Unlinked Elbow Arthroplasty
Tim Cresswell
David Stanley
INTRODUCTION
Total elbow arthroplasty began in the early 1940s when Boerema and de Waard reported their experience of using a single axis metallic hinge arthroplasty for elbow reconstruction (1). Following this early experience, other hinge arthroplasties were designed, and although all demonstrated encouraging early results, loosening, predominantly on the humeral side of the joint, was soon recognized as a significant complication. Because of this early experience, some designers began to look at the possibility of resurfacing elbow arthroplasties in the hope that this would result in fewer complications. This type of implant required minimal bone resection, and most of the early designs lacked intramedullary stems. The stability of the components depended on accurate implant orientation and appropriate soft-tissue tensioning. They included the Wadsworth (2), Lowe-Miller (3), and original Kudo implant (4). However, rigid fixation of unstemmed humeral components proved difficult to achieve. Failure, because of the posteriorly directed resultant forces across the elbow joint, resulted in loosening and posterior displacement of the humeral component, or fracture of the bone at the bone-implant interface.
The addition of a humeral stem took unlinked arthroplasties into the modern era. The Souter-Strathclyde replacement, capitellocondylar implant designed by Ewald, and the Kudo Type V arthroplasty are perhaps the most frequently used unlinked arthroplasties at the present time (Fig. 22-1). These modern designs have significantly improved the quality of life for many patients suffering with disabling elbow disorders. They have enabled the elbow surgeon to treat the severely damaged elbow joint with the expectation that the patient’s pain will be significantly reduced, often becoming pain free. In addition,
some improvement in flexion and extension is usually also achieved. This reduction in pain and increase in the flexion-extension arc of the elbow frequently will improve the function of the entire extremity.
some improvement in flexion and extension is usually also achieved. This reduction in pain and increase in the flexion-extension arc of the elbow frequently will improve the function of the entire extremity.
 Figure 22-1 Unlinked elbow replacements. A: The Souter-Strathclyde implant. B: The capitellocondylar implant. C: The Kudo implant. |
Indications
The indications and contraindications for unlinked total elbow arthroplasty are listed in Table 22-1. Unlinked total elbow arthroplasty is most frequently used for the treatment of rheumatoid arthritis. In addition, it can be used for posttraumatic arthritis, degenerative arthritis, elbow ankylosis, and some distal humeral fractures.
The primary indication for the use of an unlinked total elbow arthroplasty is to treat elbow pain associated with disabling elbow disease. Secondary indications include the desire to improve elbow function. Although elbow arthroplasty should never be undertaken primarily to improve elbow motion, some improvement in the arc of flexion and extension is often achieved with a successful total elbow replacement. Unlinked elbow arthroplasty has been used in patients with an unstable elbow resulting from severe bone loss secondary to rheumatoid arthritis or selected cases of distal humeral fractures. However, because a successful result is dependent on appropriate bone and soft-tissue support, it is our experience that the use of an unlinked total elbow replacement in these circumstances is less reliable than the use of a linked total elbow replacement. As such, it is our view that unlinked arthroplasty is most suitable for patients with debilitating pain and loss of function but in whom there is reasonable bone preservation and elbow joint stability.
TABLE 22-1 INDICATIONS AND CONTRAINDICATIONS FOR UNLINKED TOTAL ELBOW REPLACEMENT | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||
Contraindications
Sepsis around the elbow is an absolute contraindication to elbow arthroplasty. Relative contraindications to unlinked elbow arthroplasty include those conditions where compromise of the bone or soft-tissue stabilizers may develop as a result of the surgical procedure or develop in the postoperative period. These conditions include takedown of an elbow arthrodesis or pain-free ankylosis, neuropathic elbow, muscle paralysis of the biceps or triceps, and excision of heterotopic bone. Young patients who want to remain physically active will wear the implant at an accelerated rate and should only be considered for arthroplasty if alternative therapies have been attempted or the patient agrees to curtail physical activity.
IMPLANT CONSIDERATIONS
Although unlinked, the degree of constraint between the humeral and ulnar components of the arthroplasty varies in different designs. The Souter-Strathclyde prosthesis reproduces, as closely as possible, the normal anatomic shape of both the distal humerus and proximal ulna to create normal elbow biomechanics (5). The humeral component is designed to transmit forces to the proximal humerus via the supracondylar ridges and side flanges of the prosthesis that provide maximal lateral and medial fixation, thereby resisting the forces that predispose to loosening of the arthroplasty.
The capitellocondylar implant is a shell-fit prosthesis with an intramedullary humeral stem (6). It allows eccentric tracking of the ulna around the trochlea as the instant centers of motion change. This together with the unlinked nature of the components reduces the torsional and distraction-compression forces that act on the humeral cement-bone interface.
The Kudo Type V implant is the least constrained of these three arthroplasties. It consists of a saddle-shaped humeral component with a reciprocal ulna. The shape allows translation of the ulna component across the humeral surface during flexion and extension.
EVALUATION
Clinical Evaluation
The assessment of a patient who is being considered for elbow arthroplasty must include a full history and physical examination. Details of the patient’s elbow pain should be recorded including the presence of pain at rest, during activities, and at night. It is also important to ask specifically as to whether there are neurologic symptoms affecting the arm and hand. The presence of active or previous elbow discharge or sepsis must also be recorded. Questions regarding the stability of the elbow are also essential because consideration may need to be given to the use of a linked arthroplasty. Finally, a social history should be taken to determine that the patient has realistic expectations regarding the results of total elbow arthroplasty.
In addition to clinically examining the elbow joint for range of movement, swelling, and stability, it is also important to examine the ipsilateral shoulder, wrist, and hand to be certain that a total elbow arthroplasty is appropriate treatment.
A neurologic examination is essential. Particular reference to the function and position of the ulnar nerve is mandatory.
Radiologic Evaluation
In our institution anteroposterior and lateral radiographs of the elbow joint are performed and examined not only for the degree of arthritic change affecting the joint but also for the degree of bone loss and the size of the medullary canal (Fig. 22-2). Patients with rheumatoid arthritis with severe bone loss on the humeral side of the joint may not be suitable for an unlinked arthroplasty, whereas on the ulnar side of the joint, erosion and loss of bone imply that particular care will be necessary to avoid a fracture to the ulna during bone preparation.
Radiographic assessment of the size of the medullary canal is helpful preoperatively in giving an indication as to the most likely implant size that will be used. Rarely do we find it necessary to undertake additional radiographic views or perform other imaging studies such as computed tomography.
SURGICAL APPROACHES
Total elbow arthroplasty is normally performed through a posterior approach to the elbow joint. In the past, an extended Kocher lateral approach to the elbow joint has been used, but this has the disadvantage that the ulnar nerve is not visualized and is therefore potentially at greater risk of injury during the procedure.
Several posterior surgical approaches have been described, all of which involve either splitting or reflecting the triceps muscle.
Triceps Splitting
In 1932 Campbell (8) described a posterior approach to the elbow in which the distal humerus and olecranon were exposed by splitting the triceps and reflecting it medially and laterally. The dissection was continued subperiosteally with reflection of the anconeus muscle laterally and the flexor carpiulnaris muscle medially.
In 1940 Van Gorder (9) described a technique whereby an inverted V-shaped flap of the triceps aponeurosis was
dissected and reflected distally. The muscle fibers of the triceps were then split in the midline and reflected, enabling exposure of the elbow joint. This approach remains popular with many elbow surgeons undertaking total elbow arthroplasty.
dissected and reflected distally. The muscle fibers of the triceps were then split in the midline and reflected, enabling exposure of the elbow joint. This approach remains popular with many elbow surgeons undertaking total elbow arthroplasty.
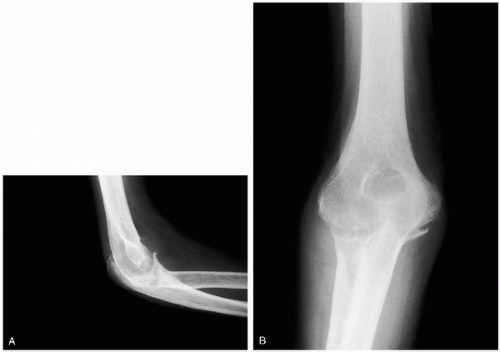 Figure 22-2 A: An anteroposterior and B: lateral radiograph of a patient preoperatively with rheumatoid arthritis. Assessment is made of the degree of arthritic change affecting the joint, the degree of bone loss, and the size of the medullary canal.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





