Ulnar-sided wrist pain can be a challenging entity for the hand surgeon and even more so in the athletic population. The authors present 8 causes of ulnar-sided wrist pain in an athlete (hook of hamate fracture, pisiform fracture, hypothenar hammer syndrome, triangular fibrocartilage complex injuries, ulnocarpal impaction syndrome, lunotriquetral ligament tears, extensor carpi ulnaris tendinitis, subluxation of extensor carpi ulnaris) and their associated imaging and treatment options.
Key points
- •
The athlete can present an interesting clinical challenge due to the overlap between acute injury and susceptibility to overuse phenomena from repetitive activities experienced during athletic pursuit.
- •
Although most of the entities described in this section are found among all patient groups, their treatment may differ in an athlete due to sport-specific considerations, temporal restraints, and outside influences on the athlete (coaching staff/trainers/recruiters).
- •
Thoughtful consideration of all of these factors will lead to a more satisfying outcome for the athlete with a goal of a safe and expedient return to sports activities.
Introduction
Management of hand and wrist injuries in the athlete can be a challenge and requires a good assessment of sport-specific athletic demands and the degree of impairment incurred by the athlete. Conservative management consisting of splints, medications, and therapy is beneficial in many cases; however, more definitive intervention is sometimes necessary to alleviate pain and preserve athletic function. The focus of this section is common ulnar-sided wrist conditions and injuries sustained in athletes. Many of the conditions outlined in this article can present as a result of participation in a variety of sports and occupational pursuits and as a normal consequence of physical training. Successful management often requires a thoughtful blending of treatment modalities for this unique class of patients.
Introduction
Management of hand and wrist injuries in the athlete can be a challenge and requires a good assessment of sport-specific athletic demands and the degree of impairment incurred by the athlete. Conservative management consisting of splints, medications, and therapy is beneficial in many cases; however, more definitive intervention is sometimes necessary to alleviate pain and preserve athletic function. The focus of this section is common ulnar-sided wrist conditions and injuries sustained in athletes. Many of the conditions outlined in this article can present as a result of participation in a variety of sports and occupational pursuits and as a normal consequence of physical training. Successful management often requires a thoughtful blending of treatment modalities for this unique class of patients.
Hook of hamate fractures
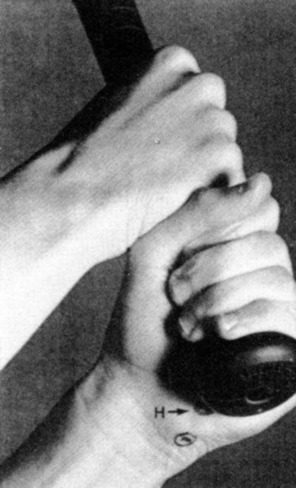
Although hamate hook fractures represent only 2% to 4% of all carpal fractures, they are frequently seen in racket sports as well as golf, baseball, and hockey. Hamate hook fractures are thought to be caused from a direct blow sometimes seen after grounding a golf club or during a check swing in baseball ( Fig. 1 ). These fractures can be further subdivided by identifying them as tip, waist, or body fractures. Hamate fractures are notoriously poor healers with waist and tip fractures progressing to nonunion most commonly secondary to poor vascularity. Because these injuries may be difficult to diagnose, hamate hook fractures must be suspected in athletes with ulnar-sided wrist pain competing in racquet or club sports.
Examination Findings
Patients may complain of pain over the hypothenar eminence and hamate hook and pain with resisted flexion of ring and small finger. In chronic cases, ulnar nerve dysfunction or crepitus with ring and small finer motion may be detected.
Imaging
Radiographic visualization of a hamate hook fracture can be difficult even with oblique and carpal tunnel views. Computed tomography (CT) is the image modality of choice when a hamate hook fracture is suspected ( Fig. 2 ).

Treatment
Although acute nondisplaced fractures can be managed with cast immobilization, athletes should be counseled regarding the poor healing rate and prolonged immobilization, and that even after lengthy immobilization, they may still require surgery. Most investigators recommend fracture excision for displaced or nonunited fractures. Excision has been shown to have no adverse effect on grip strength or wrist range of motion. Complications of hook of hamate fractures can include ulnar neuritis, flexor tendon irritation and rupture, ulnar artery thrombosis, and most commonly, symptomatic nonunion.
Pisiform fractures
In athletes, pisiform fractures commonly occur from a direct blow. A more rare mechanism is an avulsion fracture from a sudden contraction of the flexor carpi ulnaris, which surrounds the pisiform. Pisiform fractures make up about 2% of carpal fractures and are usually described as parasagittal, transverse, comminuted, and pisiform-triquetral impaction fractures.
Examination Findings
Presenting symptoms usually include pain directly over the pisiform or hypothenar eminence along with occasional ulnar nerve irritation.
Imaging
Visualizing the fracture on plain radiographs is difficult, but a 30° supinated view, 45° supinated oblique view, carpal tunnel view, or a CT scan may be necessary ( Fig. 3 ).
Treatment
Nondisplaced fractures typically heal with cast immobilization. Displaced and comminuted fractures are typically treated with pisiform excision with reliable pain relief and no loss of motion.
Hypothenar hammer syndrome
Hypothenar hammer syndrome (HHS) is a vascular phenomenon that results typically from repetitive blunt trauma to the hypothenar hand where the relatively unprotected ulnar artery remains superficial as it exits Guyon canal. Although HHS has classically been described in the dominant hand of middle-aged male workers who habitually use the ulnar palm as a tool to hammer objects, it has also been reported in athletes participating in a variety of sports, including baseball, golf, tennis, biking, and lifting. The pathophysiology of HHS is related to trauma to the ulnar artery as it travels around the hook of the hamate, with the hook acting as an “anvil” upon which the artery may be impacted. It is accepted that HHS symptoms occur secondarily as a result of thrombosis with or without embolic events.
Examination Findings
Ischemia in the ulnar digits of the hand associated with hypothenar callus, cold sensitivity, paresthesias, and pain are common findings. Other findings may include hamate hook fracture and ulnar tunnel syndrome. The Allen test and Doppler ultrasound are clinically useful to evaluate the patency of the ulnar artery and superficial palmar arch.
Imaging
Imaging may be accomplished with ultrasound; however, angiography is the accepted standard for definitively establishing the diagnosis of HHS and localizing the site of occlusion or aneurysm ( Fig. 4 ).
Treatment
Nonsurgical treatment is aimed at avoiding repetitive insults in episodically symptomatic patients. Calcium channel blockers and oral sympatholytics have been shown to be equally effective in this subset of patients. Thrombolysis can also be attempted if the onset is acute enough for a chance of success. Recombinant tissue plasminogen activator is commonly used for this purpose via intra-arterial administration. Surgery is the only treatment that will prevent recurrence of emboli and decompresses the adjacent neurologic structures. Surgical options include ligation of the ulnar artery if a complete radial arch exists. Excision of the damaged artery and reconstruction with an interposition vein graft is more common. Because there appears to be a subset of the population that is inherently susceptible to developing HHS, prevention is accomplished by ensuring athletes wear proper protective equipment and are taught proper grip techniques.
Triangular fibrocartilage complex injuries
Triangular fibrocartilage complex (TFCC) injuries are common in athletes and may result from repetitive load bearing and rotational stresses seen in sports such as tennis, golf, hockey (from impact with the boards in slap shots, resulting in hypersupination), lacrosse, gymnastics, golf, boxing, waterskiing (from traction injury), and pole vaulting. The TFCC is an important stabilizer of the distal radioulnar joint (DRUJ) and load absorber of the wrist. The TFCC is composed of a central articular portion that is avascular and a peripheral ligamentous portion that is a stabilizer of the DRUJ. This peripheral portion is more vascular and has a healing capacity ( Fig. 5 ).
Examination Findings
Ulnar-sided wrist pain in the athlete may be vague and associated with tenderness in the foveal area along with occasional clicks and pops.
Imaging
Imaging studies should include posteroanterior (PA) zero rotation view (with the shoulder abducted 90° and elbow flexed 90°), clenched fist pronation PA view, and contralateral views to assess ulnar variance and which may impact treatment decisions if ulnocarpal abutment is suspected. Although MRI arthrography is the definitive imaging modality of choice, it is associated with interpretative difficulty, and findings must be viewed in context of the clinical history and physical examination.
Treatment
If the DRUJ is unstable, early intervention with arthroscopy and peripheral TFCC repair is indicated. If the DRUJ is stable with continued symptoms for 2 to 3 weeks, arthroscopy may be indicated.
TFCC tears are broadly classified as either traumatic (class 1) or degenerative (class 2). Traumatic tears from a fall on the outstretched hand are most commonly noted in young athletes. These tears are generally amendable to arthroscopic debridement (central tears) or repair (peripheral tears). Arthroscopic central debridement is associated with 90% good-to-excellent results and allows early return to activity in 1 to 2 months ( Figs. 6 and 7 ). Peripheral repairs are performed via several different effective techniques and protected in a Muenster cast for at least 6 weeks followed by therapy and strengthening. Return to sport occurs in 3 to 4 months with 90% good-to-excellent results.








