Abstract
Objective
To assess the relevance of the RAPT (Risk Assessment and Prediction Tool), among a cohort of patients undergoing total hip arthroplasty (THA).
Method
Prospective study of a cohort of patients evaluated before and after THA. The difference between the postoperative orientation predicted by the RAPT and the real one is assessed. Clinical, environmental and psychosocial criteria that could significantly change the orientation are discussed.
Results
One hundred and thirty-four patients (94 women and 40 men) were included. The average age was 71.6 (±10) years. Primary hip osteoarthritis was the indication for surgery in 78% of cases. The average length of stay in the surgery ward was 10 (±3) days. It was significantly higher for patients referred to a rehabilitation ward ( P < 0.0001). Sixty-six percent of patients were referred to a rehabilitation ward and 34% returned directly home. The average length of stay in rehabilitation ward was 27 (±13) days. The validity of the RAPT as a help decision tool has been confirmed. Thus, a low RAPT score was significantly associated with more frequent referral to a rehabilitation ward, conversely, a high RAPT score is significantly related to more frequent direct return to home.
Conclusion
This study confirmed the usefulness of the RAPT to help in patient orientation decision after total hip arthroplasty. The patient preference remains the main variable for orientation after THA. By the way, the patient preference must not be integrated into the RAPT, but need to be collected and be discussed with the patient.
Résumé
Objectifs
Vérifier la pertinence du RAPT (Risk Assessment and Prediction Tool), auprès d’une cohorte de patients opérés d’une arthroplastie totale de la hanche (PTH).
Méthode
Étude prospective, d’une cohorte de patients évalués en pré- et postopératoire d’une PTH sur la différence entre l’orientation prédite par le RAPT et l’orientation réelle ainsi que les critères pouvant modifier significativement cette orientation qu’ils soient cliniques, environnementaux ou psychosociaux.
Résultats
Cent trente-quatre patients (94 femmes pour 40 hommes) ont été inclus. L’âge moyen était de 71,6 (±10) ans. Dans 78 % des cas, une coxarthrose primitive était à l’origine de l’arthroplastie. La durée moyenne de séjour en service de chirurgie était de 10,0 (±3) jours. Celle-ci était significativement plus élevée pour les patients orientés vers un établissement de rééducation ( p < 0,0001). Soixante-six pour cent des patients ont été adressés vers un établissement de rééducation et 34 % sont retournés directement à domicile. La durée de séjour moyenne en établissement de rééducation était de 27 (±13) jours. La validité du score RAPT comme outil d’aide à la décision dans l’orientation des patients a été confirmée. Ainsi, un score RAPT faible est significativement lié à une orientation plus fréquente vers un service de rééducation ; à l’inverse, un score RAPT élevé est significativement lié à un retour à domicile plus fréquent.
Conclusion
Cette étude a confirmé l’utilité du RAPT pour aider le clinicien à prévoir l’orientation des patients après arthroplastie totale de hanche. Concernant la préférence du patient, qui reste la variable prépondérante dans l’orientation après PTH, il reste légitime de ne pas l’intégrer au RAPT mais de la recueillir pour la confronter à celui-ci pour décider de l’orientation postopératoire avec le patient.
1
English version
1.1
Introduction
Often related to osteoarthritis, hip lesions trigger pain and joint limitations leading to functional impairments. When the first-line medical treatment, associating pharmacological and non-pharmacological treatments, can no longer manage the affection , total hip replacement (THR) is recommended. The frequency of this surgery is constantly increasing in industrialized countries because of the aging of the population and longer life expectancy. In the United States, the demand for primary total hip arthroplasty is estimated to grow by 174% . In France, 105,000 persons had total hip arthroplasty in 2000, which ranks it in 10th place of all surgeries for that year .
During the past 20 years, postoperative management of total hip arthroplasty has completely changed in all industrialized countries. In the light of cost-effective healthcare management, the length of stay in the surgical unit went from 3 weeks in the seventies to less than one week nowadays .
This reduction led to an increase in the number of transfers and thus a potential increase of the inpatient stays in physical medicine and rehabilitation (PM&R) centers. Furthermore, there is a strong preference to promote a return home right after surgery mainly for cost-effective reasons.
Thus, Lavernia et al. studied post-discharge costs after THR in 2003. Home-based rehabilitation had a mean cost of 2405 dollars, whereas center-based rehabilitation had a mean cost of 13,435 dollars. Brought back to the entire population of the United States, the total cost of postoperative rehabilitation after THR was estimated at 3.2 billion dollars .
An analysis of the literature regarding discharge outcomes after total hip arthroplasty, found an important clinical heterogeneity from one country to the next but also within one given country. Thus, a Canadian study reported that inpatient rehabilitation care after THR varied from 0 to 86% according to the hospital where the surgery was performed . In 2006 in France, Maravic and Landais reported a 33% hospitalization rate in PM&R centers after THR whereas this hospitalization rate increased to 46% in a study conducted on a cohort in the Provence-Alpes-Côte-d’Azur region (PACA) . However, a study showed that only 6% of British patients went to a PM&R center after THR .
In the literature, the few studies focusing on criteria related to postoperative management in rehabilitation center have a low level of scientific evidence. They unveiled that the decision to discharge patients to a rehabilitation center is based on multiple factors. The most important factors are old age, functional impairments, living alone and patient’s preference . According to these elements, it would be relevant to use tools, before surgery, to help with taking a decision on postoperative management. Finally, the reduction in the mean Length Of Stay (LOS) for short-term hospitalization stays and the actual tendency to send patients directly home post-surgery, highlight the need to determine objective evaluation criteria to better orientate patients and propose a care management strategy adapted to their preoperative and immediate postoperative needs.
An analysis of the literature found two tools to help decide on discharge outcomes. The first one, proposed by Bindelglass et al. , takes into account the patient’s age, home environment and quality of life (SF36). Its main limit lies in the absence of a prospective validation.
However, the Risk Assessment and Prediction Tool (RAPT) has been validated in a prospective manner . This tool takes into account six variables: age, gender, preoperative functional capacity with or without technical aids, social support at home, living alone as well as the patient’s preference. The total score is computed by adding the six different variables. It helps determine three subgroups of patients:
- •
a score > 9 means patients can be discharged home and do their rehabilitation as outpatients;
- •
a score < 6, means patients need to be discharged to a PM&R center;
- •
for patients with a score between 6 and 9 it is difficult to determine discharge outcomes during the preoperative period.
Once the score computed, the decision to discharge patients to a PM&R center is based on the RAPT score but also the patient’s preference. Finally, in a second prospective study the use of the tool associated with an intensive postoperative rehabilitation care allowed to change the orientation of patients, initially decided during the preoperative period . In this second study, the authors also validated the predictive value of the RAPT on a cohort of 50 patients who underwent total lower limb arthroplasty (preoperative RAPT value significantly correlated to the patients’ real discharge destination, F = 2029, P = 0.003).
The main limit of this study concerned its cohort, which included patients who had total hip or knee arthroplasty without highlighting the differences between these two subgroups.
The RAPT was validated in French according to a translation/back-translation process . It was also the theme of recent publications in cohorts of patients who had total knee replacement surgery in different health care systems and its use has been recommended in the care pathways published by the SOFMER (French Society of Physical Medicine and Rehabilitation) .
The main objective of this study was to test the validity of the RAPT tool to help decide on discharge outcomes for patients after total hip arthroplasty.
1.2
Material and method
1.2.1
Patients
All patients, over a one-year period, referred to the preoperative rehabilitation consultation before total hip arthroplasty were studied retrospectively. Patients were referred to this consultation by their surgeon after the surgical decision had been made to look at preoperative and postoperative rehabilitation measures.
Patients were seen by a multidisciplinary team, which included an occupational therapist, a social worker and a PM&R physician. During the consultation, they were handed out a preoperative physiotherapy prescription, advice on technical aids and finally were informed on the objectives of postoperative rehabilitation care. All departments of orthopedic surgery, in private or public structures, in the Clermont-Ferrand area participated in the study.
1.2.2
Collected criteria
Real destination at discharge, i.e. home or PM&R center, was collected as well as length of stays in surgery or PM&R center when appropriate.
All RAPT variables were taken into account: age, sex, preoperative walking distance, using technical aids for walking, use of community supports and patient’s expectation of postoperative discharge destination (extended rehabilitation stay in a PM&R center vs. returning directly home).
Other criteria that could influence the discharge destination of patients based on data from the literature and experts’ consensus (occupational therapist, social worker, PM&R physician) were also taken into account: type of structure where the surgery took place (private/public, hospital/clinic), length of stay (LOS) in the surgical unit and in the rehabilitation unit when adequate, comorbidities, Knee Society Classification System , functional impairments assessed by the Lequesne index , home environment (rural or urban), isolation, postoperative complications, home accessibility. Home accessibility was determined based on the opinion of experts (PM&R physicians and occupational therapists) according to three sub-items: adapted home, inside and outside accessibility. If the answer to one of these three items was negative, the home was considered not accessible.
The outside of the home was deemed not accessible if there was at least one flight of stairs to get into the home or no elevator to get to a building floor. The inside of the home was deemed not accessible if the bedroom, bathroom and kitchen were not on the same level or if there was not possibility to set up a bedroom on the same level as the kitchen and bathroom. Home adaptation concerned the bathroom and restroom with installing a non-slip shower mat, handle bar and a raised toilet seat.
1.2.3
Follow-up of patients
We used two different data collection modes. For patients discharged to a PM&R center, data were collected from the patients’ charts in the various PM&R centers where they were hospitalized. For patients who did not stay in a PM&R center, they were contacted directly by phone.
1.2.4
Ethics
In the absence of direct individual benefits and/or impact on the physical integrity of subjects, this study was not reported to the local ethics committee. Since there was no randomization and no impact on the physical or mental integrity of subjects, no signed informed consent form was required. The patient’s oral consent was collected before inclusion in the study after having been informed on the study’s objectives. This study was conducted according to good clinical practices, the declaration of Helsinki and the World Medical Association (Tokyo 2004, revised).
1.2.5
Statistical analysis
The first step of the analysis was dedicated to a description of the population. Quantitative data were expressed in mean values and standard deviations, quantitative variables were expressed in raw data and percentages.
Secondarily, an inferential analysis was conducted to determine if the variables of interest (included in the RAPT and not included in the RAPT) could influence the patients’ postoperative management. For continuous quantitative variables, we used a non-parametric Wilcoxon signed-rank test.
Using a logistic regression analysis, we determined the predictive nature of the variables included in the RAPT for discharge to a PM&R center as well as the relative weight of these variables.
Only factors with a significant P < 0.05 value in the univariate analysis were included in the logistic regression. All analyses were performed with the SAS software.
1.3
Results
1.3.1
Descriptive analysis
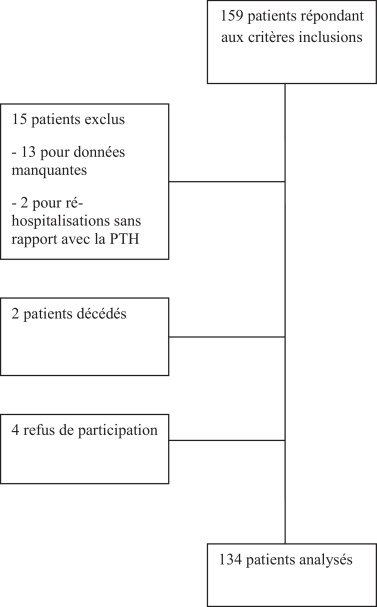
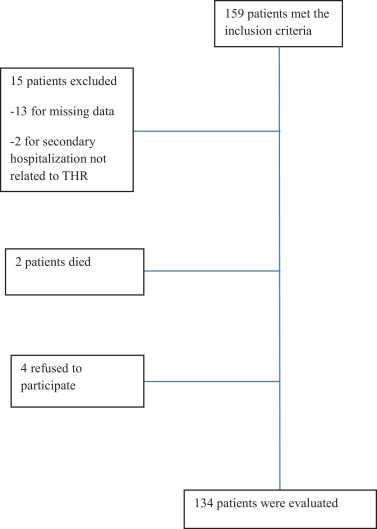
One hundred fifty-nine (159) patients met the inclusion criteria. Thirteen patients were excluded because of missing data, 3 due to hospital readmission lasting more than a month for a health problem unrelated to the surgery. Two patients died before having the surgery. Four patients did not want to participate to the phone interview and 3 patients were lost to the touch. The remaining 134 patients were included in the study ( Fig. 1 ).
The study cohort included 94 women and 40 men, i.e. a female-to-male ratio of 2.35. Mean age was 71.6 ± 10 years. On average women were older than men ( Table 1 ).
| Men ( n = 40) | Women ( n = 94) | |
|---|---|---|
| Surgery in a private hospital | 72.3% | 77.5% |
| Mean length of stay in the surgical department (days) | 10 | 10 |
| Discharge to a PM&R center | 55% | 73.5% |
| Mean length of stay in the PM&R center (days) | 26 | 28 |
| Mean age (years) | 67 | 73.3 |
| Living in a rural area | 50% | 35% |
| Isolation | 35% | 28.5% |
| Accessible home | 32.5% | 35.5% |
| Use of technical aids for walking | 40% | 44% |
| Walking perimeter > 400 m | 62.5% | 48% |
| Home help | 2.5% ( n = 1) | 25% |
| Living alone | 43% | 72.5% |
| Mean RAPT | 8.8 | 6.2 |
| Patient’s preference for PM&R hospitalization | 78% | 82.5% |
| Mean Lequesne index of severity for osteoarthritis for the hip (0–24) | 12.4 | 13.7 |
| Comorbid conditions | 40% | 27% |
| Postoperative complications | 18.7% | 16% |
In 78% of cases, primary hip osteoarthritis was at the origin of the arthroplasty. The other causes were reintervention of a hip prosthesis after sepsis (8%), congenital hip dysplasia (6%), osteonecrosis (5/134), 3 post-traumatic dysplasia (3/134), two secondary THR where the etiology was not detailed (2/134) and one rheumatoid arthritis (1/134).
Patients were referred by 18 different surgeons and the surgeries took place in 9 different structures including 3 outside the region. In all, 101 patients had surgery in a private clinic and 33 in a public hospital. Mean length of stay (LOS) in the surgical ward was 10.0 ± 3.0 days. Mean LOS was significantly higher for patients discharged to a PM&R center ( P < 0.0001). Among all patients, 88/101 (66%) were discharged to a PM&R center and 46/101 (34%) went directly home. Mean LOS in a PM&R Center was 27 ± 13 days (min = 7; max = 84).
We found 22 postoperative complications, i.e. 16% of operated patients. These complications were blood transfusions (16 cases), prosthesis dislocation (2 cases), scar infections (2 cases) with subsequent surgery and urinary tract infections with fever (2 cases).
1.3.2
Difference between the discharge predicted by the RAPT and the real discharge destination
The discharge destination predicted by the RAPT was computed during the preoperative period by the PM&R physician, the real discharge destination corresponds to the decision taken by the surgical team during the postoperative period ( Table 2 ).
| Total population ( n = 134) | |
|---|---|
| Variables taken into account for the RAPT | |
| Age (less than 66 years/between 66 and 75 years/more than 75 years) | 41.5/34/24.5 |
| Sex (women/men) | 70/30 |
| Walking perimeter (homebound/between 200 and 400 m/ > 400 m) | 15.5/32/52.5 |
| Gait aids for walking (crutches or walking frame/single-point stick/none) | 6/36.3/57.7 |
| Home help (≥twice a week/none or once a week) | 15.5/84.5 |
| “Living alone” (yes/no) | 36/64 |
| Variables not taken into account for the RAPT | |
| Comorbid conditions (yes/no) | 31/69 |
| Knee Society Classification System (A/B/C) | 65/11/24 |
| Lequesne index (0–24) | 13.29 ± 4.16 |
| Home environment (rural/urban) | 40/60 |
| Isolated (yes/no) | 30/70 |
| Accessible home (yes/no) | 35.5/64.5 |
We focused mainly on the patients for whom the predicted discharge destination was different from the real discharge destination.
Among the 25 patients who had a RAPT score > 9 (value predicting a direct return home), 7 ended up staying in a PM&R center post-surgery. Their preoperative orientation criteria were: sex (3 women for 4 men), mean age 63.2 (±8.0) years, their maximum walking distance was always > 400 meters, none of them used technical aids for walking and none reported “living alone”. Two of these patients had at least one comorbidity. Regarding their living environment, 5 patients lived in rural areas, two patients were isolated. The home of these 5 patients was deemed not accessible. During the preoperative period, all these patients expressed a preference for staying in a PM&R center post-surgery. Postoperative criteria for being discharged to a PM&R center were hip prosthesis dislocation for one patient and the onset of pressure ulcers for another.
Their mean LOS in the PM&R center was significantly shorter than for the rest of the cohort (16.4 [±7.6] days).
Among the 44 patients who had a RAPT score < 6 (value predicting postoperative management in a PM&R center), three went home directly after discharge from the surgical ward. Their preoperative orientation criteria were: sex (3 women), age (65 for 2 of them and 82 for the third one) they were living alone, two were walking with a single-point cane, the third did not use any technical aid for walking, only one had a walking distance > 400 meters, the other two had a walking distance between 200 and 400 meters. Two of them wanted to do their physiotherapy at home and two patients had at least one comorbidity. Regarding their living environment, two patients reported living in a rural area, none felt isolated and only one had a home classified as not accessible. No postoperative criterion (such as a post-surgical complication) was found for these three patients.
Sixty-five (65) patients had a RAPT score between 6 and 9 (threshold values requiring specific postoperative rehabilitation care to promote a direct return home). During the preoperative period, 59 patients wanted to be discharged to a PM&R center. At the end, 42 patients were in fact discharged to a PM&R center (mean RAPT score = 7) and 23 patients were discharged home (mean RAPT score = 7.36). Among the 23 patients who were discharged home, 19 had expressed during the preoperative period their preference for going to a PM&R center after THR surgery. Among the 42 patients who were discharged to a PM&R center, only two of them had wanted to go home after surgery. They both had a RAPT score of 6 and did not present any postoperative complications that could have explained their final discharge to a PM&R center.
1.3.3
Inferential analysis of the RAPT and its variables
The RAPT score was significantly correlated to being discharged to a PM&R center, whether studied as a continuous quantitative variable from 1 to 12 or divided into three categories (< 6, 6 to 9 and > 9) with P < 0.0001 for both analytic modes ( Tables 3 and 4 ).
| RAPT < 6 Discharge to a PM&R center | 6 ≤ RAPT ≤ 9 Discharge home under specific care | RAPT > 9 Direct discharge home | |
|---|---|---|---|
| Number of patients | 44 | 65 | 25 |
| Surgery in a private hospital | 82% | 72% | 72% |
| Rehabilitation in a PM&R center | 93% | 65% | 28% |
| MLS in the surgical department | 10.5 | 10.1 | 8.8 |
| MLS in the rehabilitation center (days) | 29.9 | 26.5 | 16.4 |
| Mean age (years) | 78 | 70 | 63 |
| Female patients | 97.7% | 62% | 44% |
| Living in a rural environment | 36% | 39.4% | 48% |
| Isolated | 27.3% | 33.3% | 28% |
| Accessible home (yes/no) | 43% | 30.3% | 36% |
| Living alone (yes/no) | 97.7% | 65% | 0% |
| Home help (yes/no) | 40% | 3% | 4% |
| Absence of gait aids | 30% | 62% | 96% |
| Walking perimeter > 400 m | 25% | 59% | 84% |
| Mean Lequesne index (0–24) | 14.8 | 12.9 | 11.4 |
| Presence of at least one comorbidity | 38.6% | 31.8% | 16% |
| Patient’s preference for being hospitalized in a PM&R center | 84% | 91% | 48% |
| Postoperative complications | 23% | 12% | 16% |
| P value | |
|---|---|
| Variables included in the RAPT | |
| Age (in 3 classes) | 0.0144 |
| Sex | 0.0009 |
| Technical aids for walking | 0.0327 |
| Living alone | < 0.0001 |
| RAPT | |
| Discontinuous > 6/6 to 9/ > 9 | < 0.0001 |
| Continuous 1–12 | < 0.0001 |
| Variables not included in the RAPT | |
| Age (continuous quantitative variable) | 0.0041 |
| Lequesne index | 0.0420 |
| Patient’s preference | < 0.0001 |
| Length of stay | < 0.0001 |
The “age” variable was significantly correlated to being discharged to a PM&R center ( P = 0.0144). In all, 41% of patients ( n = 56) were 75 years or older and 75% of them were hospitalized in a PM&R center after THR. Among the 24% ( n = 33) of patients < 65 years, only 45% were discharged to a PM&R center.
The “female” variable was statistically associated with a discharge to a PM&R center ( P = 0.0009). Overall, 74% of women pursued their rehabilitation in a PM&R center vs. 45% of men; on average in this cohort women were older than men. They also reported “living alone” more often than men. Only one man had home help vs. 25% of women ( Table 1 ). The “living alone” variable was significantly correlated to being discharged to a PM&R center. It was the most significant criterion within the RAPT with P < 0.0001, 80% of patients who reported “living alone” were discharged to a PM&R center vs. 60% of patients who reported not living alone.
Needing technical aids for walking made staying in a PM&R center more likely. Fisher’s exact test found P = 0.0327 when applied to the RAPT’s three sub-variables (no technical aids, single-point cane and crutches or walker). In our study, two variables included in the RAPT showed no statistical correlation to a PM&R discharge post-surgery: preoperative “walking perimeter” ( P = 0.3175) and “home help” ( P = 0.1139) ( Table 5 ).
| P value | |
|---|---|
| Variables included in the RAPT | |
| Walking perimeter | 0.3175 |
| Home help | 0.1139 |
| Variables not included in the RAPT | |
| Public or private nature of the structure where the surgery took place | 0.1125 |
| Rural or urban living environment | 0.8240 |
| Isolation | 0.7016 |
| Accessible home | 0.8069 |
| Comorbid conditions | 0.0908 |
| Knee Society Classification System | 0.0856 |
Patient’s preference was a variable not accounted for in the RAPT and in fact had the strongest statistical link with postoperative rehabilitation in a PM&R center ( P < 0.0001). During the preoperative period, 109 patients expressed a preference for being hospitalized in a PM&R center post-surgery, i.e. 80% of the total cohort. At the end, 74% of them ( n = 81) were in fact discharged to a PM&R center. Most patients for whom the final discharge destination did not match their preoperative preference ( n = 20) had a RAPT score between 6 and 9. For the 25 patients who wanted to be discharged home directly, 6 were in fact discharged to a PM&R center, 4 of them had a RAPT score < 6.
1.3.4
Logistic regressions
Several logistic regression models were tested, including or not the patient’s preference or mean age ( Table 6 ). The global model, taking into account patient’s preference and age, was the best fit for all the data including age, patient’s preference, being female and living alone. Environmental variables not taken into account by the RAPT such as urban or rural environment, sensation of being isolated, accessible home and public or private nature of the structure where the patient had THR surgery were also analyzed. No statistical relationship was found between these variables and being discharged to a PM&R center. Overall, 60% of patients recruited in this study lived in an urban environment vs. 40% who lived in a rural setting.
| Variables to be explained | Odds ratio | 95% Confidence interval | P | |
|---|---|---|---|---|
| Mean age | 1.028 | 1.018 | 1.038 | < 0.0001 |
| Sex | 0.373 | 0.154 | 0.902 | 0.0286 |
| Living alone | 0.247 | 0.106 | 0.576 | 0.0012 |
| Patient’s preference | 0.163 | 0.056 | 0.472 | 0.0008 |
In 66% of cases, patients who were discharged to a PM&R center post-surgery lived in urban areas vs. 64% of patients who lived in rural areas. Thirty percent (30%) of patients reported feeling isolated, and out of these patients 68% of them were discharged to a PM&R center but the decision was not related to this feeling of isolation. Sixty-six percent (66%) of patients whose home was considered not accessible were hospitalized in PM&R center, vs. 64% of patients who had accessible homes.
The presence of comorbidity, evaluated alone or using the Knee Society Classification System, was not statistically associated with a discharge to a PM&R center. Overall, 69% of patients did not have comorbid conditions and out of these, 61% were discharged to a PM&R center, for patients with at least one comorbid condition, the PM&R hospitalization rate was 76%.
A high Lequesne index was correlated to a higher PM&R hospitalization rate ( P = 0.0420). Mean Lequesne index value was 13.2 (±4 points); (min = 4, max = 23.5) for the entire cohort with a mean value of 13.7 points for patients discharged to a PM&R center vs. 12.5 points for patients discharged home.
1.4
Discussion
This study conducted on 134 patients with THR surgery confirmed the validity of the RAPT score as a decision-making tool for discharge outcomes. Thus, a low RAPT score is significantly correlated to a higher rate of PM&R hospitalizations; conversely a high RAPT score is significantly correlated to being discharged home post-surgery. Furthermore, we validated that old age, living alone and patient’s preference were determining factors, analyzed during the preoperative period, for deciding on a PM&R stay after THR surgery.
1.4.1
Length of stay
The mean LOS in surgical wards was significantly shorter when patients were returning home directly ( P < 0.0001). Patients with a RAPT score > 9 were most likely to be discharged home, thus mean LOS in this category was also shorter. The most likely hypothesis to explain this shorter LOS when patients were discharged home, resides in the delay needed to obtain a bed in a PM&R center. These difficulties in transferring patients to a PM&R center can negatively impact the entire hospital care pathway and it shows the relevance of using the RAPT to anticipate, right from the preoperative period, the rehabilitation needs of a patient in order to affect the discharge rate to a PM&R center.
1.4.2
Demographic criteria
For our cohort and among the various RAPT criteria, old age and being female were the two criteria correlated to the highest probability of being discharged to a PM&R center. This relationship between the need for rehabilitation and age is validated by an analysis of the literature . Among other factors, it is linked to the absence of a spouse or husband able to care for the patient at home, the frequent association of several other pathologies and a precarious functional status.
However, it is relevant to note that age appears significantly correlated through univariate and multivariate analyses when it is expressed in means and not by age groups. When age is expressed by groups, it does not show a correlation which brings us to wonder if the threshold values for these age groups are appropriate. An updated calculation of these age groups would require a new study on a larger number of subjects.
Conversely, data appear more contradictory for the variable “being female”. Out of the various studies that considered sex as a relevant variable , two did not report any statistical link between gender and discharge to a PM&R center. The mean age of female patients in these two studies, just like the other four studies found in the literature, was lower than for our cohort (63.6 and 65.6 years vs. 71.6 years). In our cohort, women were older and most of them lived alone.
1.4.3
Psychosocial criteria
Psychosocial criteria are also highly relevant in postoperative care management for these patients. Again, this study highlights that patient’s preference was the most important criterion in determining discharge destination, validating the results of previous studies that included this variable . In fact, Oldmeadow et al. chose to extract this variable from the RAPT because its statistical weight was too important . Furthermore, “living alone” was also strongly correlated to a transfer to a PM&R center in accordance with the literature . Heine et al. , based on semi-structured interviews, reported the importance of feeling confident and safe as well as the role of family and friends in the decision-making process for postoperative management. However, in our cohort we did not find any statistical relationship between discharge to a PM&R center and having home help for tasks such as cleaning and nursing care or having meals delivered contrarily to Oldmeadow et al. who included this item in the RAPT . The very low incidence of home help for patients in our cohort (15% had home help at least twice a week) can be responsible for the low statistical power of this variable.
1.4.4
Functional impairments
In this study, preoperative functional impairments evaluated by the walking perimeter were not statistically correlated to a transfer to a PM&R center post-surgery, which contradicts the RAPT validation study . It is quite possible that having evaluated the walking perimeter during the preoperative interview without an actual walking test could have altered the validity of the collected data. We did however find a statistical relationship between discharge to a PM&R center and using technical aids for walking during the preoperative period . However, Lequesne index values, which also evaluates functional impairments, were significantly correlated to discharge outcomes ( P = 0.0420), this relationship was not validated when the Lequesne index was included in a logistic regression that comprised the RAPT variables previously found significant during the inferential analysis. Preoperative functional impairments were studied in two other publications with contradictory results . It was difficult to compare them since the evaluation criteria were different in both studies. De Pablo et al. , using a score adapted from the Harris Hip Score, which included functional items (technical aids, going up the stairs, walking perimeter and limping), did not report a statistical relationship between preoperative functional impairments and discharge to a PM&R center post-surgery. Similarly, in their study evaluating patients during the preoperative period using the Preadmission Discharge Planning Instrument taking into account gait and transfers separated into two variables (analyzed independently or not), Mahomed et al. did not find any statistical link with a discharge to a PM&R center.
1.4.5
Patient’s preference
Our study also validated the importance of taking into account the patient’s preference for postoperative care management; this variable had the heaviest statistical weight in the linear regression model. Thus, when the RAPT score points towards a direct return home (score > 9), or the need for staying in a PM&R center post-surgery (score < 6), in most cases it is in accordance with the patient’s preference. For these same scores, when the real discharge destination was not the one originally determined by the RAPT, the patient’s preference was in fact different than the discharge destination predicted by the RAPT and could have indeed influenced the real discharge destination. In fact, it is for the intermediate RAPT values (scores between 6 and 9 points) that the decision on postoperative management was the most uncertain. Oldmeadow et al. reported that targeted rehabilitation care during the immediate postoperative period could multiply by three the discharge home rate in this subpopulation of patients . Furthermore, specific rehabilitation care before surgery, associating an exercise program with targeted therapeutic education, could have an influence on modifying the postoperative discharge destination . To our knowledge, no study has evaluated the impact of a rehabilitation intervention on the patient’s preference during the postoperative period.
1.4.6
Other criteria
We did not find any environmental criteria, not accounted for in the RAPT, such as the type of structure (public hospital or private clinic), home environment (rural or urban), isolation and home accessibility, which could have influenced the orientation of patients during the postoperative period. This validates the data from the literature . Furthermore, we did not highlight any relationship between patients hospitalized in a PM&R center and comorbid conditions. Comorbid conditions were studied either separately or as a score (Charlston Comorbidity Index , score ASA ). The results are either contradictory (ASA score and obesity) , or discard the impact of comorbid conditions (Charlston Comorbidity Index, COPD, cardiac pathology, rheumatoid arthritis, neurological or mental disorders) . Medical criteria seem to have very little influence on the patient’s postoperative management after total hip arthroplasty. One can imagine that THR surgery is only scheduled when the patient’s comorbid conditions are stable, do not present a risk for the anesthesia and in fact will not negatively impact the postoperative autonomy.
1.4.7
Limits
In our study, 80% of patients over the age of 75 were women and 80% of them reported “living alone”. Conversely, among men 75 years or older (20% of the cohort), only 44% of them reported “living alone”. The statistical analysis of some factors was in fact negatively affected by the homogeneity of our sample, which led to unbalanced patient subgroups. Thus, it was difficult to interpret the “home help” variable since only very few subjects reported having home help during the preoperative interview.
Regarding technical aids for walking, they were significantly correlated to discharge outcomes in the inferential analysis but not validated by the logistic regression. This variable remained very discriminative for predicting discharge outcomes in the original study by Oldmeadow et al. ( P < 0.0001) .
The repartition of patients in the three categories of the “technical aids” was unbalanced. In fact 78 patients did not use any technical aids during the preoperative period, 49 used a simple single-point cane and only 8 patients used crutches or a walking frame. Among the latter, none were discharged home directly. A study conducted on a larger cohort could help validate definitely this variable and address the above-mention issue of the solidity of threshold values for the age groups.
Another limit of our study is the lack of data on the elements that truly impacted the actual discharge decision taken by the surgical team after surgery. Data collection on the real discharge destination was performed retrospectively, thus it was impossible to know what element most influenced the final decision, i.e. patient’s preference or objective postoperative criteria such as autonomy . This could be further investigated by conducting semi-directed interviews on factors influencing patient’s preference as suggested by Heine et al. . According to the importance of the patient’s preference on discharge outcomes, it was decided by the authors not to re-integrate it into the RAPT, nevertheless this issue remains open. Finally, using a tool, such as the RAPT, to help the decision-making process on discharge outcomes is highly related to the healthcare system. The RAPT was validated in Australia and used in different healthcare systems such as Singapore or France , countries where rehabilitation care units exist. It is obvious that in countries that do not have such structures as part of their healthcare system, the impact of the RAPT is much more limited, even if in our opinion, its use during the preoperative period remains quite relevant to prepare the patient to postoperative management and implement the necessary measures to improve the conditions of a safe discharge home.
1.5
Conclusion
Multiple factors influence the postoperative management (direct return home or transfer to a PM&R center) of patients after total hip replacement surgery. This study validates the relevance of the RAPT to help clinicians plan discharge outcomes after total hip arthroplasty. The patient’s preference remains the prominent variable for deciding on discharge outcomes after THR surgery, it is legitimate, as proposed by Oldmeadow et al. to not integrate this variable into the RAPT but rather to collect it and confront it to the RAPT score in order to take the decision with the patient, on discharge destination post-surgery.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
Les lésions de l’articulation de la hanche, le plus souvent liée à l’arthrose, peuvent être à l’origine de douleurs, de limitation articulaire responsable d’incapacité fonctionnelle. Lorsque le traitement médical, associant des mesures pharmacologiques et non pharmacologiques, qui doit être proposé en première intention, ne permet plus de contrôler l’affection , l’arthroplastie totale de hanche (PTH) est recommandée. La fréquence de cette intervention est en constante augmentation dans les pays industrialisés en raison d’une augmentation de l’incidence de l’arthrose lié au vieillissement de la population et à l’allongement de la durée de la vie. Aux États-Unis, les perspectives d’augmentation d’arthroplastie sont de l’ordre de 174 % d’ici 2030 . Dans la population française, 105 000 personnes auraient bénéficié d’une arthroplastie totale de hanche en 2000, ce qui placerait cette intervention au 10 e rang des interventions chirurgicales .
Au cours de ces vingt dernières années, la prise en charge postopératoire des arthroplasties totales de hanche s’est profondément modifiée dans l’ensemble des pays industrialisés. La tendance commune, dans un contexte de réduction des coûts de santé, va vers une diminution significative de la durée de séjour en service de chirurgie qui est passée de trois semaines dans les années 1970 à moins d’une semaine actuellement .
Cette réduction a pour corollaire une augmentation des transferts et par conséquent d’une augmentation potentielle du nombre de séjours en service de rééducation. Il existe par ailleurs, une tendance forte à favoriser le retour direct à domicile après une intervention entre autre pour des raisons médico-économiques. Ainsi, Lavernia et al. se sont intéressés aux coûts de la prise en charge postopératoire après PTH en 2003. Une rééducation à domicile revenait en moyenne à 2405 dollars alors qu’une rééducation en centre coûtait en moyenne 13 435 dollars. Ramené à l’ensemble de la population américaine, le coût total de la rééducation postopératoire après pose de PTH était estimé à 3,2 milliards de dollars .
L’analyse de la littérature concernant l’orientation des patients après arthroplastie de hanche, retrouve une grande hétérogénéité de pratique d’un pays à un autre mais également à l’intérieur d’un même pays. Ainsi, une étude canadienne observe un recours aux hospitalisations en rééducation variant de 0 à 86 % selon l’établissement où a lieu l’intervention . En France, l’étude de Maravic et Landais en 2006 retrouve un taux d’hospitalisation en rééducation de 33 % alors que ce taux est de 46 % dans une étude menée sur une population dans la région Provence-Alpes-Côte-d’Azur . En revanche, une étude menée en Angleterre montre que seuls 6 % des patients effectuent un séjour en service de rééducation .
Les études disponibles dans la littérature qui s’intéressent aux critères associés à un transfert en service de rééducation sont restreintes et de faible niveau de preuve scientifique. Elles font apparaître que l’orientation vers ce type de service est multifactorielle. Les facteurs les plus importants sont un âge élevé, l’incapacité fonctionnelle, le fait de vivre seul et la préférence du patient . Compte tenu de ces éléments, le recours à des outils d’aide à la décision dans l’orientation des patients après chirurgie, à utiliser en amont de l’intervention chirurgicale semble nécessaire. En effet, la diminution de la durée moyenne de séjour (DMS) en court séjour et la tendance actuelle à transférer les patients directement à domicile incitent à déterminer des critères d’évaluation objectifs permettant de mieux orienter les patients afin de leur proposer une prise en charge adaptée à leurs besoins en préopératoire et en postopératoire immédiat.
L’analyse de la littérature retrouve deux outils d’aide à la décision. Celui proposé par Bindelglass et al. prend en compte l’âge du sujet, les conditions du domicile et la qualité de vie (SF36). Sa principale limite est son absence de validation de façon prospective. En revanche, le RAPT (Risk Assessment and Prediction Tool) a été validé de façon prospective . Cet outil prend en compte l’âge, le sexe, la capacité fonctionnelle préopératoire avec ou sans aide technique, le support social à domicile, le fait de vivre seul ainsi que la préférence du patient. Le score total est obtenu par addition des six variables. Il permet de déterminer trois sous-groupes de patients :
- •
un score > 9, les patients pouvant rentrer directement à domicile et effectuer leur rééducation en ambulatoire ;
- •
un score < 6, les patients nécessitent un transfert en service de rééducation ;
- •
les patients ayant un score entre 6 et 9 constituent une population intermédiaire pour laquelle il est difficile de déterminer en préopératoire leur orientation postopératoire.
Une fois ce score établi, la décision d’orienter le patient vers une structure de rééducation est prise en tenant compte à la fois de la valeur du RAPT mais également de la préférence du patient.
Enfin, cet indice a été utilisé dans une seconde étude prospective où son usage associé à une prise en charge intensive en postopératoire a permis de modifier l’orientation des patients prévue initialement en préopératoire . Dans cette seconde étude, les auteurs ont également confirmé la valeur prédictive de l’indice sur une cohorte de 50 patients ayant bénéficié d’une arthroplastie totale des membres inférieurs (valeur préopératoire du RAPT significativement corrélée avec la destination réelle de sortie des patients, F = 2029, p = 0,003). La principale limite de ce travail concernait la population de l’étude comportant des patients opérés d’une arthroplastie totale de la hanche ou du genou sans faire de différence entre ces deux sous-populations.
Le RAPT a fait l’objet d’une validation en français selon une procédure de traduction/contre-traduction . Il a également fait l’objet de plusieurs publications récentes dans des cohortes de patients opérés d’une prothèse totale de genou dans des systèmes de soins différents et son utilisation est recommandée dans les parcours de soins publiés par la SOFMER (Société française de médecine physique et de réadaptation) .
L’objectif principal de cette étude est de vérifier la validité du F-RAPT, outil d’aide à la décision pour orienter les patients opérés d’une arthroplastie totale de la hanche.
2.2
Patients et méthode
2.2.1
Patients
L’ensemble des patients adressés en consultation de rééducation préchirurgicale avant arthroplastie totale de hanche sur une année pleine a été étudié rétrospectivement. Les patients sont adressés à cette consultation par leur chirurgien après que la décision opératoire a été prise pour envisager les mesures de rééducation pré- et postopératoire. Ils sont reçus par une équipe pluridisciplinaire comportant un ergothérapeute, un travailleur social et un médecin de MPR. Ils bénéficient lors de cette consultation de la prescription de kinésithérapie préopératoire, de conseils sur les aides techniques et enfin d’une information sur les objectifs de la rééducation postopératoire. L’ensemble des services de chirurgie orthopédique, hospitaliers et privés, de l’agglomération de Clermont-Ferrand a participé à l’étude.
2.2.2
Critères recueillis
L’orientation réelle, retour direct à domicile ou transfert en service de rééducation après chirurgie était recueillie ainsi que les durées de séjour en service de chirurgie et en service de rééducation le cas échéant.
L’ensemble des critères du RAPT a été pris en compte : âge, sexe, périmètre de marche préopératoire, utilisation d’aides techniques pour la marche, présence d’une personne à domicile au décours de l’intervention pouvant aider l’opéré, préférence du patient pour l’orientation postopératoire (transfert vers une structure de rééducation versus retour direct à domicile).
D’autres critères, pouvant modifier l’orientation des patients issues d’une des données de la littérature et de l’avis d’experts (ergothérapeute, assistante sociale, médecin de MPR), ont également été pris en compte : type de l’établissement où a lieu l’intervention (privé/public, centre hospitalier/clinique), durée de séjour (DDS) en service de chirurgie, et en service de rééducation le cas échéant, comorbidités, Knee Society Classification System , incapacité fonctionnelle mesurée par l’indice de Lequesne , lieu de vie (rural ou urbain), isolement, complications postopératoires, accessibilité du domicile. L’accessibilité du domicile a été déterminée à partir de l’avis d’experts (médecins MPR et ergothérapeute) en fonction de trois sous-items qui étaient l’aménagement du domicile, l’accès intérieur et extérieur. Si la réponse à l’un de ces trois sous-items était négative, le domicile était considéré comme inaccessible. L’accès extérieur était côté inaccessible s’il existait au moins une volée de marches pour accéder au domicile ou l’absence d’ascenseur pour accéder à un étage. L’accès intérieur était côté inaccessible si la chambre, la salle de bain et la cuisine n’étaient pas sur le même palier ou s’il n’existait pas de possibilité d’installer une chambre sur le même palier que la cuisine et la salle de bain. L’aménagement du domicile concernait la salle de bain et les toilettes avec la présence d’une douche avec tapis antidérapant, barre d’appui et la présence d’un réhausseur.
2.2.3
Suivi des patients
Le recueil des données était réalisé selon deux modes. Pour les patients transférés en service de rééducation, les données étaient extraites des dossiers d’hospitalisation des services de rééducation les ayant accueillis. Pour les patients n’ayant pas séjourné dans un service de rééducation, ils étaient contactés directement par téléphone.
2.2.4
Considérations éthiques
En l’absence de bénéfice individuel direct et/ou d’atteinte à l’intégrité des personnes, l’étude n’a pas fait l’objet d’une déclaration au CPP (comité pour la protection des personnes). En l’absence de randomisation et d’atteinte à l’intégrité physique ou psychologique aucun consentement écrit n’était requis. Le consentement oral des patients a été recueilli avant l’inclusion dans l’étude après les avoir informé de l’objectif du travail.
Cette étude a été menée conformément aux bonnes pratiques cliniques et en accord avec la déclaration d’Helsinki de l’Association médicale mondiale (Tokyo 2004, révisée).
2.2.5
Analyse statistique
Le premier temps de l’analyse concerne la description de la population. Les données quantitatives sont exprimées à l’aide des valeurs moyennes et des écarts-types, les variables quantitatives en données brutes et pourcentages.
Secondairement, une analyse inférentielle est réalisée pour déterminer si les variables d’intérêt (comprises dans le RAPT puis non comprises dans le RAPT) ont une influence sur l’orientation postopératoire des patients. Pour les variables qualitatives et quantitatives non continues, le test du Chi 2 a été utilisé. Pour les effectifs théoriques inférieurs à 5, un test exact de Fisher est utilisé. Pour les variables quantitatives continues, un test non paramétrique de Wilcoxon est utilisé.
À l’aide d’une équation de régression logistique, le caractère prédictif d’orientation vers un service de rééducation des variables prises en compte dans le RAPT, ainsi que leur poids relatif sont déterminés. Seuls les facteurs ayant une valeur statistiquement significative avec p < 0,05 en analyse univariée ont été inclus pour la régression logistique.
L’ensemble des analyses a été effectuée sur logiciel SAS.
2.3
Résultats
2.3.1
Analyse descriptive
Cent cinquante-neuf (159) patients répondaient aux critères d’inclusion. Treize patients ont été exclus en raison de données manquantes, trois patients en raison d’une ré-hospitalisation pour une durée supérieure à un mois pour un problème de santé sans rapport avec l’intervention. Deux patients sont décédés avant d’avoir pu bénéficier de l’intervention. Quatre patients n’ont pas voulu répondre à l’enquête téléphonique et trois patients ont été perdus de vue. Les 134 patients restant constituaient la population de l’étude ( Fig. 1 ).