The gross anatomical features of the thoracolumbar spine are shown in Figures 30-1, 30-2, 30-3, 30-4, 30-5, and 30-6.
See references 1–4.
The three ossification centers of each vertebra (one for the centrum and two for each neural arch) typically fuse between the age 2 and 6 years. Each vertebra assumes adult characteristics by approximately age 8 years and oblique pattern is achieved by age 15 years. The vertebral body physes can be seen on x-ray by 8 years of age when they begin to ossify peripherally and are relatively thicker at the periphery (ring apophysis). Ossification is completed by 12 years of age. The physis begins to fuse with the vertebral body at approximately 14 years of age and the fusion is complete between the age 21 and 25 years. The physis contributes to the growth in height of the vertebral body whereas the ring apophysis contributes to the growth in breadth of the vertebral body.
The basic structure of the immature vertebral body and associated disk is depicted in Figure 30-7. The intervertebral disk is composed of a centrally located nucleus pulposus and peripheral annulus fibrosus, and the adjacent vertebral endplate. The nucleus pulposus in the immature spine is more resilient and elastic because of relatively higher water content compared to the mature spine.
The spinal canal achieves the adult volume by 6 years of age. There is an inherent difference between the spinal column and the spinal cord flexibility in the immature spine. The spinal column can be stretched up to 5 cm before it fails owing to disruption, whereas the spinal cord fails after 1 cm of stretch. This explains the phenomenon of spinal cord injury without radiological abnormality (SCIWORA) seen mostly in young children and predominantly affects the cervical spine. The spinal cord ascends to L1 by age 1 and therefore the neurological levels of spinal cord injury are the same as adult after age 1 year.
Sport-related thoracolumbar injuries can involve soft tissue structures, the bony elements, or the spinal cord. Sport-related acute trauma is rare in young children and uncommon in adolescents. It is estimated that 80% of the injuries occur during practice, and acute injuries account for 60% of these.
Overuse injuries of the back are relatively more common in adolescent athletes. Sport-related injuries account for 10% to 15% of injuries to the spine. Overall, the prevalence of back pain from all causes has been reported to be between 20% and 30% in 11- to 17-year age group.5–12 The incidence of back pain related to sports injuries vary widely depending upon the sport. The most common injuries are the acute soft tissue sprains, strains, and contusions.
Unlike in an acute injury, the cause and effect relationship between the chronic injury and symptoms or spine abnormalities cannot be always clearly established in young athletes. In adolescent athletes the most common underlying identified spine lesion is spondylolysis.
The most common predisposing factor for thoracolumbar back pain in adolescent athletes has been reported to be a recent change in training regimen. Other reported predisposing factors include poor conditioning, relative core muscle weakness, decreased hamstring flexibility, increased lumbar lordosis, improper sport technique, and poor fit or use of equipment. Sports with relatively higher prevalence of back pain are listed in Table 30-1.5–12
Golf |
Running |
Weight lifting |
Racquet sports |
Gymnastics |
Cheerleading |
Dancing |
Diving |
Rowing |
Basketball |
Wrestling |
Rugby |
Ice hockey |
American football |
Fast bowling in cricket |
Sport biomechanics play an important role in the type of stress and injury sustained in sports (Table 30-2). Flexion of the thoracolumbar spine has been shown to increase the pressure on the intervertebral disks, increase the tension on the nerve root and dural sac, and increase the relative size of the intervertebral canal and the foramen. Extension of the spine will have the opposite effects.
Biomechanical Stress | Example of Sport |
|---|---|
Compression of spine in vertical plane | American football, weight lifting |
Rotational (torque) or shear force in horizontal plane | Throwing sports, golf, baseball |
Tensile stress from excessive, repetitive motion | Gymnastics, ballet, cheerleading |
Direct blows to the back can cause muscle contusions. Hyperextension of lumbar spine, as seen in football and gymnastics, is implicated in the development of spondylolysis. In gymnasts, a higher level of competition is correlated with a higher incidence of back problems. Studies suggest that floor exercises, the balance beam, uneven parallel bars, flips, and vaulting dismounts contribute to back injuries in gymnasts. In throwing sports, musculotendinous avulsions may occur from forceful sudden muscle contractions. In the adolescent athlete, the immature vertebral end plates may be injured from improper weight lifting. Lifting with spine in flexion, and moving from flexion to extension causes significant stress to the spine. Improper lifting techniques may cause injuries in ballet and figure skating. Twisting motions in tennis can cause musculotendinous strains and avulsions. Chronic poor posture may result in chronic ligamentous strain.
History should include the mechanism of injury and detailed history characterizing the pain. Pain should be characterized by onset, location, duration, progression, exacerbating factors and relieving factors. Is there night pain? Is there radiation of pain in legs? Ascertain past history of back pain or injury. Has the athlete sought any previous medical care?
Athlete will present with a history of back pain following acute trauma or activity-related chronic or recurrent pain. Back pain in a young child must be thoroughly investigated for specific etiology that may include infection, tumors, or developmental anomalies of the spine. Localization of pain may indicate possible etiology. Scheuermann disease is the most common identifiable cause of thoracic back pain. Spondylolysis most commonly affects the lower lumbar spine. Constitutional symptoms such a fever, rash, other joint pain, loss of appetite, and weight loss suggest systemic disease. Family history and psychosocial history are essential in all adolescents to assess psychosomatic pain syndrome which is common in this age group. Although neurological injuries are rare, it is important to recognize symptoms and signs that indicate neurological injury that should prompt appropriate imaging and referral for definitive diagnosis and treatment.
General physical examination should focus on detecting signs that indicate systemic etiology. Sexual maturity rating or Tanner stage (see Figures 2-2, 2-3, and 2-4, Chapter 2) should be assessed and both lower extremities should be carefully examined. A systematic examination of the back and thoracolumbar spine as well as neurological examination should be conducted in all athletes with back injuries and pain.
See references 13–16.
- Gait: Observe for pain during full weight bearing or any protective posture. Also judge the degree of pain or discomfort.
- Observe the overall standing posture from behind and from side. Note any asymmetry. Note the normal thoracic (convex) and lumbar (lordotic) curves. Note listing. Note tendency to stand or walk with flexed hips and knees (crouching).
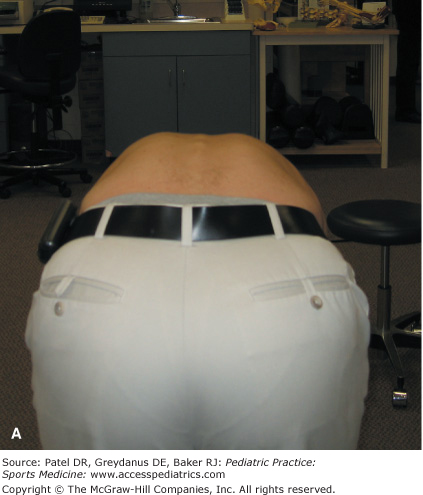
- Have the athlete bend over (flexion) and observe the spine from front, behind, and side of the athlete. Note scoliosis (Adam test) or kyphosis (Figure 30-8).
- Observe from the front the symmetry of hips and alignment of iliac crests.
- Assess active range of motion of the spine (Table 30-3). Schober test (Figure 30-9) is helpful to measure the degree of flexion of the thoracolumbar spine. To measure the lateral flexion first mark the point on the lateral aspect of the thigh where the tip of middle finger reaches; followed by marking the point on lateral flexion. The distance between the two points is useful to assess the amount of lateral flexion.
- One-legged hyperextension test (Figure 30-10)
- Trendelenburg test (Figure 30-11)
- Assess the strength of the calf muscle by observing the ability of the athlete to do repeat unilateral heel raises (S1). Manual testing of plantar flexion is not reliable. Assess the strength of the anterior tibialis muscle (ankle dorsiflexion) by having the athlete do heel walking (L5).
- Palpate and localize soft tissue and bony tenderness over the back, spine, and hips.
Figure 30-9
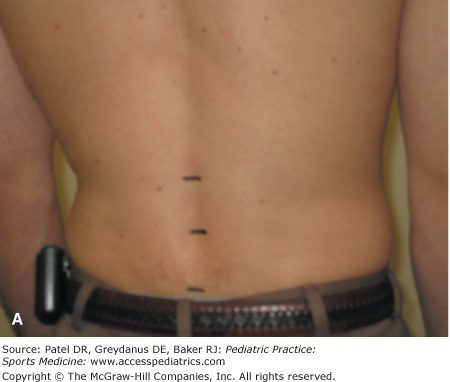
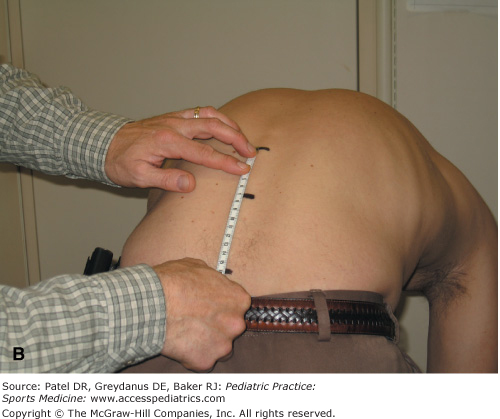
Schober test. With the athlete standing, mark a point on the spine midway between the posterior superior iliac spines, second point 5 cm above and third point 10 cm below (A). Measure the distance between the most superior and the most inferior points. Ask the athlete to bend forward and measure the distance between the same points again (B). The degree of flexion of the lumbar spine is indicated by the difference between the measurements.
Figure 30-10

One-legged hyperextension (Stork test). With the athlete standing on one leg have her extend the back. Repeat the same on the opposite leg. Pain is elicited on extension in case of pars interarticularis stress fracture of a lumbar vertebra. Pain is relatively more intense on the ipsilateral side.
Figure 30-11



Trendelenburg test. Have the athlete stand on one leg (A). Observe from behind. Normally the pelvis remains level or horizontal mainly because of the contraction of the gluteus medius of the leg that is weight bearing (B). Sagging of the hip of the leg lifted off the ground is suggestive of gluteus medius weakness of the weight-bearing leg (C).
- Observe the athlete for any apparent discomfort as he or she moves from standing to sitting on the exam table. Observe the sitting posture from back, side, and front. Note asymmetry of shoulders or hips. Note the alignment of iliac crests.
- Tripod test (Figure 30-12)
- Slump test (Figure 30-13)
Figure 30-12

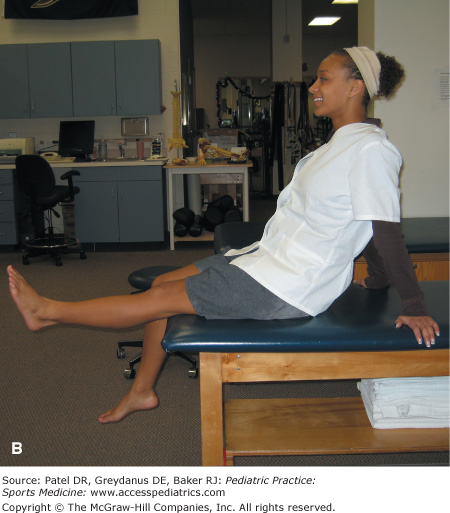
Tripod test. The athlete is seated on the examination table with both hips and knees at approximately 90-degree flexion and straight back. The knee is then extended (A). If the hamstring on that side is tight or if the nerve roots are irritated, the athlete will extend her back to relieve the tension in hamstrings or on the sciatic nerve (B). Repeat on the other side.
Figure 30-13

Slump test. The athlete is seated on the examination table. She is asked to slump with flexion of spine and allowing the shoulders to sag forward. Sequentially, the examiner flexes the neck, followed by passive extension of the knee, and passive dorsiflexion of the foot. Sciatica type pain in the leg is considered positive test suggesting impingement of the dura or spinal cord or nerve root.
- Note the level of anterior superior iliac spines
- Measure for both legs (a) the leg length from the anterior superior iliac spine to lateral malleolus; (b) girth at midthigh; and (c) girth at midcalf.
- Assess quadriceps and hamstring flexibility (Figure 30-14)
- Assess strength (Table 30-4), sensation to pin prick (Table 30-5) and reflexes (Table 30-6) in both lower limbs
- Straight leg raise (Lasegue) test: Contralateral leg pain is characteristic of a disk herniation whereas, ipsilateral pain is characteristic of sciatica.
- Hoover sign (Figure 30-15)
- Patrick or FABER test (Figure 30-16)
- Gaenslin test (Figure 30-17)
Figure 30-14
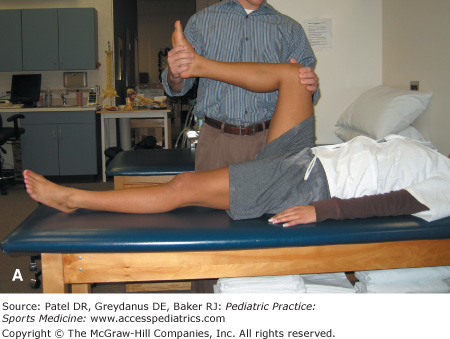
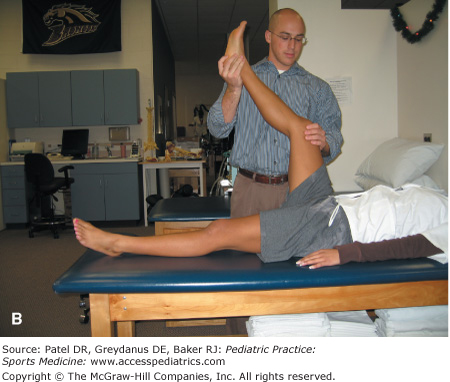
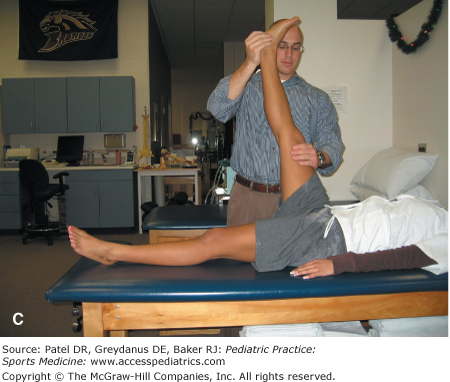
Testing hamstring flexibility. With the athlete supine on the examination table, first fully flex the hip and knee (A), then bring the hip to 90 degree flexed position (B), and extend the knee as far as possible (C). With good flexibility of hamstrings, the knee can be extended to 180 degrees. The degree of lack of extension (popliteal angle) of the knee is a measure of hamstring tightness. Examine each leg separately.
Muscle Group | Neurological Level |
|---|---|
Abdominals | T7–T12 |
Hip flexors | L1–L2 |
Knee extensors | L3 |
Knee flexors | S2 |
Ankle dorsiflexors | L4 |
Ankle plantarflexors and evertors | S1 |
Hip extensors | |
Great toe extensor | L5 |
Figure 30-15


Hoover test. With the athlete supine on the examination table ask her to raise her fully extended leg while cupping the heel of the opposite foot. Normally, a downward pressure is appreciated in the opposite leg, while the athlete attempts to raise the other leg. If no such downward pressure or bearing down is felt it is suggested that the athlete is not trying to raise the opposite leg, as in malingering.
Figure 30-16

Patrick or FABER test. With the athlete supine the leg is placed in a figure of 4 position (flexion, abduction, external rotation of the hip). Then it is lowered with gentle downward pressure over the knee while holding down the opposite hip. Positive test is indicated by pain or discomfort in the sacroiliac area iliopsoas or sacroiliac pathology.
Figure 30-17

Gaenslin test. The athlete lies supine on the examination table. Ask her to fully flex both legs, followed by having her move to the edge of the table and slowly extend the hip and lower the leg over the edge of the table. Repeat on the opposite leg. Pain in the sacroiliac joint area while extending the hip and lowering the leg is suggestive of sacroiliac pathology.
- Observe for thoracic kyphosis: Apparent kyphosis owing to postural round back disappears when the athlete extends the back while prone whereas a fixed deformity will persist.
- Femoral nerve stretch test (Figure 30-18)
Back pain in young children with certain “red flag” signs (Table 30-7) warrants a thorough evaluation. In addition to apparent acute or repetitive trauma, a number of other intrinsic (Table 30-8) and extrinsic (Table 30-9) conditions should be considered in the differential diagnosis of back pain in adolescents.1,2,5–9,11,17,18
Back pain in a child younger than 10 y |
Pain that wakes the patient up from sleep |
Pain lasting 2 or more months |
Severe progressive pain |
Continuous or constant pain |
Pain at rest |
Associated neurological signs |
Associated systemic symptoms and signs |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree