Trigeminal Pain and Sensitization: Proposal of a New Stochastic Model
Peter Svensson
Abhishek Kumar
In this chapter, we will discuss the complex relationship between cervical pain related to whiplash trauma and pain in the trigeminal (V) region. We will specifically focus on the painful temporomandibular disorders (TMD) and start with a brief review of the clinical observations of overlaps between TMD pain and cervical pain. Then we summarize what is known about V sensitization and discuss possible mechanisms that may account for such overlaps in symptom presentation. In the last part, we will report on purported risk factors for TMD pain and finally propose a new stochastic model to account for complex interactions between cervical pain and V pain and sensitization.
A typical presentation of pain patterns in a patient with V pain and cervical pain and a history of a whiplash trauma 3 years previously is shown in Fig. 5-1. The patient experiences an almost constant and daily pain both in the jaws and in the neck that is exacerbated by physical function such as chewing and turning the head. The pain is also
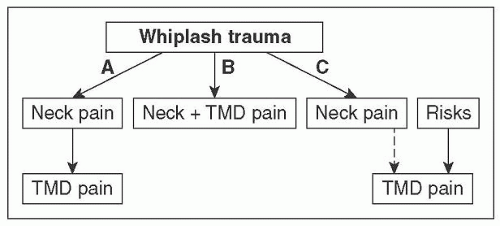
reported to influence quality of life, mood, and social relationships. When seen in the dental clinic years after a whiplash trauma, most patients will report that they think there was a tight relationship between the V pain and the cervical pain in terms of debut, development, and impact on function. Theoretically, there may be different options for a relationship (Fig. 5-2). In the attempt to dissect such difficult relationships, it may first be necessary to better define what is meant by V pain. In this chapter, we will focus primarily on the painful TMDs. The clinical classification of TMDs started with a landmark paper by
Dworkin and LeResche [7], who proposed a dual axes system with axis I being the physical presentation of the problem and axis II the psychosocial and distress part of the problem for the patient. Axis I was subdivided into (1) myofascial pain, (2) disk derangements in the temporomandibular joint (TMJ), and (3) pain in the TMJ and degenerative changes in the TMJ. It should be noted that not all TMDs per definition are painful (e.g., a clicking TMJ). The Research Diagnostic Criteria for TMD (RDC/TMD) has now been updated to the Diagnostic Criteria for TMD (DC/TMD), maintaining the dual axes approach but with validated and operationalized criteria for most of the painful TMDs [26]. A new entity termed Headache attributed to TMD has been added and serves as a link to the headache classification, that is, ICHD-3. In short, the DC/TMD allows an accurate and reproducible clinical phenotyping of the patients with V musculoskeletal pain.
reported to influence quality of life, mood, and social relationships. When seen in the dental clinic years after a whiplash trauma, most patients will report that they think there was a tight relationship between the V pain and the cervical pain in terms of debut, development, and impact on function. Theoretically, there may be different options for a relationship (Fig. 5-2). In the attempt to dissect such difficult relationships, it may first be necessary to better define what is meant by V pain. In this chapter, we will focus primarily on the painful TMDs. The clinical classification of TMDs started with a landmark paper by
Dworkin and LeResche [7], who proposed a dual axes system with axis I being the physical presentation of the problem and axis II the psychosocial and distress part of the problem for the patient. Axis I was subdivided into (1) myofascial pain, (2) disk derangements in the temporomandibular joint (TMJ), and (3) pain in the TMJ and degenerative changes in the TMJ. It should be noted that not all TMDs per definition are painful (e.g., a clicking TMJ). The Research Diagnostic Criteria for TMD (RDC/TMD) has now been updated to the Diagnostic Criteria for TMD (DC/TMD), maintaining the dual axes approach but with validated and operationalized criteria for most of the painful TMDs [26]. A new entity termed Headache attributed to TMD has been added and serves as a link to the headache classification, that is, ICHD-3. In short, the DC/TMD allows an accurate and reproducible clinical phenotyping of the patients with V musculoskeletal pain.
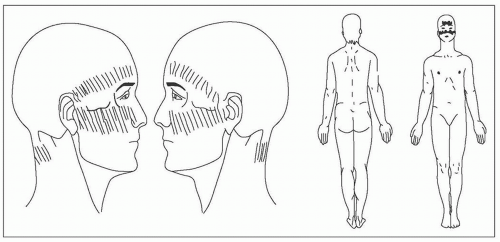 FIGURE 5-1 Illustration of pain drawings from a 39-year-old woman who had experienced a whiplash injury 3 years previously. Currently, she reports pain in the neck region as well as in the jaws. |
Systematic reviews of the clinical overlaps between TMD pain and cervical pain related to a whiplash trauma demonstrate that a median of 35% of a TMD population will report a previous whiplash trauma that seems higher than the 2-13% in non-TMD control groups [11]. Furthermore, TMD patients with a history of whiplash trauma report more severe TMD symptoms such as difficulties in jaw opening, more intense TMD pain, and more headache and stress [11]. Thus, conclusions from such systematic reviews strongly support the notion that cervical pain and TMD pain are linked together and that the whiplash injury may be a significant risk factor, not only for the cervical pain, but also for the subsequent development of TMD pain. However, few prospective studies have been performed, and without valid information on the temporal relationship, it may be difficult or at least premature to draw very strong conclusions. One prospective study in a relatively small sample demonstrated that the incidence of TMD pain following a whiplash injury was no different from the incidence of TMD pain following an ankle distortion [15]. This is one of the few exceptions that used an active control group (ankle distortion) instead of a nonpainful control group, and the results from this particular study seem to suggest that whiplash injury is only a relatively minor risk factor for subsequent development of TMD pain. Obviously, this result needs to be reproduced in larger sample sizes. In the following paragraph, we will briefly review what is known about the basic mechanisms of TMD pain and sensitization.
Pioneers in the field of basic orofacial pain research have over the last forty years carefully and systematically examined the V nociceptive system and characterized the peripheral nocieptors, afferent fiber properties, V brainstem sensory nuclei, thalamic nuclei, and cortical networks [25, 27, 30, 33]. Key elements in much of this research are the convincing demonstration of the vulnerability of the V nociceptive system and the inherent property of neuroplasticity leading to peripheral sensitization and central sensitization and therefore changing the entire gain in the nociceptive system [4, 14, 34]. Moreover, pain modulatory systems—both inhibitory and facilitatory—have been shown to have a profound impact on the responsiveness of nociceptive cells and nocifensive behaviors in animals [22, 24] and humans [2, 35]. Recent research efforts have also emphasized the interplay between the V nociceptive system and glial cells [3] as well as the immune system [20]. In fact, there are strong indications of interactions between the nociceptive system and several other biological systems including, for example, motor function [10, 13], autonomic function [6], sleep [17], emotions [32], and cognitive function.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree