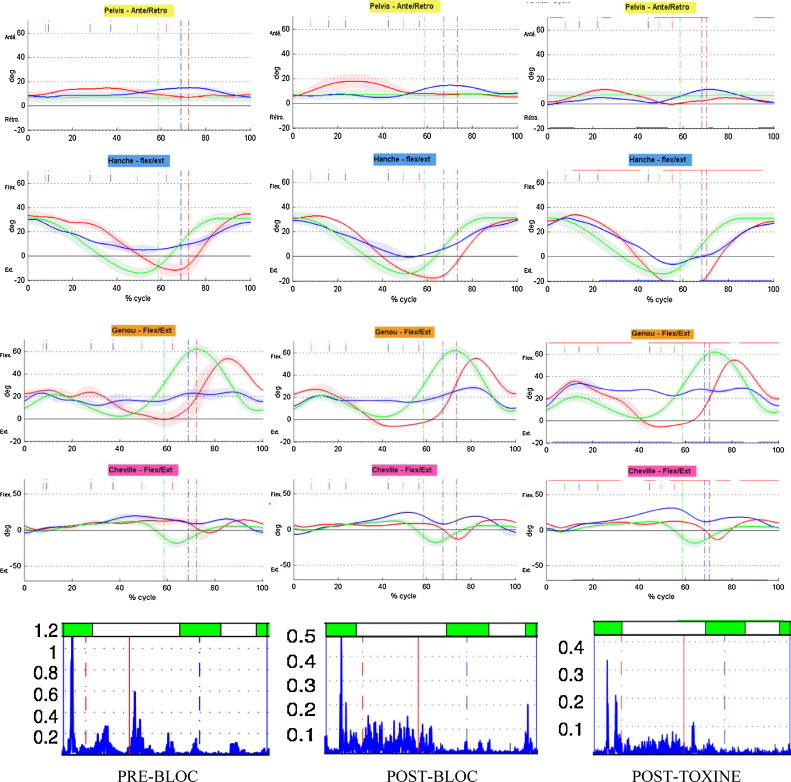
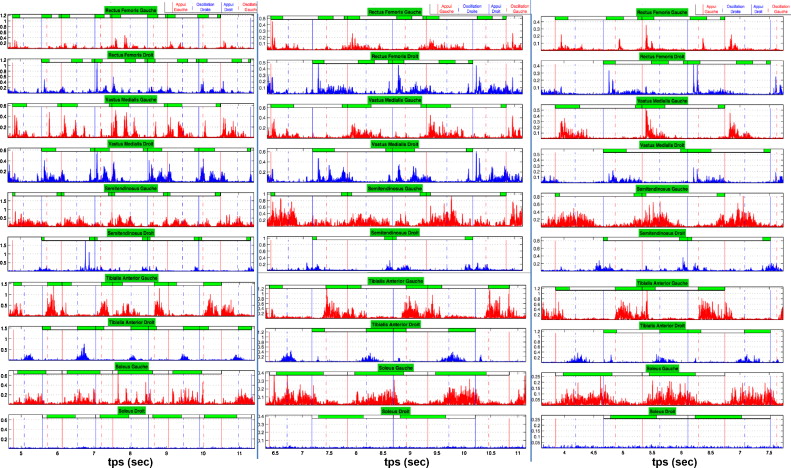
Kinematic data in the sagittal plane for the pelvis, hips, knees and ankles at T1, T2 and T3 are presented in Fig. 1 . At T1, the most significant abnormalities at the hips were an oscillating motion during the first half of the stance phase on both sides, and a limitation of the right hip extension in terminal stance. Both knees showed a weak loading response, followed by an oscillating flexion/extension motion during the stance phase, more marked on the right side. This right knee was also stiff during the swing phase (maximal flexion = 24.1°). The right ankle was plantarflexed at initial contact and excessively dorsiflexed in terminal stance. Almost no plantarflexion movement was present in the stance/swing transition, and the ankle quickly returned into plantarflexion in terminal swing. The left ankle presented an irregular, oscillating dorsiflexion during the stance phase.
At T2 and T3, the following changes were observed: the hips had a regular extension motion during the stance phase, and their extension in terminal stance was increased. The knees’ loading response was improved. Instead of the oscillating motion during the stance phase, an excessive right knee flexion was noticed, and the left knee turned into recurvatum in mid-stance. The right peak knee flexion in the swing phase was increased at T2 relative to T1 (28.6° vs. 24.1°), but not at T3.
Gait variability was low on the right side (ICC between 0.9 and 1) for the hips and ankles in all sessions, indicating good inter-cycle reproducibility of the movement of these joints. Conversely, the ICC was poor for the right knee at T1 (0.56), indicating high variability of its motion. Reproducibility was improved at T2 (ICC = 0.78) and T3 (ICC = 0.87) for this joint. In the left lower limb, reproducibility was good for the hip and knee in all conditions (ICC > 0.9), while the reproducibility was poor for the ankle at T1. It increased at T2 and T3 (ICC = 0.94).
1.4
Discussion
We present the situation and treatment of a patient with a BSPS whose gait disorder was characterized by a clonus of the RF during the stance phase, which appeared after a surgical procedure for a spastic equinus foot. Spasticity of the RF was responsible for an oscillation of the knee during the stance phase. The muscular and kinematic disorders in the stance phase have been identified by a gait analysis and corrected by a focal treatment of the spasticity of the RF (motor nerve block and botulinum toxin type A injection). The impact of these two interventions regarding gait improvement was very similar.
The role of the spasticity of the RF is well known in the post-stroke hemiplegic stiff-knee gait (SKG). Four studies showed an improvement of the SKG after diminution of the spasticity of the RF. Two studies assessed the effect of a RF nerve block and one study the effect of botulinum toxin type A injection into the RF . Roberson et al. studied the combination of both techniques . In their study, there was a correlation between the effectiveness of the nerve block and the effectiveness of the toxin injection. A moderate increase of peak knee flexion in swing was observed in our patient after the RF nerve block (+ 4.5°), but not after the toxin injection. Yet, the major increase of hip extension in terminal stance witnessed the increased extensibility of the RF after the toxin injection. It accounted for the increase of step length and gait speed at T3. In the case of our patient, other biomechanical disturbances were associated with the inappropriate activity of the RF during the swing phase. First, weak ankle plantarflexors were responsible for the lack of propulsion in pre-swing. Second, there was an insufficient hip flexion movement in the stance-to-swing transition, associated with weak hip flexors (MRC score: 3/5). These two deficiencies have been described in association with SKG , and the persistence of the SKG despite the diminution of the inappropriate RF activity during the stance phase in our patient could rely on these associated mechanisms. Furthermore, the dose of botulinum toxin that was injected (100 Botox ® units) was lower than the dose used in other studies (200 units) , which can participate in the absence of improvement of the patient’s SKG at T3.
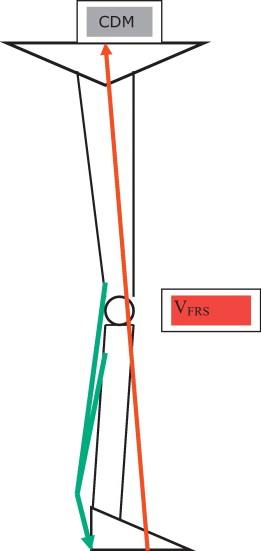
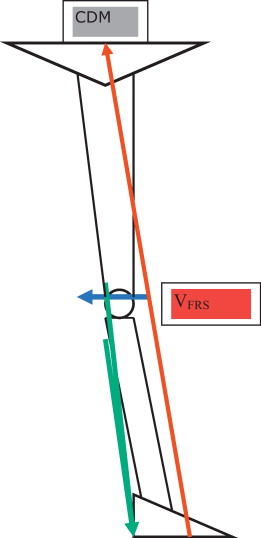
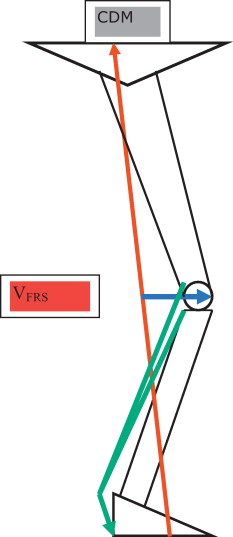
The involvement of the spasticity of the quadriceps in gait disorders during the stance phase, especially in knee recurvatum (KR), has been hypothesised . The first movement of the knee following initial contact is a flexion (weight acceptance), allowed by an eccentric contraction of the quadriceps. According to Perry’s hypothesis, in case of a spastic quadriceps, the response of this muscle to the loading response could overwhelm the normal absorption and induce a KR . No study to date confirmed this hypothesis, while studies by Nene et al. showed that the normal RF did not contract during the first half of the stance phase . The role of the spasticity of the quadriceps in KR remains therefore to be demonstrated. In the absence of a true KR, our patient presented with a knee oscillation during the stance phase at fast speed. This instability was due to the spasticity of the RF, as attested by the effectiveness of the RF nerve block and botulinum toxin injection. The onset of this gait disorder after a surgery associating a selective tibial neurotomy and TS lengthening indicates an associated responsibility of the weakness of the TS in this disorder. The TS has a key-role in the stabilization of the knee during the stance phase, a phenomenon known as the plantar flexion/knee extension (PFKE) couple . Its hallmark is the eccentric contraction of the ankle plantarflexors (principally the soleus) during the first part of midstance, which controls the progression of the ground reaction force (GRF) over the stationary foot. This mechanism allows the GRF vector to pass in front of the knee and therefore to create a knee extensor moment that stabilizes the knee during midstance without any need for a quadriceps contraction ( Fig. 3 ). In case of insufficient ankle dorsiflexion during the stance phase (for example, due to TS spasticity), the lack of forward progression of the tibia during the first half of midstance creates an excessive knee extensor moment and therefore a KR ( Fig. 4 ). This mechanism has been put forward by many authors to explain KR in hemiplegic patients . Conversely, in case of weak TS, the progression of the tibia during midstance becomes excessive, leading to a strong knee flexor moment ( Fig. 5 ). Such a mechanism has been described in the child with diplegic cerebral palsy after Achilles tendon lengthening, which in some cases could lead to crouch gait . Our patient probably presented such a gait disorder after the surgery that he underwent for his spastic foot. This surgery initially resulted in weak TS. At fast speed, the brisk knee flexion after initial contact, created by the excessive progression of the tibia, was amplified and the rapid stretch of the quadriceps triggered a clonus of the RF. This latter was responsible for a knee oscillation. The responsibility of the spasticity of the RF was confirmed by the disparition of the clonus during the RF nerve block and after the botulinum toxin injection. Furthermore, the kinematic and EMG analysis displayed that the oscillation and clonus were bilateral, although less marked on the left side, in our patient. We hypothesize that the clonus of the right RF induced an oscillation of the entire right lower limb, which was transmitted to the left limb during the double support. In this spastic left limb, this oscillation also caused a clonus. It is worthwhile that the block and toxin injection, performed on the right side, allowed a bilateral extinction of the clonus and oscillation, although the spasticity of the left RF was not modified by the block ( Table 1 ). This bilateral effect of a unilateral treatment could be explained by an improved stability and by a reduction of the oscillations on the left thanks to the extinction of the clonus on the right side. In this case study, the right RF muscle appears to be the “trigger muscle” of a clonus of both quadriceps.
The first line treatment of our patient’s gait disorder is questionable. The strengthening of the TS could help improve the ankle control and the excessive dorsiflexion during the stance phase. A ground reaction force ankle foot orthosis could temporarily compensate the TS weakness. We chose to propose to our patient the focal treatment of the spasticity of the RF in order to rapidly improve his ability to walk at fast speed, without ruling out the other possibilities.
This case illustrates the interest of gait analysis in the diagnostic and therapeutic approaches of complex gait disorders. Gait analysis is a precious tool to evidence the kinematic disorders and match them with EMG abnormalities. It also allows the objectification and quantification of changes induced by a test or by a treatment.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
Le syndrome médullaire de Brown-Séquard (BSS), ou syndrome d’hémisection de moelle, a été initialement décrit en 1851 dans le contexte d’une plaie de la moelle spinale par arme blanche . Il associe, du côté de la lésion médullaire, un déficit moteur par atteinte du tractus corticospinal et des troubles proprioceptifs et, du côté controlatéral, une anesthésie thermo-algique. En pathologie spinale traumatique, ce syndrome est extrêmement rare dans sa forme pure . Plus récemment a été introduit le concept de syndrome de Brown-Séquard plus (BSPS). Celui-ci correspond à une lésion médullaire incomplète responsable en sous-lésionnel d’une atteinte bilatérale, avec prédominance des troubles moteurs et des troubles proprioceptifs d’un côté et prédominance controlatérale des troubles de la sensibilité thermo-algique . Les BSPS représenteraient 2 à 4 % des syndromes médullaires identifiés après traumatisme vertébromédullaire . Leur évolution se fait dans plus de trois quarts des cas vers la reprise d’une marche fonctionnelle . Cependant, ces patients présentent fréquemment un trouble de la marche marqué par une spasticité délétère du membre inférieur le plus déficitaire. Ces situations de troubles complexes de la locomotion méritent une évaluation précise pouvant aboutir à des indications thérapeutiques ciblées. Dans l’hypothèse du bénéfice d’un traitement focal de la spasticité, l’utilisation de tests anesthésiques (blocs moteurs) ainsi que le recours à l’analyse quantifiée de la marche (AQM) semblent constituer des moyens utiles dans la prise en charge de ces patients . À partir de l’observation d’un patient BSPS, nous soumettons l’intérêt de l’utilisation combinée de ces deux explorations.
2.2
Patient et méthodes
Un sujet masculin de 53 ans a été victime le 10 décembre 2008 d’un traumatisme vertébromédullaire par chute d’une hauteur de 3 m sur son lieu de travail, responsable d’une tétraplégie incomplète AIS C spastique de niveau moteur C8 droit, C5 gauche, et de niveau sensitif C6 droit, C4 gauche. Le score ASIA moteur initial était de 32 aux membres supérieurs et 30 aux membres inférieurs . Le bilan lésionnel a mis en évidence une fracture de C7, traitée chirurgicalement (ostéosynthèse par voie antérieure). Le patient a été pris en charge dans notre service de MPR neurologique à six semaines du traumatisme. Au terme de la phase de rééducation/réadaptation ayant duré huit mois, la situation neurologique a évolué vers un tableau de tétraplégie incomplète AIS D de niveau moteur C8 droit, C7 gauche, de niveau sensitif C4, spastique, réalisant un syndrome de Brown-Séquard-plus droit. En effet, le syndrome pyramidal déficitaire sous-lésionnel était bilatéral, avec prédominance droite ( Tableau 1 ), de même que les troubles de la sensibilité profonde. En revanche, le déficit sensitif à la piqûre prédominait à gauche. Le score ASIA moteur était de 43 aux membres supérieurs et 39 aux membres inférieurs. En septembre 2009, le patient a regagné son domicile, autonome pour toutes les activités de vie quotidienne, avec un périmètre de marche de 500 m à l’aide une canne anglaise portée à gauche. Douze mois plus tard, il s’est plaint d’une dégradation de la marche. L’examen a alors objectivé un trouble de la marche en lien avec un pied varus équin spastique droit avec griffe des orteils. Le contact initial et l’appui à droite se faisaient sur l’avant-pied. Le genou droit passait systématiquement en recurvatum pendant la phase d’appui. À l’examen analytique, on mettait en évidence une rétraction du soléaire et des gastrocnémiens (flexion dorsale de cheville genou fléchi : 0° et genou tendu : −5°), une spasticité marquée du triceps sural (TS) droit avec un score de 3/4 sur l’échelle d’Ashworth modifiée . La motricité volontaire du tibial antérieur, de l’extenseur propre de l’hallux et de l’extenseur commun des orteils était cotée à 3 selon le score MRC . Un bloc moteur à la lidocaïne, portant sur les branches du nerf tibial droit destinées au soléaire et au tibial postérieur, a été réalisé pendant la consultation. Ce bloc a permis une amélioration de la marche, l’appui devenant plantigrade. Le recurvatum de genou, en revanche, persistait. Le score d’Ashworth modifié est passé de 3/4 à 1/4 sur le TS. La flexion dorsale maximale de cheville en passif est passée de 0° à 5° genou fléchi et de −5° à 0° genou tendu.
| Pre-bloc | Post-bloc | Post-toxine | ||||
|---|---|---|---|---|---|---|
| D | G | D | G | D | G | |
| Spasticité (MAS) | ||||||
| Grand fessier | 1 | 0 | 1 | 0 | 1 | 0 |
| Adducteurs | 1 | 0 | 1 | 0 | 1 | 0 |
| Vastes | 1+ | 0 | 1+ | 0 | 1+ | 0 |
| Droit fémoral | 3 | 1 | 1 + | 1 | 2 | 1 |
| Ischio-jambiers | 1 | 0 | 1 | 0 | 1 | 0 |
| Fléchisseurs plantaires de cheville (genou fléchi) | 0 | 1 | 0 | 1 | 0 | 1 |
| Fléchisseurs plantaires de cheville (genou tendu) | 0 | 1 | 0 | 1 | 0 | 1 |
| Force (testing MRC) | ||||||
| Fléchisseurs de hanche | 3 | 5 | 3 | 5 | 3 | 5 |
| Grand fessier | 4 | 5 | 4 | 5 | 4 | 5 |
| Ischio-jambiers | 3 | 4 | 3 | 4 | 3 | 4 |
| Extenseurs de genou | 5 | 5 | 5 | 5 | 5 | 5 |
| Fléchisseurs dorsaux de cheville | 3 | 5 | 3 | 5 | 3 | 5 |
| Extenseur propre de l’hallux | 3 | 5 | 3 | 5 | 3 | 5 |
| Fléchisseurs plantaires de cheville | 1 | 5 | 1 | 5 | 1 | 5 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







