This article describes the evidence for the physiologic foundation and interpretation of the videofluorographic swallowing study (VFSS). The purpose and clinical efficacy of VFSS are explained. Standardization of the VFSS procedure, protocol, interpretation, and reporting is highlighted as a critical step in future clinical practice and research. Individualized evidenced-based rehabilitation strategies are presented as key components that are systematically applied during the VFSS procedure and integrated into the swallowing management plan. A new tool that has been developed and tested for the quantification of swallowing impairment is introduced.
The literature is dense with measurement methods used to estimate the presence and degree of oropharyngeal and esophageal swallowing dysfunction. These methods are directed toward gaining objective indexes of the timing , pressure , range , and strength of structural movements, bolus flow patterns , bolus clearance and efficiency , airway protection , and sensation . These studies have established a strong theoretic framework toward understanding the nature of swallowing abnormalities. Multiple assessment methods are in existence and development. Although the current health care climate demands fiscal responsibility, clinicians must choose the test that is appropriate for each patient and delivers the highest diagnostic and prognostic clinical yield. Furthermore, the test and the measurement methods used to capture oropharyngeal swallowing impairment must be practical for routine clinical application.
The videofluorographic swallowing study (VFSS), also known as a modified barium swallowing (MBS) examination, is often considered the preferred instrument by most practicing swallowing clinicians because it allows visualization of bolus flow in relation to structural movement throughout the upper aerodigestive tract in real time. The VFSS also permits detection of the presence and timing of aspiration (ie, entry of ingested material through the level of the true vocal folds into the trachea) and helps identify the physiologic and often treatable causes of the aspiration . Furthermore, clinicians are able to observe the effects of various bolus volumes, bolus textures, and compensatory strategies on swallowing physiology .
Clinicians evaluating and treating swallowing disorders use a videofluoroscopic radiology procedure to assess swallowing physiology in patients who have symptoms of swallowing disorders (ie, dysphagia) and to estimate the degree of swallowing impairment from observations made during the examination. The examination usually includes the collaborative expertise of a physician, most commonly a radiologist or physiatrist, and speech–language pathologist.
This MBS examination captures sequential videoradiographic images of barium contrast–impregnated food and liquid as they are transported through the oral cavity, pharyngeal cavity, and esophagus in real time. Various volumes and textures of food and liquid are administered and clinical impressions of the presence and degree of swallowing impairment are obtained from the radiographic images . Judgments are also made regarding the coordination and timing of swallowing events . Based on these qualitative observations, critical and sometimes life-sustaining recommendations are made regarding oral versus nonoral intake, diet type, referrals to other medical specialties, and treatment strategies that improve function or minimize the risk for aspiration .
Despite the clinical efficacy of the examination, clinicians must acknowledge that the patient’s performance during the examination may not be entirely representative of the patient’s typical eating and drinking function. Variables such as fatigue, medications, and anxiety may impact the testing results. Clinicians must observe patients during their usual eating and drinking environment to determine the external validity of the examination results and assess the patient’s ability to carry-over any learned swallowing strategies. Furthermore, the VFSS is also used to monitor any changes in swallowing function over time during the course of swallowing treatment and the progression of a disease or condition.
Videofluorographic swallowing study: an indirect sensory and motor examination
Swallowing is an array of synergistic interdependent movements, initiated by a complex set of sensory inputs that generate motor responses. These motor responses create pressures and forces to propel ingested materials through the upper aerodigestive tract and simultaneously protect the upper airway. Although the VFSS does not use direct measures of sensation and muscle strength, the following evidence suggests that trained examiners can make accurate and reliable clinical judgments about the presence of sensory and motor impairment.
The following description of VFSS observations are characterized as physiologic components. Most observed components contribute to judgments of sensory and motor impairment because the initiation and integrity of the motor response partly depends on sensory input.
A prime example of this combined sensorimotor assessment is observation of the motor events that occur early in the pharyngeal swallow. If these events are delayed for several seconds, the sensory input to the pharyngeal motor response is probably decreased below the normal level required to initiate the cascade of pharyngeal motor events. Clinicians evaluate the sensorimotor relationships during the VFSS and administer various bolus consistencies, textures, and sometimes taste to assess their effect on swallowing function.
Swallowing physiology: foundation for videofluorographic swallowing study
Swallowing is a complex physiologic event comprised of simultaneous and sequential contractions of muscles of the oral–facial region, pharynx, larynx, and esophagus. Descriptions of swallowing physiology were attempted well before the development of a sophisticated modality for viewing the rapid contractions and movements of the muscles and structures associated with swallowing. In 1813, Magendie was the first to separate swallowing into phases or stages representing the anatomic regions traversed by the bolus , or ball of material, to be swallowed. The rapid sequential and overlapping motions characterizing adult human swallowing behavior were better appreciated after radiography was introduced, especially videoradiography.
Although phase descriptions remain in current literature, evidence suggests that the physiologic components of the process overlap and are interdependent as the bolus traverses the regional phases (oral, pharyngeal, esophageal), which has led clinicians to attempt to assess the physiology of the swallowing rather than report abnormality of a given phase. Furthermore, the physiology is the target of swallowing rehabilitation, and therefore these targets must be identified before the treatment plan is developed. Swallowing clinicians attempt to evaluate components of swallowing behavior on VFSS examinations in patients presenting with clinical signs or symptoms of dysphagia ( Box 1 ).
- 1.
Lip closure
- 2.
Lingual elevation
- 3.
Tongue-to-palatal seal
- 4.
Bolus preparation/mastication
- 5.
Bolus transport/lingual motion
- 6.
Initiation of pharyngeal swallow
- 7.
Soft palate elevation and retraction
- 8.
Laryngeal elevation
- 9.
Anterior hyoid excursion
- 10.
Laryngeal closure
- 11.
Pharyngeal contraction
- 12.
Pharyngoesophageal segment opening
- 13.
Tongue base retraction
- 14.
Epiglottic inversion
- 15.
Esophageal clearance
Clinicians also use the 15 literature-based components to estimate the severity of the impairments and make critical intake and diet texture recommendations, swallowing therapy recommendations, and predictions about functional outcomes .
Although the late oral and early pharyngeal components of swallowing are the most critical from a safety viewpoint, the oral preparatory and early oral transport aspects of swallow are the most aesthetically and psychologically important. During the oral preparatory stage of swallow, the bolus is manipulated by lingual motion and masticated (if necessary). Although not a characteristic of natural drinking or eating behavior in most healthy individuals , the ability to contain a liquid bolus (component 1, Fig. 1 A ) in the oral cavity through an anterior lip seal and lateral and posterior tongue-to-palatal contact ( Fig. 1 B) is assessed. The proficiency of this task provides clinical information about a patient’s ability to follow simple commands during swallowing, which is an important prognostic indicator for successful learning of compensatory swallowing strategies.
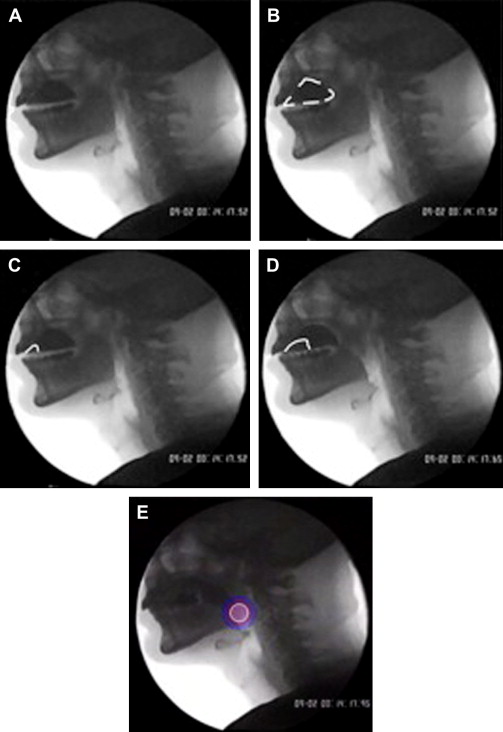
Furthermore, the ability to contain a bolus within the oral cavity provides information on oral motor control. The tongue is the major mobile element of the oral swallow and plays a complementary role in bolus preparation and mastication. The tongue also plays a major role in bolus containment and airway maintenance . The back of the tongue assumes a slightly elevated position from contraction of various muscle groups, and opposes an actively contracted soft palate that is drawn downward and forward (component 2, see Fig. 1 B). This glossopalatine mechanism (component 3, see Fig. 1 B) ensures that portions of a liquid bolus do not fall prematurely over the base of the tongue . The ingested material is mixed with saliva and tasted during rotary mandibular chewing (component 4), a motion that is integrated into the oral swallowing process and propelled through the oral cavity by way of lingual motility (component 5, Fig. 1 C, D) .
When adult humans eat natural bite sizes of solid foods, portions of the food may be propelled to and accumulate in the pharynx during mastication . If the system has inefficiencies, such as muscle weakness or sensory loss, residual material may remain in the oral or pharyngeal cavity, placing the patient at risk for inadequate nutrition/hydration or airway compromise.
As the bolus is propelled through the oral cavity through upward and forward motion of the tongue, the head of the bolus reaches the region of the posterior oral cavity or oropharynx. When the sensory receptive fields in these areas are stimulated, the pharyngeal swallow is initiated (component 6, Fig. 1 E) and the respiratory pause to accommodate swallowing becomes obligatory .
Although onset of the pharyngeal swallow varies relative to the position of the bolus , when initiated it is characterized by five mechanical events that have been shown to overlap during synchronized videorecordings of structural movements during swallow. These events protect the airway and clear the pharynx of ingested material, and include (1) elevation and retraction of the soft palate (component 7, Fig. 2 A ); (2) elevation and anterior displacement of the larynx (component 8, Fig. 2 B) and hyoid bone ( Fig. 2 C); (3) laryngeal closure (component 10, Fig. 2 D); (4) pharyngeal contraction (component 11); and (5) opening of the pharyngoesophageal region (component 12, Fig. 2 E) . Contraction of the pharyngeal constrictors ( Fig. 2 F) coincides with the forceful retraction of the tongue (component 13, Fig. 2 G), which applies strong positive pressure on the bolus tail, assisting in pharyngeal clearance and prevention of pharyngeal residue . The hyoid bone and larynx move as a functional unit in a superior and anterior trajectory during a normal, nutritive swallow.
These critical motions, observed during VFSS, are physiologically linked to effect vestibular closure (ie, through approximation of the arytenoid cartilages and the epiglottic petiole together with full inversion of the epiglottic tip) (component 14, see Fig. 2 F; Fig. 2 H) and to opening and distension of the pharyngoesophageal segment (PES) (see Fig. 2 E). Opening of the segment permits entry of the ingested material into the cervical esophageal region . The traction placed on the cricoid cartilage during this brisk motion pulls the cartilage anteriorly and away from the posterior pharyngeal wall, opening the compliant PES region (see Fig. 2 E) . This compliance is related to early relaxation of the cricopharyngeal muscle, the primary muscular component of the segment . As the larynx descends toward its rest position in the latter stages of pharyngeal swallowing, respiration is resumed and characterized by a small expiratory airflow in most adult human swallows .
The mechanics of the esophageal body and lower esophageal sphincter are less complex and easier to study because of their slow speed relative to oropharyngeal swallow events. The bolus head enters the cervical esophageal region through the distended PES, continues through the esophagus, and is propelled and cleared (component 15, Fig. 3 ) through primary and secondary esophageal peristaltic muscle contractions . These contractions continue until the bolus head and tail progress through the passively relaxed lower esophageal sphincter (LES) and advance into the stomach.
A few behavioral interventions are available to modify the contractile characteristics of the esophagus and improve esophageal clearance . However, clinical evidence and preliminary research indicate that esophageal clearance in the upright position seems to have some functional impact on pharyngeal clearance and possible airway protection . Therefore, clinicians observe esophageal clearance in the upright eating and drinking position during the MBS examination to gain an impression of the potential impact of incomplete or slowed esophageal clearance on oropharyngeal swallowing function; the potential for aspiration of residual esophageal contents; and the nutritional status of the patient.
The anteroposterior image projection is the optimal view for assessing the efficiency of esophageal clearance in the upright position. This viewing plane is also best suited to determine the overall symmetry of oropharyngeal swallowing function and the immediate effectiveness of compensatory postures.
Swallowing physiology: foundation for videofluorographic swallowing study
Swallowing is a complex physiologic event comprised of simultaneous and sequential contractions of muscles of the oral–facial region, pharynx, larynx, and esophagus. Descriptions of swallowing physiology were attempted well before the development of a sophisticated modality for viewing the rapid contractions and movements of the muscles and structures associated with swallowing. In 1813, Magendie was the first to separate swallowing into phases or stages representing the anatomic regions traversed by the bolus , or ball of material, to be swallowed. The rapid sequential and overlapping motions characterizing adult human swallowing behavior were better appreciated after radiography was introduced, especially videoradiography.
Although phase descriptions remain in current literature, evidence suggests that the physiologic components of the process overlap and are interdependent as the bolus traverses the regional phases (oral, pharyngeal, esophageal), which has led clinicians to attempt to assess the physiology of the swallowing rather than report abnormality of a given phase. Furthermore, the physiology is the target of swallowing rehabilitation, and therefore these targets must be identified before the treatment plan is developed. Swallowing clinicians attempt to evaluate components of swallowing behavior on VFSS examinations in patients presenting with clinical signs or symptoms of dysphagia ( Box 1 ).
- 1.
Lip closure
- 2.
Lingual elevation
- 3.
Tongue-to-palatal seal
- 4.
Bolus preparation/mastication
- 5.
Bolus transport/lingual motion
- 6.
Initiation of pharyngeal swallow
- 7.
Soft palate elevation and retraction
- 8.
Laryngeal elevation
- 9.
Anterior hyoid excursion
- 10.
Laryngeal closure
- 11.
Pharyngeal contraction
- 12.
Pharyngoesophageal segment opening
- 13.
Tongue base retraction
- 14.
Epiglottic inversion
- 15.
Esophageal clearance
Clinicians also use the 15 literature-based components to estimate the severity of the impairments and make critical intake and diet texture recommendations, swallowing therapy recommendations, and predictions about functional outcomes .
Although the late oral and early pharyngeal components of swallowing are the most critical from a safety viewpoint, the oral preparatory and early oral transport aspects of swallow are the most aesthetically and psychologically important. During the oral preparatory stage of swallow, the bolus is manipulated by lingual motion and masticated (if necessary). Although not a characteristic of natural drinking or eating behavior in most healthy individuals , the ability to contain a liquid bolus (component 1, Fig. 1 A ) in the oral cavity through an anterior lip seal and lateral and posterior tongue-to-palatal contact ( Fig. 1 B) is assessed. The proficiency of this task provides clinical information about a patient’s ability to follow simple commands during swallowing, which is an important prognostic indicator for successful learning of compensatory swallowing strategies.
Furthermore, the ability to contain a bolus within the oral cavity provides information on oral motor control. The tongue is the major mobile element of the oral swallow and plays a complementary role in bolus preparation and mastication. The tongue also plays a major role in bolus containment and airway maintenance . The back of the tongue assumes a slightly elevated position from contraction of various muscle groups, and opposes an actively contracted soft palate that is drawn downward and forward (component 2, see Fig. 1 B). This glossopalatine mechanism (component 3, see Fig. 1 B) ensures that portions of a liquid bolus do not fall prematurely over the base of the tongue . The ingested material is mixed with saliva and tasted during rotary mandibular chewing (component 4), a motion that is integrated into the oral swallowing process and propelled through the oral cavity by way of lingual motility (component 5, Fig. 1 C, D) .
When adult humans eat natural bite sizes of solid foods, portions of the food may be propelled to and accumulate in the pharynx during mastication . If the system has inefficiencies, such as muscle weakness or sensory loss, residual material may remain in the oral or pharyngeal cavity, placing the patient at risk for inadequate nutrition/hydration or airway compromise.
As the bolus is propelled through the oral cavity through upward and forward motion of the tongue, the head of the bolus reaches the region of the posterior oral cavity or oropharynx. When the sensory receptive fields in these areas are stimulated, the pharyngeal swallow is initiated (component 6, Fig. 1 E) and the respiratory pause to accommodate swallowing becomes obligatory .
Although onset of the pharyngeal swallow varies relative to the position of the bolus , when initiated it is characterized by five mechanical events that have been shown to overlap during synchronized videorecordings of structural movements during swallow. These events protect the airway and clear the pharynx of ingested material, and include (1) elevation and retraction of the soft palate (component 7, Fig. 2 A ); (2) elevation and anterior displacement of the larynx (component 8, Fig. 2 B) and hyoid bone ( Fig. 2 C); (3) laryngeal closure (component 10, Fig. 2 D); (4) pharyngeal contraction (component 11); and (5) opening of the pharyngoesophageal region (component 12, Fig. 2 E) . Contraction of the pharyngeal constrictors ( Fig. 2 F) coincides with the forceful retraction of the tongue (component 13, Fig. 2 G), which applies strong positive pressure on the bolus tail, assisting in pharyngeal clearance and prevention of pharyngeal residue . The hyoid bone and larynx move as a functional unit in a superior and anterior trajectory during a normal, nutritive swallow.







