Tumors
Ganglions
General Information
Ganglion cysts are the most common soft-tissue tumor of the hand. Ganglions are formed from modified synovial cells. The cyst is usually connected with an underlying joint or tendon sheath. A ganglion cyst usually occurs when there is a small tear in capsule allowing the synovial tissue to herniate out of its normal position.
Diagnostic Criteria
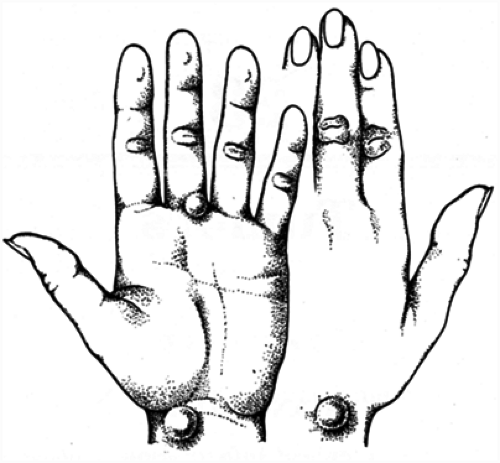
The patient presents with a soft-tissue mass. The mass may be painless or slightly painful. The mass tends to be nontender, semisoft, and will transilluminate. The mass can wax and wane as the cyst decompresses internally. The most common locations of the cyst are the dorsoradial wrist (originating from the dorsal scapholunate interosseous ligament) (Fig. 1), the volar radial wrist (originating from the volar radiocarpal joint) (Fig. 1), thumb carpometacarpal joint, or flexor carpi radialis tendon sheath), distal palm and proximal finger (a retinacular cyst originating from the tendon sheath between the A1 and A2 pulley) (Fig. 1), and dorsal distal finger (a mucous cyst originating from an arthritic distal interphalangeal joint) (Fig. 2).
Dorsal wrist ganglion cysts should be differentiated from dorsal extensor tenosynovitis and a dorsal carpometacarpal boss. Volar radial ganglion cysts should be differentiated from a radial artery aneurysm or traumatic pseudoaneurysm. An Allen’s test to determine the patency of the ulnar artery should be performed prior to surgical excision. Retinacular cysts are small pea-sized masses that should be differentiated from a giant cell tumor, lipoma, or nerve tumor (e.g., neurilemmoma).
Treatment
Treatment options include observation, splinting, aspiration with or without steroid injection, or excision of the cyst. Aspiration of the cyst, with an 18-gauge
needle, may be indicated if the cyst is large or enlarging. Care should be taken in aspirating volar ganglion cysts owing to the presence of adjacent neurovascular structures. Injection of steroids and lidocaine may reduce the mass and symptoms for a varying amount of time. Recurrence following aspiration of the cyst is high (50% or more).
needle, may be indicated if the cyst is large or enlarging. Care should be taken in aspirating volar ganglion cysts owing to the presence of adjacent neurovascular structures. Injection of steroids and lidocaine may reduce the mass and symptoms for a varying amount of time. Recurrence following aspiration of the cyst is high (50% or more).
Definitive treatment includes removal of the ganglion and its origin. When excising a ganglion arising from the joint capsule or retinaculum, a small cuff of joint capsule or tendon sheath is also excised and left open. Excision of a mucous cyst from the distal interphalangeal joint also requires debridement of underlying joint osteophytes.
Operative excision of a cyst is associated with a significantly lower recurrence rate than aspiration and also allows for an accurate diagnosis.
Giant Cell Tumors of Tendon Sheath
General Information
Giant cell tumor (GCT) of tendon sheath is a benign soft-tissue tumor that is the second most common tumor of the hand. It has also been referred to as localized nodular synovitis, fibrous xanthoma, and pigmented villonodular tenosynovitis.
Diagnostic Criteria
The tumor is usually a slow growing, firm, nontender, and nodular mass. The tumor tends to occur along the volar aspect of the hand and fingers, although it can involve the dorsal aspect. It has a propensity for the radial three digits and the distal interphalangeal region. It may produce a sensory deficit secondary to digital nerve compression. In contrast to ganglions, the mass does not transilluminate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree