Abstract
Patients with spinal cord injuries are prone to knee hydrarthrosis (also known as “water on the knee”), which can cause pain, functional impairment and the restriction of social activities. Total knee arthroplasty is a potentially appropriate treatment. Here, we report on a patient presenting partial T12 AIS grade C paraplegia who was able to walk with two forearm crutches, an ankle-foot orthosis on the right leg and a knee-ankle-foot orthosis on the left leg. Thirteen years after the spinal cord injury, the patient presented with septic arthritis of the right knee, complicated by recurrent hydrarthrosis during standing and walking. Arthroscopy revealed advanced osteoarthritis. Total knee arthroplasty was performed, with very good functional and social outcomes two and half years after surgery.
Résumé
Les patients blessés médullaires sont prédisposés à développer des hydarthroses du genou ayant pour conséquence une limitation fonctionnelle et une entrave à la vie socioprofessionnelle. La prothèse totale du genou, indiquée à bon escient, peut constituer un traitement de choix. Nous rapportons l’observation d’un patient paraplégique niveau T12 AIS C, qui marchait avec une attelle releveur à droite, un grand appareil de marche à gauche et deux cannes canadiennes. Il a présenté, après 13 ans d’évolution de la paraplégie, des hydarthroses récidivantes dès la verticalisation ou la tentative de marche en rapport avec une gonarthrose tricompartimentale confirmée par l’arthroscopie et secondaire à une arthrite septique. Ce patient a bénéficié d’une arthroplastie du genou avec un très bon résultat local, fonctionnel et même socioprofessionnel à deux ans et demi de recul.
1
English version
1.1
Introduction
Late-onset complications in spinal cord-injured patients compromise the latter’s quality of life. Over the last 30 years or so, we have witnessed a remarkable and continuous extension of life expectancy for spinal cord-injured patients. As a result (and in addition to the various impairments inherently due to the spinal cord injury itself), these patients are now confronted by degenerative conditions related to age and use, such as arthritis. For patients with only partial spinal cord injuries, neurological damage (motor impairments and spasticity) can increase joint strain and worsen the arthritis in weight-bearing joints, such as the hip and knee. The occurrence of septic arthritis is also an aggravating factor which can result in rapid destruction of the joint; the ultimate therapeutic solution corresponds to total joint replacement, particularly when gait is still possible.
1.2
Observation
At the age of 24, the male patient “SA” (now aged 42) had suffered a workplace accident involving dorsolumbar spine trauma with an L1 compression fracture, complicated by T12 AIS grade A paraplegia. Treatment consisted of T11-L3 osteosynthesis with a bone graft. Postoperative care was fairly straightforward. After rehabilitation, the patient’s condition was characterized by sensorimotor recovery and T12 AIS grade C paraplegia. The patient was able to walk for up to 200 m with two forearm crutches, a knee-ankle-foot orthosis on the left leg and an ankle-foot orthosis on the right leg. For longer distances, the patient used a non-motorized wheel chair. He had good bladder and bowel balance with intermittent self-catheterization and anticholinergic drugs. He was able to resume work as a cashier.
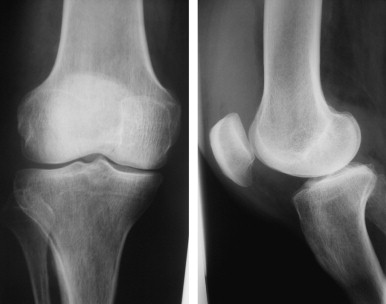
Thirteen years after the injury, the patient was hospitalized for septic arthritis of the right knee, with functional impairment and inability to walk. There were no apparent signs of trauma or other triggering factors. On examination, the patient was not feverish. The right knee was hot and gave a positive patella impact test. Joint movement was possible but painful. There were no symptoms outside the knee region. Laboratory tests did not reveal any inflammatory or infective syndromes (one-hour erythrocyte sedimentation rate: 10 mm; C-reactive protein: 6 mg/l; white blood cell count: 8,100/mm 3 ). Standard radiography of the right knee did not show any anomalies ( Fig. 1 ). Needle biopsy of the knee joint withdrew a fluid with an inflammatory aspect and a white blood cell count of 13,000/mm 3 (80% of which were polynuclear neutrophils). Staphylococcus aureus was isolated from culture of the fluid. The synovial biopsy evidenced acute suppurative synovitis, with no signs of specificity. A diagnosis of septic arthritis was therefore made. A survey of potential causes was negative in the sense that no entry sites was identified (notably urinary and cutaneous sites). Treatment consisted of a 60-day course of appropriate antibiotics, together with joint lavage and weight relief for the right leg. The change over time in the patient’s condition was characterized by the repeated occurrence of knee hydrarthrosis (water on the knee) whenever the patient stood or walked for any length of time; this produced right knee pain and stiffness (with only 15° of flexion). The patient lost his ability to walk (despite good muscle status, Table 1 ) and was ultimately obliged to give up work.
| Muscles | Right leg | Left leg |
|---|---|---|
| Abdominals | 5 | 5 |
| Hip flexors | 3 | 3− |
| Hip extensors | 3− | 3− |
| Gluteus medius | 2 | 2 |
| Hamstrings | 4 | 2 |
| Quadriceps | 4 | 2+ |
| Tibialis anterior | 3 | 0 |
| Triceps surae | 3 | 1 |
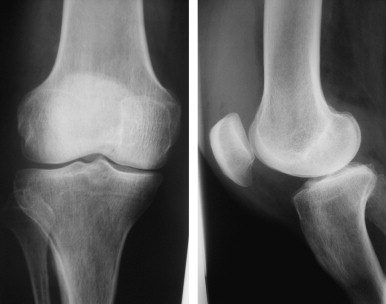
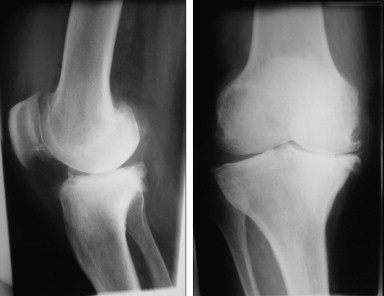
At each relapse of hydrarthrosis, the successive needle biopsies yielded a fluid with a mechanical aspect and a negative microbiological culture test result. Radiographic imaging of the right knee 5 years after the occurrence of the septic arthritis evidenced narrowing of the lower and upper femorotibial and femoropatellar joint spaces, with the presence of large numbers of osteophytes ( Fig. 2 ). Arthroscopy revealed a degenerative internal and external femorotibial chondropathy, rated as stage 5 according to the French Arthroscopy Society’s classification .
A diagnosis of late-stage, three-compartment gonarthrosis was made. The pain intensity was 80 mm on a 100 mm visual analogue scale (VAS). The Functional Independence Measure (FIM) score was 105. The Medical Outcome Scale (MOS) SF 36 quality of life score was 52.7.
Total knee replacement was thus indicated in a patient who:
- (i)
presented T12 AIS grade C paraplegia in the absence of sensory disorders.
- (ii)
was initially able to walk with technical aids.
- (iii)
had lost the ability to walk (and thus lost his job as a result) following repeated, congestive flare-ups of gonarthrosis.
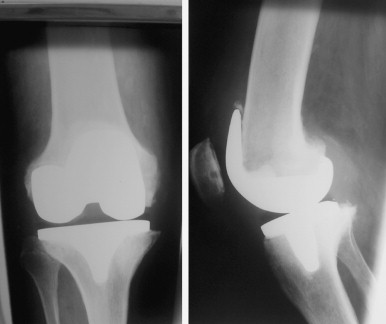
The surgical operation was performed 6 years later. It consisted of knee arthroplasty ( Fig. 3 ) with straightforward postoperative care and a very good mid-term outcome. In fact, the patient had started walking again (with a left-side forearm crutch) and resumed his professional activity 3 months after the operation. Two and a half years after operation, no prosthesis-related complications had occurred and the patient’s radiological and clinical biochemical status was normal. An examination evidenced an improvement in personal independence, quality of life and pain relief. The FIM score had risen from 105 to 117 and the MOS SF 36 score had risen from 52.7 to 75.3. The right knee pain had disappeared, with a VAS score of 0.
1.3
Discussion
Spinal cord-injured patients represent a particular population in view of their multiple impairments, bone/joint fragility and a predisposition to certain conditions (notably hydrarthrosis).
Knee hydrarthrosis can occur during the first few years of paraplegia and it is often linked to (i) microtrauma (potentially complicated by a fracture) occurring during rehabilitation and (ii) heterotopic ossification . The condition can also be observed several years after the onset of paraplegia, as in our patient. Mukand et al. reported 11 cases of knee hydrarthrosis in spinal cord-injured patients monitored over a 2-year period. Six patients presented hydrarthrosis within 6 months of the spinal injury and two developed the condition more than 12 years after the trauma.
The suspected positive clinical diagnosis must critically compared with the laboratory test results, the radiological data and, in the event of doubt, arthroscopy .
It can be difficult to establish the aetiology of the hydrarthrosis – notably when multiple, interlinked pathologies are present, such as septic arthritis; this condition can then destroy the joint and lead to recurrent hydrarthrosis and primary or secondary arthritis aggravated by peri-articular muscle deficits, as observed in our patient. In fact, spinal cord-injured patients are at risk of developing septic arthritis, in view of many concurrent factors: the frequent occurrence of bedsores, malnutrition, and bladder and bowel dysfunction with microbial colonization. The latter problem is aggravated by the use of an indwelling catheter – a bladder drainage method that should be prohibited in all cases.
Other more frequent aetiologies for hydrarthrosis have been reported. In the series published by Mukand et al. , the aetiology was trauma in six cases, pseudogout in two cases, septic arthritis in one case and spasticity in another. Other authors have mentioned the impact of peri-articular muscle paralysis in the genesis of (sometimes recurrent) hydrarthrosis .
The literature data agree on the fact that hydrarthrosis leads to pain and functional impairment, which prevent standing, gait and wheelchair transfer. This functional decline has an impact on socioprofessional integration and thus alters the quality of life for both ambulatory and non-ambulatory spinal cord-injured patients .
Resorting to surgical treatment (and notably joint replacement, in the event of severe damage) can be a useful therapeutic option. It may be indicated not only in ambulatory spinal cord-injured patients (thus maintaining gait and standing capacities) but also in non-ambulatory patients when the functional limitation is significant . However, it must be remembered that an indication of joint replacement in the spinal cord-injured patient is difficult to establish, in view of the osteoporotic background (which favours the development of osteomata) and the major risk of secondary infections via urinary or cutaneous entry sites. This indication must thus be made wisely and must take account of the risk–benefit ratio for the patient, given his/her degree of independence and the extent of the handicap caused by destruction of the knee joint.
In the present case report, our recourse to total knee arthroplasty was guided by (i) the patient’s ability to walk prior to the occurrence of the invalidating hydrarthrosis and (ii) the significant drop in his quality of life and thus exclusion from employment. Furthermore, the risk of infection appeared to be minor, in view of the absence of bed sores and urinary tract infections with use of an intermittent catheter.
This major surgery provided our patient with significant functional gain, a renewed ability to walk with a technical aid and a return to employment 3 months after the operation. Improvements in independence and quality of life were confirmed by increases in the FIM and MOS SF 36 scores.
1.4
Conclusion
Knee hydrarthrosis is frequent in spinal cord-injured patients and can compromise their independence and quality of life.
Total knee arthroplasty can be a useful therapeutic option in spinal cord-injured patients (and above all in those able to walk). The indication must be discussed and decided in consultation with the patient, by specifying the targeted functional objective and by taking account of the major risk of sepsis with this particular background. Clinical and radiological follow-up of the joint replacement is necessary in view of secondary bacterial infection. Rehabilitation is also required (in order to guarantee the requisite muscle performance), although extreme vigilance must be applied for patients with (even minor) proprioceptive disorders.
2
Version française
2.1
Introduction
Les complications tardives chez les blessés médullaires viennent hypothéquer la qualité de vie de ces malades. Depuis une trentaine d’années, on assiste à un allongement continu et remarquable de l’espérance de vie des blessés médullaires. Ainsi, ces patients sont confrontés, outre aux conséquences inhérentes aux différentes déficiences dues à la lésion médullaire, aux processus dégénératifs liés à l’âge et à la sur-utilisation, dont l’arthrose. Dans les atteintes médullaires incomplètes, l’atteinte neurologique (déficit moteur et spasticité) peut augmenter les contraintes articulaires et aggraver l’évolution de l’arthrose en cas d’articulation portante comme la hanche et le genou. La survenue d’une arthrite septique est aussi un facteur aggravant qui peut aboutir à une destruction rapide de l’articulation dont l’ultime recours thérapeutique est représenté par l’arthroplastie particulièrement quand la marche est possible.
2.2
Observation
Monsieur S.A., âgé de 42 ans, était victime à l’âge de 24 ans d’un accident de travail, ayant occasionné un traumatisme du rachis dorsolombaire avec une fracture tassement de L1 compliquée d’une paraplégie niveau T12 AIS A. Le traitement a consisté en une ostéosynthèse T11-L3 avec une greffe osseuse. Les suites opératoires étaient simples. Après une prise en charge rééducative, l’évolution était marquée par une récupération sensitivomotrice avec une paraplégie niveau T12 AIS C. Le patient marchait avec un grand appareil de marche à gauche, une attelle releveur à droite ainsi que deux cannes canadiennes. Le périmètre de marche était de 200 m. Pour les grandes distances, le patient utilisait un fauteuil roulant manuel. Il avait un bon équilibre vésico-sphinctérien sous autosondages intermittents et anticholinergiques. Ainsi, il avait pu reprendre son travail de caissier.
Treize ans après le traumatisme, le patient était réhospitalisé pour une arthrite septique du genou droit avec impotence fonctionnelle et incapacité à marcher. Il n’y avait pas de notion de traumatisme ni d’autres facteurs déclenchants apparents. À l’examen, le patient était apyrétique, le genou droit était rouge, chaud avec un choc rotulien positif. La mobilité articulaire était conservée mais douloureuse. Il n’y avait pas d’autres signes extra-articulaires. Le bilan biologique n’avait pas objectivé de syndrome inflammatoire, ni infectieux avec notamment une vitesse de sédimentation (VS) à 10 mm à la première heure, une C-réactive protéine (CRP) à 6 mg/l et des globules blancs à 8100 E/mm 3 . Les radiographies standard du genou droit étaient sans anomalies ( Fig. 1 ). La ponction articulaire du genou avait ramené un liquide d’allure inflammatoire, trouble avec la cytologie des globules blancs à 13 000 E/mm 3 , dont 80 % étaient des polynucléaires neutrophiles altérés. La culture avait isolé un Staphylococcus aureus . La biopsie synoviale avait objectivé une synovite aiguë suppurée sans signes de spécificité. Le diagnostic d’arthrite septique était alors retenu et l’enquête étiologique était négative à savoir aucune porte d’entrée n’était retrouvée, notamment urinaire ou cutanée. Le traitement avait consisté en une antibiothérapie adaptée durant 60 jours associée à des lavages articulaires et une décharge du membre inférieur droit. L’évolution était marquée par l’installation d’une hydarthrose récidivante survenant à chaque verticalisation ou tentative de marche et responsable de douleurs et d’une raideur du genou droit (flessum de 15°). Le patient avait perdu la marche, malgré un bon capital musculaire ( Tableau 1 ) et avait fini par arrêter son travail.