Trigger Finger
Christina F. Endress
Jonas L. Matzon
David R. Steinberg
CLINICAL PRESENTATION
Trigger finger, or stenosing flexor tenosynovitis, is a very common problem seen by primary care physicians, orthopaedic surgeons, and hand surgeons. Patients typically present with an inability to smoothly extend or flex the digit. A tender nodule, located on the palmar surface at the level of metacarpal head, may also be present. Complaints can be vague, consisting of aching in the palm and morning stiffness of one or more digits. Initially, patients may complain of mild clicking with minimal pain. Hand dominance and occupation are not related to triggering digits.
As the flexor tenosynovitis becomes more severe, patients have increased pain over the nodule and increased triggering that occurs during flexion or prevents full extension of the finger. Patients will then start complaining that the finger “locks” or “gets stuck” as the disease progresses. Patients may become reluctant to make a full fist. Although the pathology is at the level of the metacarpal joint, patients frequently perceive the triggering as occurring at the proximal interphalangeal (PIP) joint. Early in the disease process, symptoms may improve as the day progresses, but this improvement stops when the tenosynovitis becomes more severe and locking occurs.
Stenosing flexor tenosynovitis results from localized tenosynovitis and thickening of the synovial sheath over the superficial and deep flexor tendons adjacent to the A1 pulley at the metacarpal head. This causes hypertrophy of the A1 pulley and intratendinous swelling, which leads to a discrepancy between the tendon and the tendon sheath. The two types of stenosing tenosynovitis are nodular, with thickening of the tendon on the distal edge of the A1 pulley, and diffuse, with thickening of the entire flexor tenosynovium (more commonly seen in rheumatoid arthritis). Stenosing tenosynovitis can affect any digit but most commonly affects the ring finger, thumb, and long finger.1 It is more common in women by a 4:1 ratio and occurs most often in people 40 years and older. It can also be seen in young children, presenting sometime between infancy and 3 or 4 years of age. Secondary stenosing tenosynovitis is associated with medical conditions such as diabetes mellitus, hypothyroidism, gout, renal disease, and rheumatoid arthritis. Patients who develop trigger digits are prone to developing carpal tunnel syndrome and de Quervain stenosing tenosynovitis; only occasionally do two or all three of these conditions present concurrently.
CLINICAL POINTS
The inability to smoothly extend or flex the finger is common.
Pathology is at the level of the metacarpal joint.
Condition is most common in people >40 years of age.
PHYSICAL FINDINGS
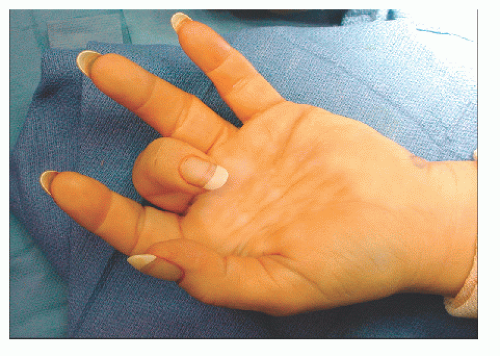
The diagnosis of trigger finger is usually suspected from the clinical presentation and can easily be confirmed on physical examination in the office. Patients usually have a nodule over the metacarpal head, at the level of the A1 pulley that moves with the flexor tendons and can be readily palpated. In patients with more severe tenosynovitis, the examiner can feel the digit “trigger” as it is flexed and extended. Some patients will present with the digit locked in flexion and may require manipulation to restore full extension. The patient is often able to voluntarily make the digit trigger or lock in the office. The examiner should evaluate both hands for flexor tendon nodules, as trigger digits may be present bilaterally.
Based on the physical exam, trigger fingers can be classified based on severity. Grade 0 is mild crepitus in a nontriggering finger. Grade 1 is uneven movement of the digit. Grade 2 is clicking without locking. Grade 3 is locking of the digit that is either actively or passively correctable. Grade 4 is a locked digit.2
STUDIES (LABS, X-RAYS)
Laboratory and radiographic studies are generally not helpful in the diagnosis of trigger finger. Plain x-rays should be obtained when there is a history of trauma, acute or remote, or for trigger thumbs, in which there is a higher association with degenerative changes.3
Impingement of the collateral ligaments on a prominent metacarpal head condyle (locked metacarpophalangeal [MCP] joint)
Dupuytren disease
Infection
Dislocation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree