Trochanteric Entry Nailing for Pediatric Femoral Shaft Fractures
J. Eric Gordon
June C. Smith
DEFINITION
Fractures of the femoral shaft are characterized by acute, nonpathologic fractures of the femur in which the primary portion of the fracture is at least 5 cm distal to the lesser trochanter and at least as far proximal to the distal femoral physis as the width of the physis.
ANATOMY
Understanding of the bony and vascular anatomy of the proximal femur is essential to the successful insertion of lateral trochanteric entry nails.
The proximal femur originates from a single proximal femoral epiphysis that develops two separate ossification centers that lead to the femoral head and greater trochanter.
Although the bony portion of the epiphysis is separate at age 8 years, a remnant of the proximal femoral epiphysis lies along the lateral aspect of the femoral neck allowing the femoral neck to increase in diameter (FIG 1).15
After age 8 years, injury to the lateral aspect of the greater trochanteric physis has no effect on the ultimate shape of the femoral neck.3 Injury to the medial aspect of this physis can lead to proximal femoral valgus and femoral neck narrowing (FIG 2A).
The medial femoral circumflex artery originates from the profunda femoris artery and courses medially to the femoral neck, passing adjacent to the piriformis fossa and forming the extracapsular arterial ring which lies at the base of the femoral neck, then anastomosing with branches of the lateral femoral circumflex artery.12, 16
Branches of the extracapsular ring give off the ascending cervical branches, which lie along the lateral femoral neck and enter the posterolateral epiphysis of the femoral head (see FIG 1).
Injury to the medial circumflex artery or the external ring can produce avascular necrosis (AVN) of the femoral head (FIG 2B).
PATHOGENESIS
Fracture of the femoral shaft can result from a direct blow, which can produce a transverse or oblique fracture with or without comminution.
Fracture of the femoral shaft can also result from rotational stresses or a twisting injury, often seen during sports injuries, leading to a spiral-type fracture.
NATURAL HISTORY
Muscle forces following fracture of the femoral shaft produce flexion and external rotation of the proximal fragment.
Muscle forces on the distal fragment produce shortening of the fracture with varus alignment.
These muscle forces produce shortening, procurvatum, varus, and an internal rotation deformity in the untreated fracture.
PATIENT HISTORY AND PHYSICAL FINDINGS
Fractures of the femoral shaft in adolescents can be produced by either sporting activities or more commonly high-energy trauma.
Examination usually reveals tenderness at the midthigh area with swelling present. The limb may have obvious deformity and shortening and may show ecchymosis or open wounds in the case of an open fracture.
A careful neurovascular examination should also be performed—palpating distal pulses and evaluating both motor and sensory neurologic function.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Good-quality anteroposterior and lateral radiographs of the femur should be obtained that allow visualization of the entire femur including the hip and knee.
If any question of a potential femoral neck fracture arises, anteroposterior and lateral views of the hip should be performed.
Patients with femoral shaft fractures secondary to high-energy trauma should have a separate anteroposterior radiograph of the pelvis to rule out concomitant injury.
DIFFERENTIAL DIAGNOSIS
Pathologic femoral shaft fracture due to benign or malignant tumor
NONOPERATIVE MANAGEMENT
Nonoperative management of older children with femur fractures consists of skeletal traction for 2 to 3 weeks followed by application of either a spica cast or a cast brace for an additional 6 to 8 weeks.
Nonoperative management of adolescents with femur fractures historically has consisted of skeletal traction for 3 to 4 weeks followed by application of a spica cast or cast brace for an additional 8 to 12 weeks.
SURGICAL MANAGEMENT
Children younger than the age of 12 years and up to 50 kg with femoral shaft fractures can be surgically treated by flexible intramedullary nailing.2
Children older than the age of 8 years can be treated by lateral trochanteric nailing using either reamed or unreamed rigid nails.5, 6
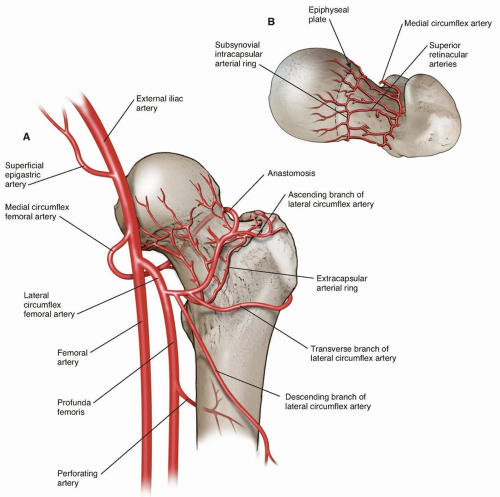
FIG 1 • A. Anteroposterior view of the bony and vascular anatomy of the proximal femur. B. Superoinferior view of the bony and vascular anatomy of the proximal femur.
Lateral trochanteric nails are particularly indicated in children 12 years of age or older or who weigh 50 kg or more up to skeletal maturity.7, 8
Lateral trochanteric nailing is also indicated in children age 8 years or older who have length-unstable fractures.
Preoperative Planning
Measurement of the femur from the greater trochanter to the distal femoral physis as well as measurement of the diameter of the medullary canal of the femur at the isthmus should be performed preoperatively in order to ensure that appropriately sized implants are available.
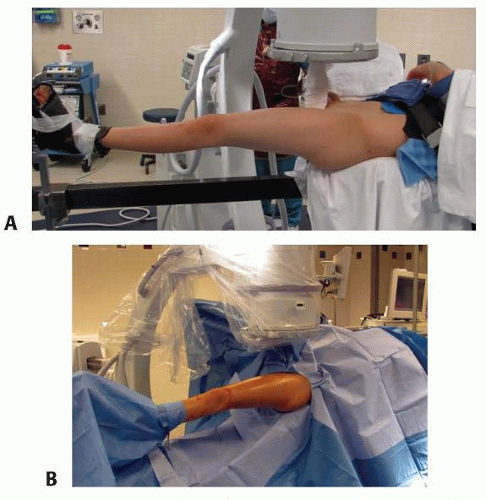
Positioning and Prepping
The patient is positioned supine on a fracture table.
The contralateral limb is flexed and abducted away from the injured limb.
The ipsilateral upper extremity should be positioned across the chest and padded and secured.
The perineal post should be padded well.
Traction is applied through a well-padded boot placed on the injured limb.
Prior to draping, the image intensifier should be used to ensure that the hip and entire femur can be visualized and that adequate traction has been applied through the boot to bring the fracture out to length (FIG 3A).
The patient’s skin should be prepared from above the hip at least 10 cm proximal to the tip of the greater trochanter to the midtibia circumferentially.
Sterile split sheets should be used to drape the patient allowing access to the femur in order to reduce the fracture via manual manipulation or open reduction if necessary.
The image intensifier should be draped sterilely as well (FIG 3B).
Approach
The preferred approach is percutaneously to the lateral aspect of the greater trochanter.
Insertion of the nail can also be performed through a lateral open approach.
TECHNIQUES
▪ Guide Pin Placement
The image intensifier should be used to visualize the hip. Because the proximal fragment usually externally rotates, the image intensifier may need to be arced past perpendicular (overrotated) to obtain a good anteroposterior image of the proximal femur (TECH FIG 1A,B).
The guide pin should be placed on the skin proximal to the greater trochanter and the image intensifier used to align the pin
so that the entry point allows placement onto the midportion of the lateral aspect of the greater trochanter and allows the pin to be driven in an angle that allows the trajectory of the pin to impact the medial cortex 1 to 2 cm distal to the lower edge of the lesser trochanter (TECH FIG 1C,D).
The pin is then pushed down onto the greater trochanter and aligned (TECH FIG 1E).
After the pin is driven into the proximal femur (TECH FIG 1F), a lateral image is obtained by arcing the image intensifier back to obtain an image perpendicular to the anteroposterior image (TECH FIG 1G,H).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree