The Treatment of Distal Tibia Peri-articular Fractures with Circular Ring Fixators
James J. Hutson Jr.
Indications/Contraindications
Circular tensioned-wire fixators are dynamic devices that provide the surgeon with the ability to fabricate a customized external fixator to treat complex, distal tibia, peri-articular fractures. The fixators are constructed based on the position and quality of the fracture fragments and the severity of injury to the soft tissues. Basic principles are applied in sequence resulting in alignment and fixation of the fractures.
Type B fractures have an intact column of bone maintaining length and are ideal for buttress plating with low profile plates and fibula fixation. Type A and C fractures with moderate soft-tissue injury are treated with internal fixation or half-pin bridging frames with limited internal fixation. As soft-tissue damage and bone comminution worsen, the indication to use circular tensioned wires to treat these complex injuries increases (1). Extension of the fracture pattern proximally to the midshaft compromises the ability to use limited plating, but the stiffness of circular fixators allows fixation using the entire shaft of the tibia with fixation pins and wires to treat these extensile fractures. Pilon fractures combined with complex foot injuries are an indication for circular tensioned-wire fixation.
Patients with ischemic vascular disease or diabetes who would have difficulty healing wounds over plates and screws or who are not candidates for local and free flaps are well treated with tensioned-wire fixation. Open wounds can be treated with local wound-healing methods, resulting in closure by secondary intention, or delayed split-thickness skin grafting. The local wound-healing modalities include hyperbaric oxygen treatment, saline wet-to-dry dressing changes, and vacuum sponge dressings. A relative indication is the need for early ambulation. Patients treated with circular fixators can apply partial weight early after fixation, whereas limited low-profile plating must be protected for 3 or more months. The patient with multiple extremity fractures or morbid obesity will be able to use his or her externally stabilized pilon fracture for transfer assistance or partial weight gait, reducing their dependency on a wheel-chair.
Preoperative Evaluation and Planning
Distal tibia peri-articular fractures often occur in patients with multiple trauma. The patient is evaluated for life-threatening injuries. Once stable, the extremity is evaluated, and the dorsalis pedis and posterior tibial pulse are palpated. If undetectable, a Doppler evaluation is conducted. The lower leg and foot is evaluated for compartment syndrome. The extremity is stabilized and a careful physical examination is performed. A detailed neurologic exam with specific testing of deep and superficial peroneal, medial, lateral and calcaneal plantar, saphenous, and sural nerve function is recorded. Open wounds are observed for size and location. Intravenous cephalosporin antibiotics are started immediately in patients with open fractures. With sterile gloves, the wound may be lavaged with normal saline and a sterile dressing applied. Exploration of the wound in the emergency room should be avoided. The lower extremity is splinted with a bulky dressing and plaster splints.
Full length films of the tibia and fibula, as well as anteroposterior (AP), lateral, and mortise views of the ankle should be obtained.
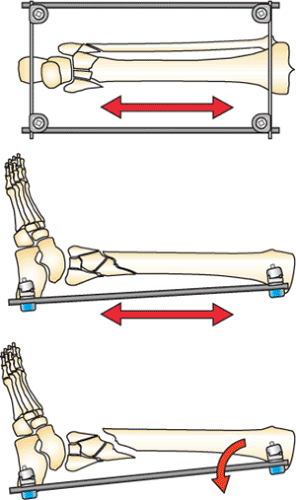
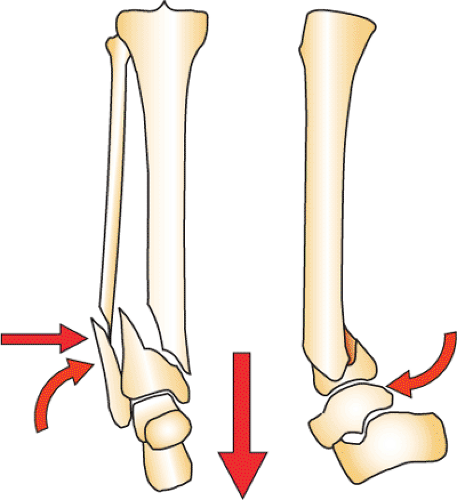
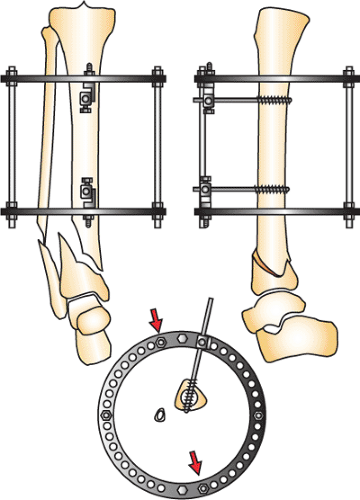
Lower-energy fractures are maintained in the splint. Open fractures and fractures with compartment syndrome require emergent operative intervention. Following debridement and compartment release, the fracture is temporarily stabilized with bridging half-pin fixation and a transverse calcaneal pin (Fig. 32.1). Closed fractures with comminution and displacement also are stabilized with bridging half-pin fixation. If these comminuted fractures are not stabilized and reduced, massive edema and fracture blisters will occur. Calcaneal traction on a Bohler-Braun frame, or traveling traction, is an alternative if the patient cannot be taken to surgery (Fig. 32.2).
The goal of initial bridging fixation is to bring the fracture out to anatomic length and to align the dome of the talus with the central axis of the tibial shaft on the AP and lateral view. The second toe of the foot must be aligned with tibial tubercle at the knee for the surgeon to align correctly the rotation of the extremity. The forefoot is controlled with a first metatarsal pin and the foot is aligned in plantar neutral position. It is essential that excellent alignment be established with this initial trauma resuscitation frame. Failure to achieve these goals will compromise subsequent reconstruction. Repeat debridement and antibiotic bead pouches are indicated for severe open fractures with gross contamination.
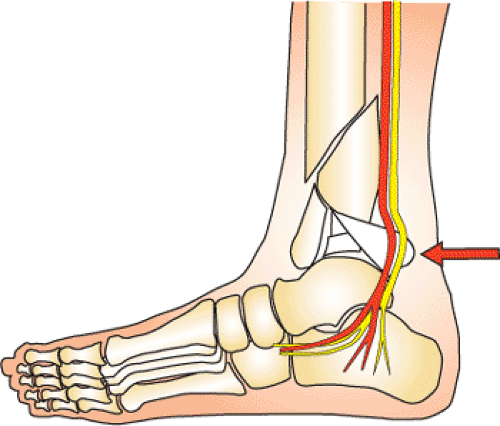
Serial examination of the extremity during the first week is critical. A small number of patients will have further soft-tissue compromise requiring a return to the operating room for further debridement. A small subset of patients will have a fragment of the posterior plafond rotated and displaced against the tibial nerve (Fig. 32.3). These patients have paresthesia or anesthesia of the plantar surface of their foot. Reduction of this fragment is indicated urgently, even if the soft-tissue envelope is not in ideal condition. In a small subset of patients with grade IIIB or grade IIIC fractures, early amputation may be indicated (2).
The majority of closed and simple open fractures will show improvement in the soft-tissue envelope during the first 7 to 14 days. The skin condition determines the timing of the reconstruction of the pilon fracture. When the edema has resolved and the fracture blisters healed, definitive fixation of the pilon fracture can be performed.
The plain films and computed tomography (CT) scan are carefully evaluated. The fibula fracture is observed for level of fracture, comminution, and separation of the fibula from the tibia. The proximal extension of the tibia fracture and comminution of the plafond is evaluated. The CT scan helps the surgeon plan the location of incisions when an open approach is needed. Pilon fractures can be approached through the anterior medial, anterior lateral, or posterior medial exposures. The condition of the soft tissues will be compared to the fracture pattern to avoid dissection through soft tissues with extensive damage. At this time, the decision will be made about the treatment approach: (a) open reduction and internal fixation (ORIF), (b) bridging fixation with limited internal fixation, or (c) circular tensioned-wire fixation. The following sections will describe the treatment strategies for tensioned wire fixation.
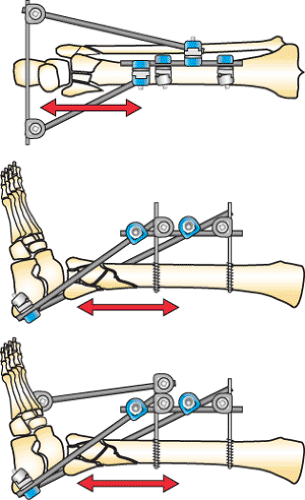
The technical goals of treatment are to align the fracture axially with correct rotation, reduce the joint surface to match the contour of the dome of the talus, reconstruct the mortise, and reconstruct metaphyseal bone loss and comminution. These goals are approached with cautious handling of the soft tissues. Distraction is the key to reduction. Because of the terminal location of pilon fractures, the mid tibial shaft is used as a fixation base to reduce the fracture. When circular fixators are used, a fixation block is applied with two half
pins in the AP plane in an orthogonal position. This fixation block is used as a base to support the distal fixation rings, which are placed at the level of the plafond or calcaneus to distract the fracture. If the plafond or calcaneus (hind foot) is distracted axially with correct rotation, the distal tibia fracture will be spatially reduced with correct rotation, alignment, and length. This initial reduction will facilitate the local alignment of the joint surface and the metaphysis by percutaneous or open techniques. The better the alignment gained by accurate distraction, the easier the reduction of the joint and metaphysis. It is almost impossible in complex pilon fractures to reduce the plafond if the dome of the talus is mal-aligned, shortened, and rotated. This fact pertains to any type of external fixator used to treat pilon fractures (monolateral, clamp and rods, and circular tensioned fixators). The dome of the talus must be aligned correctly in distraction before beginning the reduction of the fracture fragments.
pins in the AP plane in an orthogonal position. This fixation block is used as a base to support the distal fixation rings, which are placed at the level of the plafond or calcaneus to distract the fracture. If the plafond or calcaneus (hind foot) is distracted axially with correct rotation, the distal tibia fracture will be spatially reduced with correct rotation, alignment, and length. This initial reduction will facilitate the local alignment of the joint surface and the metaphysis by percutaneous or open techniques. The better the alignment gained by accurate distraction, the easier the reduction of the joint and metaphysis. It is almost impossible in complex pilon fractures to reduce the plafond if the dome of the talus is mal-aligned, shortened, and rotated. This fact pertains to any type of external fixator used to treat pilon fractures (monolateral, clamp and rods, and circular tensioned fixators). The dome of the talus must be aligned correctly in distraction before beginning the reduction of the fracture fragments.
Reduction Technique for Type A, C1, and C2 Fractures
The level of the horizontal reference-wire placement is determined by the fracture pattern being treated. In type A distal tibia fractures, the joint surface is intact. In C1 and C2 fracture patterns of the joint, there is a simple fracture plane with two large fragments. A limited open reduction and fixation with subchondral lag screws will reduce the joint surface anatomically creating a unified bone block. This reconstructed metaphysis can be treated as a type A fracture (Fig. 32.4).
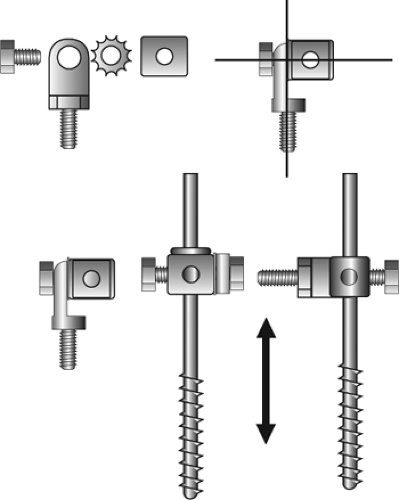
The proximal ring block is aligned on the tibial shaft with two anterior posterior 5- or 6-mm half pins. The half pins should be spread apart 10 cm or more to increase stiffness of the fixator. Mounting these pins with universal fixation cubes facilitates alignment of the frame. The distal half pin is placed 3 cm above the proximal extent of the fracture. Placing the half pins far superior to the fracture increases the working length and thus leads to frame instability. It is important to align the fixation block in an orthogonal position. The frame should be parallel to the tibia on the AP and lateral views, and the tibia should be placed
into the rings to provide clearance for the soft tissues. The ring over the plafond must clear the anterior soft tissues of the ankle, and the superior ring of the fixator block must not impinge on the posterior leg where the gastrocnemius and soleus muscles bulge posteriorly. See Figures 32.5 and 32.6.
into the rings to provide clearance for the soft tissues. The ring over the plafond must clear the anterior soft tissues of the ankle, and the superior ring of the fixator block must not impinge on the posterior leg where the gastrocnemius and soleus muscles bulge posteriorly. See Figures 32.5 and 32.6.
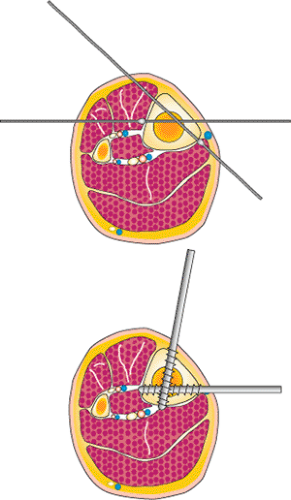
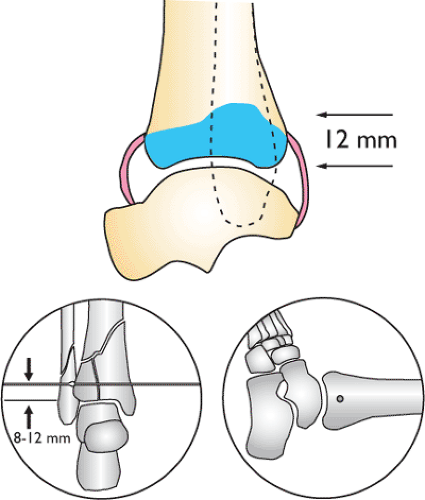
If the fixation block on the tibia is orthogonal, then the joint surface of the plafond will be in anatomic alignment when the joint forms a 90-degree angle with the axis of the shaft and orthogonal, ring, stable base. The plafond on the AP view forms an angle of 90 degrees to the axis of the tibia. This anatomic fact allows the surgeon to align distal tibia fractures accurately by placing a horizontal reference wire parallel to the joint surface. The plane of the carbon-fiber fracture-reduction ring, which is connected to the orthogonal stable base, is 90 degrees to the shaft. The horizontal reference wire in the plafond is placed onto the distal surface of the carbon-fiber fracture ring and manipulated with fluoroscopic guidance so that the plafond aligns axially and with correct rotation. The horizontal reference wire may need to be loosened and repositioned several times until excellent alignment is obtained. Small angular corrections are done with washers on one side of the ring to improve alignment if needed. Once the wire is tensioned, distraction is placed across the fracture to reduce the metaphysis. See Figures 32.7 to 32.9.
The alignment in the lateral view is examined. Often the foot can be manipulated into dorsi flexion to rotate the plafond around the horizontal reference wire. Arc wire technique and manipulation with half pins are used to correct apex anterior and posterior mal-alignment. Occasionally, during this phase of the reduction, it will become obvious that the
horizontal reference wire needs to be adjusted anterior or posterior on the ring to align the plafond anatomically. Once the plafond is aligned, at least two additional divergent olive wires are placed across the fracture in the 60-degree safe zone of wire pathways. A fourth wire is placed if space is available. Two wires are never adequate fixation. At least three olive wires should be placed. A medial-face half pin is added to the stable base. A minimum of two AP half pins and a medial-face half pin are necessary on the stable base. A fourth medial face pin is placed in large patients. See Figures 32.10, 32.11, 32.12, 32.13, 32.14, 32.15, 32.16, 32.17, 32.18 and 32.19.
horizontal reference wire needs to be adjusted anterior or posterior on the ring to align the plafond anatomically. Once the plafond is aligned, at least two additional divergent olive wires are placed across the fracture in the 60-degree safe zone of wire pathways. A fourth wire is placed if space is available. Two wires are never adequate fixation. At least three olive wires should be placed. A medial-face half pin is added to the stable base. A minimum of two AP half pins and a medial-face half pin are necessary on the stable base. A fourth medial face pin is placed in large patients. See Figures 32.10, 32.11, 32.12, 32.13, 32.14, 32.15, 32.16, 32.17, 32.18 and 32.19.
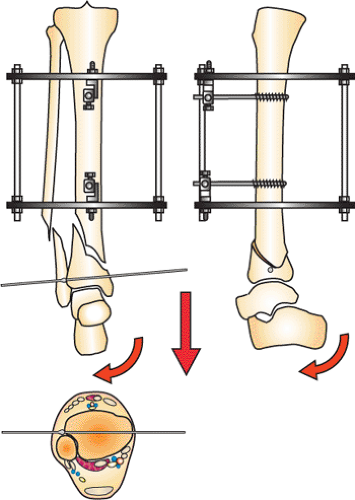 Figure 32.8. A horizontal reference wire is placed parallel to the anterior joint. The wire is placed approximately 8 to 12 mm above the joint. (Copyright © James J. Hutson, Jr., MD.) |
A sequential guide to type A and C1-2 distal tibia fractures is as follows:
The simple fracture of the C1-2 fracture is reduced and fixated with a 3.5- or 4.5-mm subchondral screw.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree