Abstract
Introduction and methods
We carried out a systematic review of the literature on treatment of genu recurvatum in hemiparetic adult patients by searching the PubMed, Pedro, Trip Database and Science Direct databases. The following keywords were used: (recurvatum or hyperextension or knee) and (hemiplegia or hemiparesis).
Results
Nine articles met our selection criteria. Four assessed retraining methods (functional electric stimulation or electrogoniometric feedback), two assessed orthopaedic or neurosurgical treatments and three articles focused on orthoses.
Discussion and conclusion
Even though all the various treatments produced encouraging results, most of the reviewed studies presented methodological limitations. Moreover, none of the selected articles suggested a treatment strategy which takes account of the various aetiologies in genu recurvatum. On the basis of some of the reviewed articles and our own clinical experience, we propose an aetiology-specific treatment strategy for genu recurvatum patients. In a broad patient population, this categorization could form the basis for testing the specificity of each treatment method as a function of the cause of genu recurvatum. This approach could help confirm the clinical indications and identify the most appropriate treatment for each patient.
Résumé
Introduction et méthode
Nous avons réalisé une revue systématique de la littérature concernant le traitement du recurvatum de genou chez le patient adulte hémiparétique en parcourant les bases de données PubMed, Pedro, Trip Database et Science Direct, et en utilisant les mots-clés suivants : recurvatum and hemiplegia/-paresis , hyperextension and hemiplegia/-paresis , knee and hemiplegia/-paresis .
Résultats
Neuf articles ont été retenus sur base de nos critères d’inclusion. Quatre d’entre eux évaluent des méthodes de rééducation, soit par stimulation électrique fonctionnelle, soit par feedback électrogoniométrique. Deux autres articles étudient des traitements chirurgicaux, soit orthopédique, soit neurochirurgical. Les trois articles restants sont dédiés à l’appareillage.
Discussion et conclusion
Les effets des différents traitements évalués semblent encourageants, même s’il existe certaines limites méthodologiques pour la plupart des études. Malheureusement, aucun des articles cités ne propose de prise en charge stratégique tenant compte de l’origine du recurvatum de genou. Sur base de certains de ces articles et de constatations cliniques, nous proposons une stratégie de prise en charge en fonction des différentes étiologies possibles du recurvatum. Cette catégorisation pourrait servir de base pour tester sur de larges échantillons de patients la spécificité des techniques utilisées en fonction de l’origine du recurvatum. Cela permettrait de confirmer les indications cliniques proposées et de cibler les interventions les plus efficaces pour chaque patient.
1
English version
1.1
Introduction
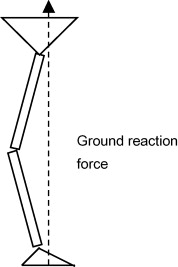
Genu recurvatum affects between 40 and 68% of hemiparetic stroke patients . From a biomechanical point of view, genu recurvatum occurs during the stance phase. It is characterized by a ground reaction force vector that passes well in front of the knee ( Fig. 1 ). In patients with quadriceps weakness, this phenomenon generates a knee extensor moment which avoids collapse during the stance phase. In other cases, the presence of spastic or retracted muscles (the ankle plantar flexors or the quadriceps, for example) causes knee hyperextension . In clinical practice, gait retraining in genu recurvatum is relatively complex because of (i) the wide variety of possible (and often interlinked) aetiologies and (ii) variability in the expression of the patient’s pyramidal syndrome . Furthermore, genu recurvatum is often associated with other kinematic gait anomalies, such as equinus foot or stiff knee. The various causes of genu recurvatum are as follows:
- •
weakness of the knee extensors. In biomechanical terms, the patient keeps the knee in hyperextension so as to keep the ground reaction force in front of the knee, which prevents the latter from collapsing. This compensatory mechanism is also used by patients suffering from peripheral paralysis of the quadriceps (due to neuropathy in the legs or the sequelae of poliomyelitis, etc.);
- •
spasticity of the knee extensors (the vastus muscles). Usually, at the start of the stance phase, one observes discrete knee flexion in an eccentric movement, which helps dampen the impact of foot-ground contact. In the event of knee extensor spasticity during the stance phase, this normal knee flexion turns into abnormal extension;
- •
weakness of the buttock muscles leads to forward pelvic tilt and lumbar hyperlordosis, excessive hip flexion and compensatory knee hyperextension. This is a classic gait pattern in L5 spine-injured patients;
- •
weakness of the knee flexors (the hamstring muscles). This weakness can also be iatrogenic in cases of over-extension of the hamstring muscles, as described in children with cerebral palsy . In the stance phase, contraction of the knee flexor muscles is needed to control knee flexion – especially if the extensors are spastic. Conversely, spasticity of the knee flexors will generate excessive, permanent knee flexion;
- •
limited dorsal ankle flexion, as a result of spasticity and/or retraction of the muscles in the posterior compartment of the leg. In this case, the knee is positioned in hyperextension due to the patient’s inability to move the tibia forward during the stance phase, as a result of ankle stiffness. If the patient wishes to avoid genu recurvatum (and as long as the knee flexors are sufficiently strong), he/she will have to adopt an equinus gait pattern;
- •
avoidance of painful pressure on the ball of the foot. As in the case of spasticity or retraction of the muscles in the posterior compartment of the leg, advancement of the tibia is restricted and generates hyperextension;
- •
proprioceptive disorders. As with weakness of the knee extensors, hyperextension enables safe step-to-step transition, without the risk of poor knee control and subsequent collapse.
It is also common to see several aetiologies in the same patient, such as (i) a combination of ankle plantar flexor spasticity and quadriceps weakness or (ii) spasticity of the quadriceps associated with a proprioceptive disorder and retraction of the ankle plantar flexors. Accurate determination of the main cause(s) of recurvatum is an essential step in adjusting the retraining programme and identifying appropriate treatments for the spasticity and/or retraction.
The goal of the present study was to perform a systematic review of the literature on the treatment of genu recurvatum in the hemiparetic adult patient, in order to (i) determine whether there is an appropriate treatment for each possible aetiology and (ii) generate concrete proposals for patient management.
1.2
Method
We performed a systematic literature review. The first two authors of the present paper independently searched the PubMed, Pedro, Trip Database and Science Direct databases by using the following keywords: (recurvatum or hyperextension or knee) and (hemiplegia or hemiparesis).
The article selection criteria were as follows:
- •
studies performed on hemiparetic adult subjects;
- •
studies describing the study population (genu recurvatum);
- •
full papers published in French or English in a peer-reviewed journal (case-reports were thus excluded).
1.3
Results
On the basis of the retrieved abstracts, we selected 49 articles. After reading the full texts, eight papers matched our selection criteria and are listed in Table 1 . Inspection of the bibliographic references in the selected articles yielded an additional paper for inclusion in the review.
| Authors | Subjects | Treatment method evaluated | Cause of the recurvatum | Variables studied | Type of study | Results |
|---|---|---|---|---|---|---|
| Stanic et al. (1978) | 15 included patients 11 performed the full programme (3–48 months after stroke) 8 of the 11 patients presented knee hyperextension in the stance phase | Retraining with multichannel functional electrical stimulation (3 times a week for 1 month, 1 month’s rest, then resume for 1 month) – stimulated muscles: ankle DF/PF, knee flex/ext, hip ext/abd | Not specified | Clinical, qualitative gait analysis | Prospective, no control group | Knee hyperextension of improved in 7 of the 8 patients, stable for 1 |
| Hogue and McCandle (1983) | 13 patients | Retraining with electrogoniometric feedback (beep from 0° extension) – gait with the device 4 × 55 feet for 10 days with a physiotherapist, then 5 days without the physiotherapist, then 5 days with the physiotherapist | Not specified | Number of beeps | Prospective, no control group | Decrease in the number of beeps |
| Basaglia et al. (1989) | 18 patients | Retraining with electrogoniometric feedback (signal at 180° to avoid hyperextension) – duration depending on the patient’s progress, stopping when there is a decrease in errors on 5 consecutive days | Not specified | Spontaneous gait speed Max gait speed Number of errors (recurvatum during the stance phase) | Prospective, no control group | Decrease in the recurvatum after 12 sessions, on average. Results maintained after 1 year |
| Morris et al. (1992) | 26 stroke patients (< 4 months) | Retraining with electro-goniometric feedback versus classical physiotherapy | Not specified | Max knee extension MAS 10 m test Gait symmetry | Prospective and randomized | Decrease in knee hyperextension Increase in MAS 10 m test: no change |
| Pinzur et al. (1986) | 54 patients with spastic equinus (equinovarus), > 1 year after stroke 3 groups: I dynamic varus (15% patients) II spastic equinovarus and knee hyperextension (70%) III knee hyperextension +++ (15%) | Orthopaedic surgery: lengthening of the Achilles tendon + lateral transfer of the TA, + lengthening of the toe flexors (group A), + for 12 patients: lengthening of the TP (group B) | Not specified | Multifactorial gait analysis (ultrasound gait monitor for measuring the duration of the stance phase/swing phase, EMG, electrogoniomete r) Need for an orthosis or not | Prospective – control group with 30 healthy subjects | Recurvatum: qualitative improvement of gait 10 patients in group II → I 1 patient in group III → II group A same as group B Decreased need for orthosis Normalization of stance phase/swing phase duration |
| Caillet et al. (1998) | 9 patients presenting spastic equinovarus foot – genu recurvatum in 6 of them | Selective tibial neurotomy (variously the nerve(s) to the soleus, gastrocnemius medialis and lateralis, TP, toe flexor/ flexor hallucis longus, brevis) | Not specified | Gait analysis (Vicon system) before and 6 months after neurotomy | Prospective – no control group | No change in stance phase/swing phase duration Correction of knee hyperextension in 5 out of 6 patients |
| Farncombe (1980) | 11 patients | Retraining with an anti-recurvatum orthosis (Swedish knee cage) for 6 months | Not specified | Clinical observation of the presence or absence of recurvatum during gait | Cohort follow-up | Independent gait with good knee control without the need for an orthosis in 9 out of 11 patients |
| Morinaka et al. (1982) | 36 patients included 25 evaluated -Brunnstrom stage 3 to 3.5 | Use of a jointed leg-foot brace with a range of knee movement from 0 to 130° | Not specified | Observation of the gait pattern Gait speed test | Prospective, control group of 15 patients wearing an ankle-foot orthosis | Better gait pattern Increase in gait speed compared with the control group |
| Morinaka et al. (1984) | 120 patients included – 82 evaluated – 3 groups: Group A: unable to walk without the leg-foot brace (53); Group B: gait improved by the leg-foot brace (29); Group C: gait reasonable with an ankle-foot orthosis (0) | Use of a jointed leg-foot brace with a range of knee movement from 10 to 130° (mean duration: 21 months). | Not specified | Follow-up of the patients, evaluation of the number of patients moving from one group to another Evaluation of the dynamic EMG with and without an orthosis for 2 patients | Cohort follow-up | Change over time for the patients: Group A → 29; Group B → 35; Group C → 18 Dynamic EMG: for 2 patients, quasi-normalization of the muscle activation times after wearing a full leg-foot brace |
Of the nine articles selected in this systematic review, four evaluated retraining methods (functional electrical stimulation or electrogoniometric feedback ), two dealt with surgical and orthopaedic treatments , and three focused on orthotic devices .
1.4
Discussion
The majority of the nine selected studies were prospective and did not include a control group. Only one prospective, randomized study was identified . On the whole, the various treatments appear to have positive outcomes, despite the presence of methodological limitations. In addition to the absence of a control group , some studies did not specify the time period between the stroke and the patient evaluation , whereas others featured a mixture of acute-phase subjects (i.e. less than six months after the stroke) and chronic-phase subjects (more than six months after the stroke) . The validity of certain evaluation methods is also questionable – mainly in the studies based primarily on observation of gait patterns . The study by Caillet et al. was the only one to include a pre- versus post-treatment instrumented gait analysis. Furthermore, five of the selected studies featured small sample sizes (< 20 patients) . Studies evaluating the effect of surgical treatments lacked standardisation. Although all 54 patients treated orthopaedically by Pinzur et al. underwent lengthening of the Achilles tendon extension and lateral transfer of the tibialis anterior muscle, 12 also underwent release of the tibialis posterior. The other 42 patients underwent lengthening of the toe flexors. In Caillet et al.’s neurosurgical study , the nine patients underwent selective tibial neurotomy; this variously included the nerves to the soleus, the gastrocnemius medialis and lateralis, the tibialis posterior and/or the toe flexors. It is noteworthy that surgical treatments were always performed distally, in order to correct spasticity-retraction of muscles in the posterior compartment of the leg. To date, proximal surgical treatment (with a view to treating spasticity of the quadriceps, for example) has not been been described in the literature. Most of the articles examining retraining methods focused on the importance of motor control and gait cycle disorders generated by abnormal muscle activation times. However, as mentioned above, the evaluation methods used by these authors (based on the mere observation of gait patterns, in the absence of objective, instrumented gait analysis) limit the conclusions that can be drawn from these works.
Lastly, none of the articles suggested a patient management strategy based on the various aetiologies possible, i.e. knee extensor weakness or spasticity, weakness of the buttock muscles, weakness or over-extension of the hamstring muscles, limited dorsal ankle flexion as a result of spasticity and/or retraction of the muscles in the posterior compartment of the leg, avoidance of painful pressure on the ball of the foot and, lastly, proprioceptive disorders . These various aetiologies (especially the first five) are frequently encountered in hemiparetic patients and can also be combined. The most typical example is a combination of knee extensor and sural triceps spasticity with hamstring weakness, which keeps the knee in hyperextension throughout the cycle gait.
The fact that the genu recurvatum patients seen in routine clinical practice often have several aetiologies may explain why the various authors cited above did not attempt to take account of this parameter in their treatment. However, systematic consideration of one or more aetiologies can help the clinician decide on the appropriate therapeutic option.
The question remains as to why genu recurvatum should indeed be treated. Firstly, the resulting gait pattern is sometimes considered to be inaesthetic by the patient. Secondly, hyperextension during the stance phase increases the latter’s duration and makes it difficult to achieve spatially and temporally symmetrical gait. Thirdly, genu recurvatum (or rather the absence of knee flexion) extends the limb and increases the external mechanical work linked to elevation of the body’s centre of mass and thus the energy cost of gait. Lastly, and probably most importantly, genu recurvatum can be painful as a result of stress to the ligaments and tendons at the back of the knee.
Once genu recurvatum had been categorized according to its aetiology, the clinician can consider various treatment options. We derived our strategy for the aetiology-based treatment of genu recurvatum from our own clinical practice and insights gained from a number of scientific publications. Evaluation of the “aetiology-treatment” pairs suggested by various authors also opens up research perspectives and provides an opportunity to better match a patient’s treatment to his/her specific condition.
In cases of knee extensor weakness , it is important for a patient to maintain recurvatum; this enables him/her to take steps safely, with a load line, which stays in front of the knee, as in femoral amputees or polio victims. A hinged leg orthosis may be useful for stopping the recurvatum from worsening but the device must be adjusted so that the patient can maintain slight recurvatum in the stance phase. If the risk of knee unlocking is high, a rigid, full leg brace that maintains the knee in extension may be useful for both correcting recurvatum and countering the risk of unlocking. However, this type of orthosis has many disadvantages: it is bulky, uncomfortable in the sitting position and may be difficult to put on by a hemiplegic patient who may often have only one fully functional arm .
In cases of knee extensor spasticity (the impact of which is often aggravated by hamstring weakness), genu recurvatum is present during both the swing phase (“stiff-knee gait”) and stance phase of gait . This gait pattern is difficult to correct. Recently, botulinum toxin injections in the quadriceps were shown to improve knee flexion in the swing phase and to reduce the energy cost of gait . However, this improvement was not clinically obvious and did not exceed 5° of knee flexion. We did not identify any literature publications dealing with the effect of treating quadriceps spasticity on genu recurvatum.
When the patient presents significant hamstring weakness and/or overextension (as has been described in children with cerebral palsy ), concentric reinforcement of the hamstring muscles and use of a ankle-foot orthosis with limited plantar flexion can help the subject to control their knee during the stance phase.
In cases of buttock muscle weakness (leading to excessive hip flexion and compensatory knee hyperextension), a combination of analytical reinforcement of the buttock muscles and functional electrical stimulation can help the patient to change his/her gait pattern. This aetiology (cited in J. Perry’s book ) is not, however, mentioned in any of the articles selected for review. Nevertheless, we note that the study by Stanic et al. on multichannel functional electrical stimulation included the hip extensors as target muscles.
When there is spasticity of the posterior leg muscles or the knee extensors, it may be useful to consider focal treatment of the spasticity (e.g. botulinum toxin injections or selective neurotomy), as suggested by Caillet et al. [4]. When the spasticity is complicated by irreducible retraction of the posterior leg muscles, two therapeutic options can be envisaged. The first consists in surgical extension of the muscle and tendon systems at the back of the leg (i.e. the Achilles tendon and the toe flexors), as proposed by Pinzur et al. . The second involves conservative treatment via the use of orthopaedic shoes, with compensation of equinus foot. When treatment of spasticity and retraction is not possible or not sufficient, an appropriate device (a hinged ankle-foot orthosis with limited plantar flexion, in this case) can help the patient to progressively adopt a different gait pattern . However, one should note that in cases of associated quadriceps weakness, an ankle-foot orthosis will prevent the ankle from positioning itself in dorsal flexion; this runs the risk of generating knee flexion on heel strike, which may well “unlock” the flexed knee and induce a fall . The effect of the Chignon ® orthosis on gait kinematics, mechanics and energetics has recently been studied in 10 hemiparetic adult patients . Only three of the subjects presented genu recurvatum, which was not significantly improved by wearing the Chignon ® orthosis. This surprising absence of improvement may be related to either suboptimal adjustment of the orthosis or the additional presence of quadriceps spasticity.
In cases of deliberate genu recurvatum in order to avoid painful pressure on the ball of the foot, treatment of the cause of the pain should be considered. In fact, the pain is often caused by a painful, spastic toe curl, which may benefit from treatment with botulinum toxin or tendon extension . There may also be overpressure pain at the heads of the metatarsals or pain related to hallux valgus. In both circumstances, use of orthopaedic insoles and/or appropriate footwear can relieve the pain. We did not find any publications that specifically discussed this latter point in the hemiparetic adult.
Lastly, in the absence of spasticity and/or weakness of the above-mentioned muscle groups, genu recurvatum can occur when major sensory disorders are present. One then considers that genu recurvatum is generated by proprioceptive disorders . This aetiology is scarcely covered in the literature: even Morris et al. [17] do not cite proprioceptive disorders as a possible cause of recurvatum, despite having studied the impact of electrogoniometric feedback therapy on knee control. If the proprioceptive impairment is minor, an ankle-foot orthosis with limited plantar flexion can help the patient to adequately position his/her knee during the swing phase. An anti-recurvatum orthosis (such as the Swedish Knee Cage) may also be of value in proprioceptive retraining . If the proprioceptive impairment is significant, the same reasoning as in cases of quadriceps weakness can be adopted and use of a full leg brace with free or locked flexion may be considered.
In practice, a combination of these different aetiologies is frequently observed and thus forms a more complex clinical picture. In such cases, a step-by-step analysis should enable the physician to progressively determine the most appropriate treatment. For example, if the patient presents spasticity of the ankle plantar flexors and/or toe flexors and/or quadriceps, the first step consists in performing selective motor nerve blocks and then botulinum toxin injections (together with an intensive physiotherapy programme and orthosis use), with a view to reprogramming the gait pattern. Depending on the results obtained once the spasticity has disappeared, the physician can think about the potential utility of surgical treatment (neurotomy or muscle lengthening procedures ).
1.5
Conclusion
The nine articles selected in this systematic review of the literature looked at the overall treatment of genu recurvatum, either via retraining methods (electrical functional stimulation and electrogoniometric feedback), orthopaedic or neurosurgical surgery or use of an orthosis. None of the selected studies specified the cause of genu recurvatum in their patients. In the Discussion section, we emphasized the value of taking the possible aetiologies (related to variable expression of the hemiparetic patient’s pyramidal syndrome) into account and thus fine-tuning the overall patient management programme. Given the prevalence of genu recurvatum in hemiparetic patients, we believe that it is important to test the suggested treatment techniques as a function of the aetiology. In concrete terms, chronic-phase patients (i.e. more than six months after the stroke) could be classified according to the likely aetiology and evaluated with an objective tool (such as instrumented gait analysis) before and after treatment. This type of clinical study would help to confirm the clinical indications suggested in this literature review and determine the most effective treatment for each patient. Likewise, protocols that evaluate the change over time in motor command following a specific physiotherapy programme should include instrumented gait analysis with dynamic electromyography, with a view to evaluating muscle activation times during the gait cycle.
2
Version française
2.1
Introduction
Le recurvatum de genou affecte 40 à 68 % des patients hémiparétiques après un accident vasculaire cérébral (AVC) . D’un point de vue biomécanique, le recurvatum de genou survient durant la phase d’appui. Il est caractérisé par un vecteur de force de réaction au sol passant nettement en avant du genou ( Fig. 1 ). En cas de faiblesse importante du muscle quadriceps, ce phénomène génère un moment extenseur de genou qui évite l’effondrement durant la phase d’appui. Dans d’autres cas, c’est la présence de muscles spastiques ou rétractés qui sera à l’origine de l’hyperextension de genou (par exemple, les fléchisseurs plantaires de cheville ou le quadriceps) . En pratique clinique, la prise en charge rééducative du recurvatum de genou est relativement complexe en raison de la diversité des étiologies possibles, souvent intriquées, liées à la variabilité d’expression du syndrome pyramidal . Par ailleurs, il est souvent associé à d’autres anomalies de la cinématique de marche telles que le pied varus équin ou le stiff knee gait . Les causes du recurvatum sont :
- •
le déficit de force des extenseurs de genou. Sur le plan biomécanique, le patient, dans ce cas de figure, maintient le genou en hyperextension pour faire passer la force de réaction au sol devant le genou, ce qui en empêche l’effondrement. Ce mécanisme de compensation est également utilisé par les patients porteurs d’une paralysie périphérique du quadriceps (neuropathie crurale, séquelle de poliomyélite…) ;
- •
la spasticité des extenseurs de genou (vastes). Normalement, on observe une discrète flexion de genou en début de phase d’appui selon un mode excentrique qui permet d’amortir les répercussions du contact du pied au sol. En cas de spasticité des extenseurs de genou s’exprimant en phase d’appui, cette flexion physiologique de genou se transforme en une extension pathologique ;
- •
la faiblesse des muscles fessiers entraîne une antéversion du bassin associée à une hyperlordose lombaire, à une flexion de hanche excessive et à une hyperextension de genou compensatrice. Il s’agit d’un pattern de marche classique chez les patients blessés médullaires de niveau L5 ;
- •
la faiblesse des muscles fléchisseurs de genou (ischiojambiers). Cette faiblesse peut également être iatrogène en cas d’allongement excessif des muscles ischiojambiers, comme décrit chez l’enfant infirme moteur cérébral (IMC) . La contraction des muscles fléchisseurs de genou est nécessaire en phase d’appui afin de contrôler la flexion du genou surtout si les extenseurs sont spastiques. À l’inverse, une spasticité des fléchisseurs de genou générera une flexion permanente excessive du genou ;
- •
la limitation de la flexion dorsale de cheville, consécutive à une spasticité et/ou à une rétraction des muscles de la loge postérieure de la jambe. Dans ce cas, le genou est positionné en hyperextension suite à l’impossibilité d’avancer le tibia durant la phase d’appui en raison de la raideur de la cheville. Si le patient souhaite éviter le recurvatum de genou, il devra marcher en équin (si toutefois la force des fléchisseurs de genou le lui permet) ;
- •
de l’évitement de l’appui sur l’avant-pied en raison de douleurs. Comme dans le cas de la présence d’une spasticité ou d’une rétraction des muscles de la loge postérieure de la jambe, l’avancée du tibia est limitée, ce qui génère l’hyperextension ;
- •
de troubles proprioceptifs. Comme dans le cadre du déficit de force des extenseurs de genou, l’hyperextension dans ce cas permet un passage du pas en sécurité, sans risque d’effondrement lié au mauvais contrôle du genou.










