Ultrasound and Alternative Imaging Outcomes
Helen I. Keen
Paul Emery
Philip G. Conaghan
Osteoarthritis (OA) is increasingly common in our aging society. Cartilage is not the only anatomic structure involved in the disease: the capsule, ligaments, synovial membrane, and subchondral bone can all be affected in this disease. Consequently it is likely that specific imaging modalities will have benefits for imaging components of the OA process.
Recent years have seen an exciting increase in clinical trials investigating the role of potential disease modifying OA drugs. While the current body of evidence remains inconclusive about the disease modifying properties of these drugs, there is a suggestion that structure modification is potentially measurable.1 Conventional radiography (CR) has largely been the imaging technique utilized to assess and monitor temporal changes in these and previous OA trials, utilizing joint space narrowing as the outcome. CR is, however, far from an ideal assessment of disease status and outcome measure. It is well documented that clinical symptoms do not correlate with CR changes in OA,2,3,4 which is explained by multiple factors. Firstly, joint space narrowing which is characteristic of OA on CR is a surrogate measure of cartilage thickness, and really reveals little about cartilage integrity. In addition, CR produces a two-dimensional image of a three-dimensional structure and provides limited information about soft tissue and composite joint structures, including synovial membrane, synovial fluid, the capsule, and ligaments. A further disadvantage of CR is that exposure to ionizing radiation is undesirable in trials that require serial imaging to monitor temporal changes. In addition, the validity of CR in monitoring changes in joint space narrowing over time has also been questioned, particularly in these recent drugs (DMOAD) studies. It is hypothesized that pain modification in OA may affect the positioning of joints when radiographs are taken, hence altering the apparent joint space narrowing.1 In addition, radiographs provide no information about the metabolic activity of the joint, or presence or absence of inflammation, which might be vital to understanding the process of OA and the effects of DMOAD drugs. No doubt that future studies are planned to build on this foundation of structure modification in OA, and it is likely alternative imaging techniques will be utilized in order to further understand the disease and the effects of drugs, and monitor disease progression. Recent decades have seen much progress in validating and investigating the role of novel imaging techniques, such as ultrasonography, magnetic resonance imaging (MRI), computer tomography (CT), optical coherence tomography, and scintigraphy in OA. This chapter will focus on the use of novel imaging techniques (with the exception of MRI which, has been covered elsewhere) in understanding, diagnosing, and managing OA.
Ultrasonography
How it Works
Ultrasound (US) utilizes the principle of sound waves reflecting off matter to the source of origin in order to produce an image. Sound waves travel at varying speeds through different matter and are reflected (as echoes) from the interface of materials with differing densities. The reflectivity of an interface is greatest when the two opposing tissues consist of very different properties; for example,
the interface between fat and bone will be highly reflective, allowing good visualization of the surface by US imaging.
the interface between fat and bone will be highly reflective, allowing good visualization of the surface by US imaging.
The development of “B mode” ultrasonography allowed this technique to be applied to medicine. “B mode” ultrasonography produces two-dimensional images in shades of gray: echoes returning to the source are displayed as pixels in varying shades of brightness to produce a picture in gray scale. The pixel brightness is in proportion to the intensity of the echo. Doppler technique can be added to gray scale to provide information about the vascularity of the tissue being imaged. Doppler ultrasonography utilizes the principle that the echo frequency is altered when reflected off moving objects. This principle can be applied to musculoskeletal US as color Doppler or power Doppler (PD). PD displays the amplitude of the Doppler signal as a color spectrum, providing information only about the power of the signal, but is sensitive to low flow. Color Doppler displays the range of frequencies reflected as color, encoding both velocity and directional information. In musculoskeletal imaging, the direction and velocity of vascular flow is often less important than the amplitude of the flow, so PD is the more commonly applied technique in this field.
US Detectable Abnormalities in Osteoarthritis
Utilizing gray scale and PD techniques, US can provide information about the integrity of several structures within the osteoarthritic joint including cartilage, integrity of cortical bone, presence of joint effusions, and synovial hypertrophy. The vascularity of structures can also be assessed, which generally reflects the degree of inflammation.
Cartilage
Animal and in vitro models have been used to demonstrate that US is reliable in measuring cartilage thickness and identifying focal chondral defects.5,6 US has also been shown to provide qualitative information on cartilage morphology and document real-time change in cartilage in animal models of arthritis.7
Imaging of articular cartilage in vivo with noninvasive US techniques is more challenging than in animal and cadaveric models, due to problems of getting adequate visualization of chondral surfaces. When articular cartilage is able to be visualized, general sonography features of osteoarthritic cartilage include loss of normal sharpness of synovial-cartilage interface, loss of clarity of the cartilaginous layer, thinning of joint cartilage, and increased intensity of the posterior bone cartilage interface.8 While Grassi has demonstrated that articular cartilage can be visualised at the knee, hip, shoulder, elbow, and metacarpal phalangeal joints, with characteristic changes identifiable, the extent on information gathered is dependent on the size of the acoustic window.8 For example, while a portion of articular cartilage can be visualized at the hip joint, this is usually not the weight-bearing portion, which is most likely to be affected in OA.
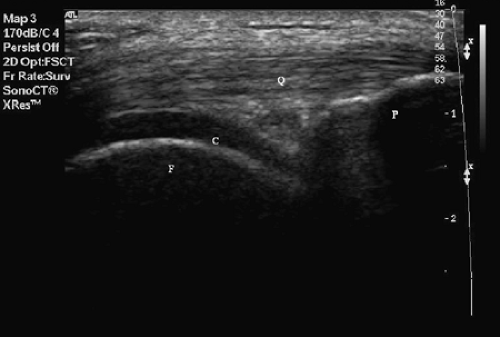
However, the reproducibility and precision of using US to determine cartilage thickness compared to MRI and CR has been shown to be good in OA knees,9,10,11 and correlate with diagnosis in OA and controls.10 The correlation between US and MRI cartilage thickness was not good in normal controls in one study, but this only looked at small numbers.9 The sharpness and clarity of cartilage on US has correlated with OA or no OA9 and good correlation with MRI. The clinical significance of imaging articular cartilage at the knee (Figures 10-1A and 10-1B) is uncertain given that weight-bearing portions are unable to be demonstrated reliably.
Bone Changes
Bone is highly echogenic, and the cortical surface is able to be visualized easily with US, as long as an acoustic window is present. General changes detectable with US in OA include bone irregularity and erosions, osteophytes, subchondral bone cysts, decreased joint space, and subluxation of joint surfaces.12,13,14,15,16
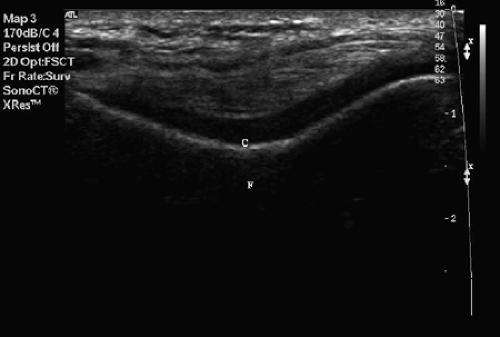 Figure 10-1B Longitudinal US of the distal femur showing articular cartilage. F = distal femur; C = articular cartilage. |
Synovial Inflammation
Many studies have demonstrated the ability of US to detect synovial hypertrophy and joint effusions, common features of OA.17 The European league against rheumatism (EULAR) study of 600 OA knees demonstrated that knee synovitis or effusions are common; 47% of patients with painful knee OA had either synovitis, effusion, or both on US, with the presence of joint effusion alone being most common (30%). It also demonstrated that in OA of the knee, US is more sensitive to their presence than clinical examination.17 The study findings are consistent with other studies, whereby US is more sensitive to the presence of synovial effusion than clinical examination.18,19,20 Further analysis of the EULAR study found that a formula to allow clinical recognition of inflammation in OA could not be derived, demonstrating that imaging is a more useful method of detecting joint inflammation than clinical pathways.21
The reliability of US in detecting effusions and synovial hypertrophy has been validated against CT, MRI, and histopathology at the knee joint9,10,22,23 and AC joint.15 US has been shown to demonstrate the presence of effusions in OA at the carpometacarpal joint and shoulder joint.14,24
PD technique has been utilized in rheumatology in addition to gray scale to document soft tissue vascularity, which has been demonstrated to reflect inflammatory activity in inflammatory arthritis.25,26,27 The use of PD in OA has been validated against histopathology in the knee and hip,25,28 and has been shown to demonstrate improved differentiation of intra-articular structures compared to gray scale in OA of the knee.23
US Contribution to Improved Understanding of Osteoarthritis
As mentioned previously, symptoms of OA do not correlate with CR changes.2,3,4 The use of US to image OA has increased our understanding of the structural changes in this disease and their relationship with symptoms. In a study of knee OA, the degree of MRI and US detected cartilage changes, synovial hypertrophy and popliteal cysts increased as radiographic grade increased. In addition, cartilage abnormalities were more common in those with osteophytes.9 This is in keeping with a study in which the presence of popliteal cysts correlates with grade of OA,29 suggesting that radiographic grade does reflect the severity of the disease in OA knee.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree