Total Shoulder Arthroplasty for Glenohumeral Arthritis
E. Scott Paxton
Gerald R. Williams Jr.
DEFINITION
Glenohumeral arthritis is characterized by loss of articular cartilage and varying degrees of soft tissue contracture, rotator cuff dysfunction, and bone erosion, depending on the underlying arthritic condition.
The results of surgical treatment are largely dependent on the integrity of the rotator cuff; therefore, glenohumeral arthritides are often subdivided on this basis.
Common arthritic and related conditions that generally involve an intact or reparable rotator cuff include osteoarthritis, posttraumatic arthritis, and avascular necrosis.
Although some patients with inflammatory arthritides such as rheumatoid arthritis have intact or reparable rotator cuffs, the rotator cuff is torn or dysfunctional in many patients. When reference is made to patients with inflammatory arthritis in this section, it pertains to the subset of patients in whom the cuff is intact or reparable.
ANATOMY
The pertinent surgical anatomy can be divided into bone, ligaments, muscles, and neurovascular structures.
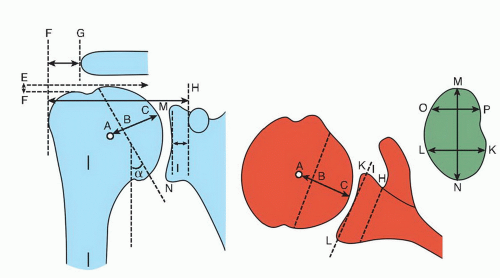
Normal osseous relationships include humeral head center, thickness, and radius of curvature, humeral neck-shaft angle, humeral head offset, glenohumeral offset, greater tuberosityto-acromion distance, greater tuberosity-to-humeral head distance, glenoid radius of curvature, glenoid size, glenoid version, and glenoid offset (FIG 1).13,21
Humeral head radius and thickness are variable and correlate with patient size. Mean humeral head radius is about 24 mm, with a range of 19 to 28 mm. Mean humeral head thickness is about 19 mm, with a range of 15 to 24 mm.13,21
The ratio of humeral head thickness to humeral head radius of curvature is remarkably constant at about 0.7 to 0.9, regardless of patient height or humeral shaft size.13,21
The center of the humeral head does not coincide with the projected center of the humeral shaft. The distance between the center of the humeral head and the central axis of the intramedullary canal is defined as the humeral head offset and is about 7 to 9 mm medial and 2 to 4 mm posterior (FIG 2).2,21
Humeral retroversion averages 20 to 30 degrees, with a wide range of about 20 to 55 degrees.2,13,21 The vertical distance between the highest point of the humeral articular surface and the highest point of the greater tuberosity (ie, head to greater tuberosity height) is about 8 mm and shows a relatively small range of interspecimen variability.13
Humeral neck-shaft angle is defined as the angle subtended by the central intramedullary axis of the humeral shaft and the base of the articular segment and shows substantial individual variation. The average neck-shaft angle is 40 to 45 degrees (130 to 135 degrees), with a range of 30 to 55 degrees (120 to 145 degrees).2,13,21
Pertinent musculotendinous anatomy includes the deltoid, pectoralis major, conjoined tendon of the coracobrachialis and short head of the biceps, rotator cuff, and long head of the biceps.
Ligamentous structures that are potentially important in the surgical management of glenohumeral arthritis include the coracoacromial ligament and the glenohumeral capsular ligaments. In many cases of glenohumeral arthritis with an intact cuff, the anterior and inferior capsular ligaments are
contracted, resulting in restriction of external rotation and posterior humeral head subluxation.
Neurovascular structures are abundant and subject to potential injury during shoulder arthroplasty. The axillary artery and all of its branches, especially the anterior humeral circumflex, posterior humeral circumflex, and the subscapular arteries, are particularly vulnerable.
The entire brachial plexus traverses the anterior aspect of the shoulder and is subject to traction and other injuries. The two most pertinent nerves are the axillary nerve and the musculocutaneous nerve.
The axillary nerve is a terminal branch of the posterior cord of the brachial plexus and is composed primarily of motor fibers from the fifth and sixth cervical roots. It descends the anterior surface of the subscapularis to the inferior aspect of the joint capsule, where it courses through the quadrilateral space to enter the posterior aspect of the shoulder.
The musculocutaneous nerve is one of the terminal branches of the lateral cord of the brachial plexus that is anterior and lateral to the axillary nerve. It typically pierces the conjoined tendon of the coracobrachialis and short head of the biceps about 5 cm distal to the tip of the coracoid. However, this course is variable and the entry point into the conjoined tendon can be as proximal as 2 cm.
PATHOGENESIS
The biologic basis for glenohumeral arthritis is not known.
However, the loss of articular cartilage associated with primary osteoarthritis, posttraumatic arthritis, avascular necrosis, and other arthritides is, in some way, the result of imbalance in the normal cycle of cartilage damage and repair.
In some cases of posttraumatic arthritis, catastrophic cartilage damage associated with single event or repetitive trauma overwhelms the shoulder’s cartilage repair mechanisms and arthritis ensues.
Primary osteoarthritis may be associated with mechanical factors such as glenoid hypoplasia and increased retroversion. However, in many cases, no cause is evident. The final common pathway involves a release of degradative enzymes, such as collagenase, gelatinase, and stromelysin, and a variety of inflammatory mediators, which further damage the cartilage, and eventually, the underlying bone.
A detailed discussion of the pathogenesis of avascular necrosis is beyond the scope of this chapter. However, the development of glenohumeral arthritis in this condition is likely the result of advanced cartilage damage following collapse of the humeral head. Involvement of glenoid articular cartilage does not occur until the later stages of the disease when the irregular humeral head has been articulating with the previously normal glenoid surface.
Rheumatoid arthritis is characterized by activation of the immune system that leads to an influx of lymphocytes into the joint and synovial tissue, with subsequent release of a variety of cytokines, destructive enzymes, and mediators of inflammation such as interleukins and tumor necrosis factor. This autoimmune response is thought to be important in perpetuating joint destruction.25
NATURAL HISTORY
Glenohumeral arthritis of any type is characterized by progressive stiffness, pain, and loss of function.
Patients with primary osteoarthritis and many types of posttraumatic arthritis develop progressive loss of external rotation, posterior subluxation, and posterior glenoid bone loss. Large osteophyte formation, especially on the inferior humeral neck, is common. Full-thickness rotator cuff tears are distinctly uncommon and occur in 5% to 10% of patients.
Rheumatoid arthritis results in progressive regional osteopenia, central glenoid bone erosion, and rotator cuff tears. The prevalence of full-thickness rotator cuff tears in patients with rheumatoid arthritis of the shoulder is 25% to 40%.31 However, rotator cuff dysfunction and substantial partial tearing are extremely common.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with glenohumeral arthritis will give a history of chronic (years) shoulder pain and restricted motion, often with a recent (months) exacerbation. Posttraumatic arthritis is typically associated with a history of prior injury, such as fracture or dislocation, or surgery.
Pain is often worse with activity and usually interferes with sleep. Neck pain, distal radiation below the elbow, and numbness and paresthesias in the fingers and hand are uncommon and should suggest other potential causes of shoulder pain, such as cervical stenosis or cervical radiculopathy.
Bilateral involvement is common in primary osteoarthritis. Contralateral symptoms are often present but to a lesser extent.
Physical findings in patients with glenohumeral arthritis and an intact rotator cuff include the following:
Posterior joint line tenderness, especially in osteoarthritis associated with posterior subluxation18
Generalized atrophy or flattening of the shoulder from long-term lack of function
Posterior prominence of the humeral head in cases of posterior subluxation
Symmetric loss of active and passive range of motion (FIG 3)
Disproportionate loss of external rotation in comparison to other motions, especially in osteoarthritis or after capsulorrhaphy arthropathy18
Increased pain with passive stretch of the capsule at the end range of motion, especially external rotation
Intact neurologic function, except in rare patients with prior neurologic injury from trauma or surgery
IMAGING AND OTHER DIAGNOSTIC STUDIES
Glenohumeral arthritis is a radiographic diagnosis. Routine radiographs should include anteroposterior (AP) views in internal and external rotation and an axillary view.
Radiographic findings in primary osteoarthritis include subchondral sclerosis and cyst formation, osteophyte formation, and asymmetric posterior joint space narrowing (FIG 4A,B).18
In cases of posttraumatic arthritis, radiographs may reveal retained hardware.
Glenoid deformity in osteoarthritis has been classified by Walch et al33 according to the presence of posterior subluxation and posterior bone deformity:
Type A: centered
Type B: posteriorly subluxated (B1) and posteriorly subluxated with posterior erosion (B2)
Type C: posteriorly subluxated with increased retroversion (hypoplasia)

FIG 3 • The hallmark of glenohumeral osteoarthritis is symmetric loss of both active and passive range of motion (A), especially external rotation (B).
Computed tomography (CT) scans are helpful in quantifying bone loss in patients with posterior subluxation (FIG 4C).
Magnetic resonance imaging (MRI) is useful in patients with rheumatoid arthritis to determine rotator cuff integrity (FIG 4D).
Electromyography may be used in patients suspected of having posttraumatic or postsurgical nerve injuries.
Medical consultation is warranted in patients with substantial comorbidities.
DIFFERENTIAL DIAGNOSIS
Frozen shoulder
Posttraumatic or postsurgical infection
Cervical stenosis
Cervical radiculopathy
Neoplasm
NONOPERATIVE MANAGEMENT
Avoiding activities that are painful or place an undue strain on the shoulder, such as weightlifting, is important.
Nonsteroidal anti-inflammatory medications may be helpful in reducing pain and inflammation.
In patients with rheumatoid arthritis, rheumatologic consultation for maximizing medical treatment is helpful.
Glucosamine chondroitin and other nutritional supplements may reduce the pain associated with arthritis, despite the relative lack of standardized data.
Intra-articular corticosteroid injections are almost always helpful, but the relief is often only temporary.
Hyaluronic acid derivatives are not yet approved by the U.S. Food and Drug Administration for use in the shoulder but may be of benefit in the future.
Therapeutic exercises should be used judiciously. Stretching to maintain flexibility may be helpful, but vigorous exercises may increase pain.
SURGICAL MANAGEMENT
Surgical options are considered when pain and dysfunction justify surgical intervention, nonoperative management has failed, medical comorbidities do not preclude surgery, and the patient is willing to accept the risks of surgery and the responsibility of postoperative rehabilitation and activity limitations.
Nonprosthetic options such as arthroscopic or open débridement are indicated in patients who are too young and active for any type of prosthetic replacement.
Prosthetic options include hemiarthroplasty, hemiarthroplasty plus biologic resurfacing, and total shoulder replacement.
Total shoulder replacement with a polyethylene glenoid component provides the most predictable pain relief but has the disadvantage of progressive polyethylene wear and eventual component loosening.29
The relative indications for hemiarthroplasty, hemiarthroplasty with biologic resurfacing, and total shoulder arthroplasty are controversial, vary among surgeons, and must be individualized according to patient age, activity level, and bone deformity, among other factors.
Similarly, the type of implant can be individualized according to patient factors and surgeon preference.
Concentricity of the joint, without subluxation, likely improves prosthetic performance in all circumstances. Therefore, fixed subluxation should be corrected when possible. Attempt should also be made to correct glenoid retroversion to the greatest degree possible, especially in the case of B2 glenoids, as component retroversion has been associated with increased radiographic osteolysis.12 Options include contracture release and correction of bone deformity with some combination of asymmetric reaming, bone grafting, and specialized components.
General principles that summarize procedural and implant indications in patients with glenohumeral arthritis and an intact or reparable cuff include the following:
Total shoulder arthroplasty is preferred with adequate glenoid bone, age younger than 50 years, and sedentary or moderate activity levels.
Hemiarthroplasty is favored in patients with normal or minimally involved glenoids, inadequate glenoid bone, age of 50 years or younger, and activity levels that include weightlifting or other strenuous activity.
When substantial reaming or resurfacing of the glenoid is planned, the procedure is facilitated by removing the humeral head rather than resurfacing it. Currently, stemmed implants are most popular, but implants with metaphyseal fixation may be useful in patients with adequate bone quality.
These principles are merely guidelines and should be individualized.
The following sections will cover the technical aspects of total shoulder arthroplasty with and without bone loss, including asymmetric reaming, augmented glenoid components, and glenoid bone grafting.
Preoperative Planning
Preoperative radiographs and CT scans should be reviewed to quantify humeral subluxation (especially posterior in osteoarthritis), version, and glenoid bone loss. This will identify the need for asymmetric glenoid reaming, augmented glenoid components, or a bone graft.
If the goals of asymmetric reaming are to correct glenoid deformity and to contain all fixation appendages of the glenoid component within the glenoid vault, the extent of reaming should be limited to about 5 mm or 15 degrees. If greater correction is desired, arrangements for glenoid bone grafting should be made. As little subchondral bone as possible should be removed as this correlates with glenoid component subsidence.34
We typically use an augmented glenoid component (Global Steptech Anchor Peg Glenoid, DePuy, Warsaw, IN) when eccentric/posterior bone loss is between 3 mm and 11 mm. We asymmetrically ream 2 mm and use a 3-, 5-, 7-, or 9-mm augmented component to restore the native glenoid version.
If posterior bone loss is greater than 11 mm, a bone graft must be used behind the glenoid component to restore the anatomic version and to avoid medialization of the joint line.
Preoperative radiographs should be templated to gain an appreciation of the humeral head size, canal diameter, and neck-shaft angle. In patients with highly varus (115 to 120 degrees) or valgus (145 to 150 degrees) neck-shaft angles in whom cementless fixation of a stemmed implant is planned, alterations in the level of the humeral cut or the use of a prosthesis with neck-shaft angle variability will be required. Canal diameter should also be examined, especially if the patient is a small statured woman, as a standard humeral stem may not fit in this patient and a humeral resurfacing may need to be available.
MRI scans should be read for substantial rotator cuff abnormalities in rheumatoid patients and others suspected of having rotator cuff tears.
All other relevant preoperative data should be reviewed, including consultations from medical colleagues. The presence of all surgical implants and instruments should be verified.
Passive range of motion should be measured intraoperatively, before positioning, to determine the need for contracture release. In particular, the degree of passive external rotation loss may dictate the method of subscapularis reflection and repair.
Subscapularis shortening is typically not a substantial factor in passive external rotation loss, unless the patient has had a prior subscapularis shortening or tightening procedure (eg, Putti-Platt or Magnuson-Stack) or the contracture is particularly severe (eg, external rotation of -30 degrees or more) and long-standing.
Methods of managing the subscapularis include intratendinous incision and anatomic repair, lesser tuberosity osteotomy and anatomic repair, lateral tendinous release with medial advancement, and Z-lengthening.
Recent evidence suggests that lesser tuberosity osteotomy is associated with better subscapularis function than soft tissue reflection and repair.7,22,27 However, randomized comparison data do not show an advantage to lesser tuberosity osteotomy versus a subscapularis peel.15,16 In addition, a recent study documents good postoperative subscapularis function with tenotomy and soft tissue repair.3
Our current preference for subscapularis management in primary shoulder arthroplasty is lesser tuberosity osteotomy and anatomic repair, with the following exceptions:
Rheumatoid arthritis with substantial erosion of the subscapularis attachment site on MRI
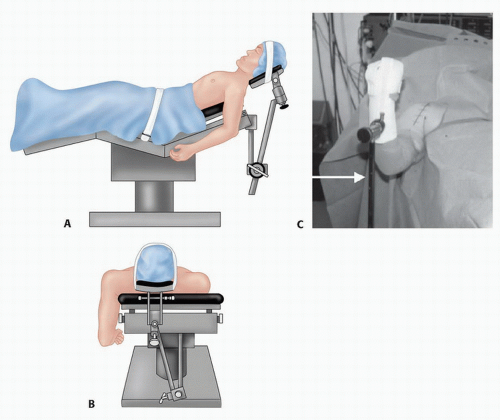
FIG 5 • A. Shoulder arthroplasty is carried out with the patient in the semirecumbent position; a special horseshoe-shaped headrest may improve access to the superior aspect of the shoulder. B. Positioning should allow unrestricted adduction and extension to allow access to the humeral shaft. C. A mechanical arm-holding device may be used to help position the arm throughout the procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access