Abstract
Objective
Reporting clinical and electrodiagnostic characteristics of sport-related ulnar neuropathies at the wrist.
Patients and methods
Eight sport-related and 45 non-sport-related cases from 53 ulnar neuropathies at the wrist cases over 14 years.
Results
Sport-related ulnar neuropathies at the wrist cases were due to cycling (5 cases), kayaking (2 cases), and big-game fishing (1 case). No patient had sensory complaints in ulnar digits, and all had motor impairment. Conduction across the wrist with recording on the first dorsal interosseous muscle was impaired in all cases, with conduction block in 5. Two cyclists showed bilateral ulnar neuropathies at the wrist. All cases recovered within 2 to 6 months with sport discontinuation. Distal lesions of the deep motor branch were more frequent in sport- than non-sport-related cases.
Conclusions
The 8 sport-related ulnar neuropathies at the wrist cases involved the deep motor branch. Conduction study to the first dorsal interosseous muscle across the wrist is the key to electrodiagnostics. Bilateral cases in cyclists does not require wrist imaging.
1
Introduction
Ulnar neuropathy at the wrist (UNW) is rare and cases occurring in patients who practice sport are exceptional . UNW may impair the whole nerve (sensory and motor fibres) or only the ulnar deep motor branch (UDMB) and may have progressive or acute onset. Clinically, differential diagnosis is always difficult with ulnar neuropathy at the elbow (UNE), which is more frequent; C 8 T 1 root disease, which is usually more painful; and lower plexus lesion, which is infrequent. In some cases, anterior horn disease has been suggested . Electrodiagnostics (EDX) of an UNW is easy when sensory and motor ulnar conductions at the wrist are impaired but can be difficult when only the UDMB is impaired and very difficult when the UDMB is partially impaired. Improving the UNW diagnosis requires systematic study of the ulnar motor conduction to the first dorsal interosseous (FDI) across the wrist to search for conduction block (CB) . The frequency of papers focused on sport-related UNW compared to those focused on “entrapment neuropathies” ( n = 18,818) found by a MEDLINE search, varies from 0.11% to 0.18% according with the terms used [“ulnar neuropathy wrist sport” ( n = 21) or “ulnar nerve wrist sport” ( n = 34)].
We reviewed our 60 cases of UNW diagnosed from 1997 to 2011 and describe 8 sport-related cases and compare these to non-sport-related cases.
1.1
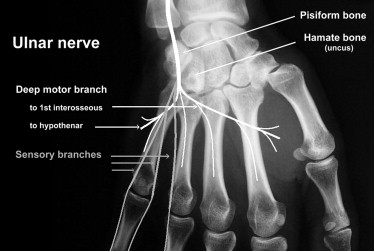
Anatomy of the ulnar nerve course at the wrist and classification of types of UNW
In 1969, Shea and McClain were the first to identify 3 different types of ulnar nerve lesion at the wrist, which were confirmed and detailed by Gross and Gelberman, in 1985 ( Fig. 1 ). Also in 1985, Wu et al. identified 5 different types of UNW: type 1 is a motor and sensory neuropathy related to a lesion located just outside of or within the proximal end of Guyon’s tunnel. Type 2 is a pure sensory neuropathy that involves the superficial branch at the wrist but distal to the branch to the palmaris brevis muscle. Types 3, 4 and 5 are pure motor neuropathies that involve the UMDB. In type 3, the lesion is located just distal to the superficial branch but proximal to the branch to the hypothenars. In type 4, the lesion is located distal to the branch to the hypothenars, and in type 5, the lesion is located just proximal to the branches to the FDI and adductor pollicis muscles. In the present study, we used the Wu et al. classification ( Table 1 ).
2
Patients and methods
2.1
Patients
Between January 1997 and July 2011, we prospectively recorded clinical and EDX data for 60 cases with a main diagnosis of UNW. Clinical examination and EDX tests were performed by the same investigator. All subjects gave their informed consent to the use of their EDX data for this study. The study was approved by the local committee on research ethics.
The diagnosis of UNW was based on clinical and EDX criteria. Clinical manifestations varied from mild to severe, intrinsic hand-muscle weakness (sparing the abductor pollicis brevis [APB]) and paresthesiae or hypoesthesia involving 1.5 ulnar digits (sparing the dorsum and palmar aspect of the hand). EDX criteria for UNE and UNW were detailed in 2 recent papers . No patient had signs or symptoms of generalized axonal or demyelinating polyneuropathy.
2.2
Methods
2.2.1
Clinical data
For each case, data were available on sex, age, body mass index, lesion side, presence of paresthesia of digits 4 and 5, weakness, and wasting of the FDI and hypothenar muscles.
2.2.2
EDX data
Each patient underwent complete EDX of both upper limbs according to a previously detailed protocol . Tests included needle examination of the impaired upper limb muscles, as well as bilateral motor and sensory conduction studies of median and ulnar nerves. Skin temperature was measured and hands were warmed before testing if < 32° C.
2.2.2.1
Ulnar nerve conduction study and criteria for abnormality
The motor conduction tested distal motor latency (DML) to both the adductor digiti minimi (ADM) and FDI. ADM recording was used to study motor conduction velocity (MCV) in the forearm, across the elbow, and in the arm. FDI recording was used to study conduction across the wrist. Recordings were performed with a pair of disposable surface electrodes. The main aim of the across the wrist conduction study was to demonstrate one motor CB, which necessitates stimulating the UDMB distal to Guyon’s tunnel.
The orthodromic sensory conduction velocity (OSCV) was studied from digit 5 to above the wrist.
The needle examination of the ADM, FDI, APB, triceps and sometimes flexor and extensor carpi ulnaris muscles of the impaired upper limb were performed in each case.
2.2.2.2
Abnormality criteria for UNW diagnosis
EDX criteria for UNW were:
- •
DML to the ADM > 3.1 ms and/or FDI > 3.4 ms;
- •
CB across the wrist (≥ 50% decrease in CMAP, without temporal dispersion);
- •
OSCV < 47 m/s and 10 m/s less than on the healthy side;
- •
absence of criteria for ulnar nerve at the elbow .
UNW diagnosis required a combination of at least one of the first 3 criteria and the 4th criterion. Non-specific findings were considered low CMAP amplitude for both the ADM and FDI (< 6.1 and 6.2 mV, respectively, or a 50% decrease as compared with the healthy side), a low sensory nerve action potential (SNAP) amplitude (< 7 μV and/or 55% decrease as compared with the healthy side), and abnormal needle examination results in one or more ulnar hand intrinsic muscles.
2.2.2.3
Median nerve conduction study
The median nerve conduction study involved DML to the APB, motor conduction velocity in the forearm, and OSCV from digit 3 to the wrist. A median nerve lesion at the wrist was diagnosed with > 3.9 ms DML to the APB and/or OSCV < 47 m/s and 10 m/s less than that for the healthy side. If results for the 2 previous tests were normal, the difference in median-to-ulnar latency of digit 4 and/or the simplified inching test were studied .
2.3
Statistical analysis
We compared data for 8 sport-related cases and 45 non-sport-related cases. Categorical data are reported as number and/or percentage and were compared by Fisher exact test. Continuous variables are reported as mean ± SD and were compared by Wilcoxon Mann–Whitney test. For all statistical analyses, a P value less than 0.05 was considered statistically significant. All statistical analyses involved the use of R release 2.2.1 statistical software package.
2
Patients and methods
2.1
Patients
Between January 1997 and July 2011, we prospectively recorded clinical and EDX data for 60 cases with a main diagnosis of UNW. Clinical examination and EDX tests were performed by the same investigator. All subjects gave their informed consent to the use of their EDX data for this study. The study was approved by the local committee on research ethics.
The diagnosis of UNW was based on clinical and EDX criteria. Clinical manifestations varied from mild to severe, intrinsic hand-muscle weakness (sparing the abductor pollicis brevis [APB]) and paresthesiae or hypoesthesia involving 1.5 ulnar digits (sparing the dorsum and palmar aspect of the hand). EDX criteria for UNE and UNW were detailed in 2 recent papers . No patient had signs or symptoms of generalized axonal or demyelinating polyneuropathy.
2.2
Methods
2.2.1
Clinical data
For each case, data were available on sex, age, body mass index, lesion side, presence of paresthesia of digits 4 and 5, weakness, and wasting of the FDI and hypothenar muscles.
2.2.2
EDX data
Each patient underwent complete EDX of both upper limbs according to a previously detailed protocol . Tests included needle examination of the impaired upper limb muscles, as well as bilateral motor and sensory conduction studies of median and ulnar nerves. Skin temperature was measured and hands were warmed before testing if < 32° C.
2.2.2.1
Ulnar nerve conduction study and criteria for abnormality
The motor conduction tested distal motor latency (DML) to both the adductor digiti minimi (ADM) and FDI. ADM recording was used to study motor conduction velocity (MCV) in the forearm, across the elbow, and in the arm. FDI recording was used to study conduction across the wrist. Recordings were performed with a pair of disposable surface electrodes. The main aim of the across the wrist conduction study was to demonstrate one motor CB, which necessitates stimulating the UDMB distal to Guyon’s tunnel.
The orthodromic sensory conduction velocity (OSCV) was studied from digit 5 to above the wrist.
The needle examination of the ADM, FDI, APB, triceps and sometimes flexor and extensor carpi ulnaris muscles of the impaired upper limb were performed in each case.
2.2.2.2
Abnormality criteria for UNW diagnosis
EDX criteria for UNW were:
- •
DML to the ADM > 3.1 ms and/or FDI > 3.4 ms;
- •
CB across the wrist (≥ 50% decrease in CMAP, without temporal dispersion);
- •
OSCV < 47 m/s and 10 m/s less than on the healthy side;
- •
absence of criteria for ulnar nerve at the elbow .
UNW diagnosis required a combination of at least one of the first 3 criteria and the 4th criterion. Non-specific findings were considered low CMAP amplitude for both the ADM and FDI (< 6.1 and 6.2 mV, respectively, or a 50% decrease as compared with the healthy side), a low sensory nerve action potential (SNAP) amplitude (< 7 μV and/or 55% decrease as compared with the healthy side), and abnormal needle examination results in one or more ulnar hand intrinsic muscles.
2.2.2.3
Median nerve conduction study
The median nerve conduction study involved DML to the APB, motor conduction velocity in the forearm, and OSCV from digit 3 to the wrist. A median nerve lesion at the wrist was diagnosed with > 3.9 ms DML to the APB and/or OSCV < 47 m/s and 10 m/s less than that for the healthy side. If results for the 2 previous tests were normal, the difference in median-to-ulnar latency of digit 4 and/or the simplified inching test were studied .
2.3
Statistical analysis
We compared data for 8 sport-related cases and 45 non-sport-related cases. Categorical data are reported as number and/or percentage and were compared by Fisher exact test. Continuous variables are reported as mean ± SD and were compared by Wilcoxon Mann–Whitney test. For all statistical analyses, a P value less than 0.05 was considered statistically significant. All statistical analyses involved the use of R release 2.2.1 statistical software package.
3
Results
Sixty cases of UNW were diagnosed over the 14 years of this study. Seven cases that occurred after ulnar nerve division at the wrist were excluded. Thus, 53 cases were selected for this study. A total of 9 of the 60 UNW cases diagnosed over the 14 years occurred in patients having a leisure practice of sport. In one 47-year-old woman, who regularly played golf, the imaging of the wrist revealed a ganglion cyst that was successfully treated with a corticosteroid injection . Thus, only 8 cases ( Tables 2A and 2B ) were exclusively related to sport and the 45 other cases were non-sport-related.
| Patient no./side | Sex | Age | Delay | CTS EDX | CTS clinic | Motor weak | FDI wast | Parest 4–5 | Sport | Outcome | Treatment | Delay |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 R | M | 43 | 1 | 1 | 1 | 1 | 0 | 0 | Fishing | Cured | Rest | 3 |
| 2 R | F | 50 | 3 | 0 | 0 | 1 | 0 | 0 | Cycling | Cured | Rest | 2 |
| 2 L | F | 50 | 3 | 0 | 0 | 1 | 0 | 0 | Cycling | Cured | Rest | 2 |
| 3 R | M | 37 | 0.2 | 0 | 0 | 1 | 0 | 0 | Kayak | Cured | Rest | 2 |
| 4 R | M | 39 | 1 | 0 | 0 | 1 | 0.5 | 0 | Kayak | Cured | Rest | 5 |
| 5 L | M | 46 | 0.2 | 0 | 0 | 1 | 1 | 0 a | Cycling | Cured | Rest | 2 |
| 6 R | M | 34 | 2 | 1 | 0 | 1 | 1 | 0 a | Cycling | Cured | Rest | 6 |
| 6 L | M | 34 | 2 | 1 | 0 | 1 | 1 | 0 a | Cycling | Cured | Rest | 1 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






