Lumbosacral radiculopathy is relatively common, and most cases resolve with appropriate conservative management. Along with pain control, the mainstay of treatment is a comprehensive rehabilitation program to correct for biomechanical factors that adversely affect spinal stability and predispose the patient to recurrent pain. Developing an appropriate treatment plan depends on thorough understanding of the structures providing core stability and the exercises to correct identifiable deficits. A comprehensive rehabilitation program includes postural training, muscle reactivation, correction of flexibility and strength deficits, and subsequent progression to functional exercises. This article reviews the current concepts regarding core stability and rehabilitation in lumbosacral radiculopathy.
The prevalence of lumbosacral radiculopathy has been reported to range from 9.9% to 25%. Lumbosacral radiculopathy may arise from a multitude of insults to the spinal nerve as it exits the lumbar spine. The classic description of radiculopathy is compromise of a spinal nerve with resultant pain, weakness, and/or sensory impairment in the distribution of the affected nerve root. This condition may be from direct trauma or from chemical irritation to the affected nerve root. Regardless of the underlying cause, injuries to the lumbar spine have been shown to adversely affect the core musculature and spinal stability. In theory, prolonged injury and pain lead to pain avoidance patterns, which can result in core muscle atrophy, loss of spine flexibility, and altered biomechanics of the spine. These conditions can significantly delay healing or even predispose to secondary injuries. This article reviews current concepts regarding core stability and rehabilitation in the setting of lumbosacral radiculopathy.
Overview
Core strengthening is widely used for both injury prevention and rehabilitation of the lumbar spine. The muscular core has been described as a box encasing the lumbar spine with the diaphragm on top, pelvic floor on bottom, abdominals anteriorly, and paraspinal and gluteal muscles postreiorly. Core musculature is required for the spine to move freely throughout its entire range of motion, and it also serves as a functional center of the kinetic chain by connecting the upper and lower extremities. The muscles of the pelvic girdle and shoulder, such as the hip abductors and scapular stabilizers, also contribute to core stability through connections to the spine and must not be overlooked in rehabilitation program design. Panjabi first described a model for spinal stability that consists of 3 components: the bone and ligamentous structures, the muscles surrounding the spine, and the neural input controlling the spine. The bone and ligamentous structures are thought to offer primarily passive stiffness, whereas the core musculature provides for stability through the full range of motion. Neural input allows for specific muscle activation patterns in both planned and unplanned movements. Low-back pain (LBP) has been shown to cause muscle atrophy and altered neural control of the spine musculature. In theory, these effects lead to altered spine biomechanics and thus progression of the degenerative spine cascade. Strengthening and activation of the core musculature are fundamental in the rehabilitation of spine injuries. Several studies have indicated the importance of a few muscles (transversus abdominis [TA] and the lumbar multifidi) ; however, as noted earlier, evaluation of the kinetic chain and activation of larger muscles are also important in the restoration of normal function and should be addressed in a comprehensive core stabilization program.
Anatomic principles of spinal stability
Ligaments and Osseous Structures
The ligaments and osseous structures combine to provide passive stiffness to the spine. The posterior osseous elements of the spine include the zygapophyseal (facet) joints, pedicles, lamina, and pars interarticularis. These structures have limited flexibility and are known to fail with repetitive loading through excessive lumbar flexion and extension. The portion of the spine that is anterior to the spinal cord is composed of the vertebral bodies, the intervertebral disks, and the anterior and posterior longitudinal ligaments. The intervertebral disk is composed of the annulus fibrosis, which encircles the nucleus pulposus. The end plates form a boundary between the disk and vertebral body. The disk can be injured through both compressive and shearing loads that cause injury initially to the end plates and ultimately to the annulus, thereby permitting disk herniation.
The ligaments of the spine include the supraspinous, interspinous, and intertransverse ligaments posteriorly; the elastic ligamentum flavum; and the anterior and posterior longitudinal ligaments on the anterior and posterior sides of the vertebral body, respectively. The anterior and posterior longitudinal ligaments may offer some protection from disk herniation. The combination of a strong anterior longitudinal ligament and limited lumbar extension makes anterior disk herniations rare. The posterior longitudinal ligament provides some protection from a pure posterior herniation, and most herniations occur in the posterolateral direction where the ligament thins and blends with the annulus fibrosis. As a whole, these ligaments seem to provide minimal inherent stability. In fact, it has been demonstrated that a cadaver with bones and ligaments intact but muscles removed buckles under about 9 kg. The role of these ligaments seems to be to provide some kinesthetic awareness as well as to serve as attachments and continuations of the back musculature and fascial planes.
Local Core Musculature
The major source of spinal stability arises from the activation and endurance of the core musculature, which is composed of several muscle groups. The deepest and smallest local spinal muscles include the multifidus, interspinales, and intertransversarii muscles. These muscles span only 2 or 3 spinal segments, and because of their short moment arm, these muscles are not thought to be involved in gross spinal movement. However, the organization of their fibers suggests stabilization of the spine in resisting unopposed lumbar flexion. In addition, their rich composition of muscle spindles suggests that these muscles act as segmental proprioceptive sensors of the spine.
Along with the multifidi, the TA has received attention in its stabilizing role in back pain. The TA runs in a hooplike fashion around the abdomen and attaches broadly to the thoracolumbar fascia. In healthy individuals, the deep fibers of the multifidi and the TA are the first fibers to activate when a limb is moved in response to visual stimulus, firing independently of limb movement direction to control intervertebral movement. In addition to stabilizing the core in preparation for limb movement, the TA has also been shown to increase the stiffness of the lumbar spine and the sacroiliac joints when activated. The multifidi and TA are found to atrophy in people with LBP, and there is evidence that the TA becomes dysfunctional in the setting of LBP. Laasonen studied postoperative patients with unilateral LBP and found that paraspinals were 10% to 30% smaller on the affected side when compared with the unaffected side. In patients with LBP and functional inactivity, biopsy results show selective type 2 atrophy of the multifidi and structural changes in type I fibers. Antigravity postural muscles have been shown to atrophy to a greater extent than lower extremity muscles in microgravity simulation models.
These changes in muscle composition in healthy individuals who stopped normal repetitive low-level activity patterns are thought to result in transformation of the muscle toward a more fatigable type of muscle fiber. All these studies suggest that these muscles are selectively vulnerable to atrophy and dysfunction in the setting of back pain. However, there is some evidence that with exercise training multifidi atrophy can be reversed.
Global Muscles Affecting the Core
Lateral to the multifidi is the erector spinae complex, which in the lumbar spine is composed of the longissimus and iliocostalis muscles. These are predominantly thoracic muscles, which attach directly by broad flat tendinous insertions (known as the erector spinae aponeurosis) to the iliac crests. In addition, the lumbar portions of the longissimus and iliocostalis originate from the lumbar vertebrae and attach on the ilium. These muscles provide lumbar extension and increase in lordosis when acting bilaterally and lateral bending when activated unilaterally. These muscles also act in opposition to spinal rotation. Patients with LBP have been shown to have decreased lumbar extensor endurance when compared with controls and to have abnormal trunk flexor to extensor strength ratios. The quadratus lumborum lies deep to the erector spinae and spans the regions from the 12th rib to the ilium, with interwoven portions to the expansive thoracolumbar fascia. It has been proposed to be a lumbar extensor as well as to provide lateral bending, and dysfunction can occur with weakness as well as unilateral shortening. The quadratus lumborum can be targeted in physical therapy for lumbar stabilization and is thought to be a key component in a core stabilization program. Anterior to the quadratus lumborum lies the psoas muscles, which arise from the anterior transverse processes and intervertebral disks of the thoracolumbar spine and insert on the femurs, acting primarily as a hip flexor. The psoas muscles may also increase lumbar lordosis when tight and may increase compressive loads of the lumbar spine when acting on the hip. Along with the TA, other circumferential muscles of the abdominal wall include the internal and external obliques. The rectus abdominis is located anteriorly and generally results in flexion of the lumbar spine and is less targeted in a core stabilization program. The internal obliques have a similar orientation of fibers to the TA, but they have received much less attention in the literature. The external obliques act as a check on the anterior pelvic tilt. Together these obliques act to allow for axial rotation and can be thought of as a stabilizing force to counter unwanted axial rotation as well.
The diaphragm and pelvic floor have also been shown to affect the lumbar spine. McGill and colleagues showed that ventilatory challenges may cause diaphragmatic dysfunction and thus lead to increased compressive loads on the lumbar spine. It has also been demonstrated that patients with sacroiliac joint pain have impaired recruitment in both the diaphragm and pelvic floor.
Discussion of the key core muscles is not complete without special attention paid to the thoracolumbar fascia and its associated musculature. This broad multilayered fascial sheath acts as an anchor for multiple muscles and allows for the distribution of kinetic chain forces from the lower to the upper extremities. Caudally it blends with the fascia of the gluteus maximus; cranially its attachments to the latissimus dorsi emphasize the importance of broadening the scope of the rehabilitation treatment plan to include functionally engaging tasks with the upper and lower extremities. In addition, this fascial sheath is also crucial to recall the role of the hip musculature. The hips transfer forces from the lower extremity to the spine during upright activities. Poor endurance in the hip extensors (gluteus maximus) and abductors (gluteus medius) has been noted in people with LBP. There has been a demonstrated association of hip extensor strength and subsequent occurrence of LBP in athletes tested in preparticipation physical examination. Asymmetries in hip extensor strength have also been found in female athletes with LBP.
Spinal Flexibility
Correction of spinal inflexibilities in addition to muscular imbalances has been advocated as an important component of rehabilitation of the spine. However, evidence is limited regarding the role of spine flexibility and injuries in the setting of lumbosacral radiculopathy. In addition, review of the literature yields conflicting reports as to the role of spine flexibility and range of motion in the treatment of spine injuries.
Several recent studies have suggested that there is no correlation between spinal flexibility and disability or function. Kuukkanen and Mälkiä suggested that in individuals with less severe back pain, flexibility did not play a role in the individuals’ overall functional ability. Similarly, a study by Sullivan and colleagues suggested that active lumbar spine flexion should not be used as a treatment goal. Kujala and colleagues looked at a 3-year longitudinal study in which specifically targeted training showed no increase in maximal lumbar extension in adolescent athletes. Moreover, the investigators suggested that aggressive attempts to increase lumbar flexibility could cause unnecessary stress to structures such as the intervertebral disks or the pars interarticularis.
In contrast, other studies have suggested that specific programs can help improve spinal flexibility. Magnusson and colleagues studied a group of patients with chronic LBP and suggested that increased trunk motion could be achieved by participation in a 2-week full-time rehabilitation program. The investigators noted that patients initially demonstrated a pain avoidance behavior but were able to achieve the confidence to recover despite their pain. Kibler and Chandler observed a specific conditioning program that effectively increased the lumbar flexibility in 51 tennis players. Kujala and colleagues also looked at lumbar flexibility and associated LBP between male and female athletes and controls. The investigators found that although no differences were observed between male athletes and controls, the female athletes (gymnasts and figure skaters) had increased overall and lower lumbar range of motion. In addition, decreased lumbar range of motion and decreased maximal extension were predictive of increased LBP in women. Despite the conflicting data regarding the effect of spinal flexibility programs on recovery, it seems reasonable to focus on specific areas of deficits.
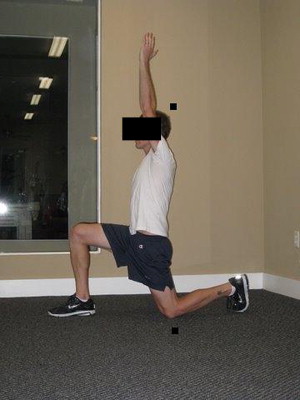
Common stretching programs include both spine-specific stretching exercises and lower extremity stretching exercises ( Fig. 1 ). Avoidance of aggravating positions in the setting of radiculopathy is prudent and should be addressed by the clinician when initiating a core stabilization program. Generally, avoidance of spinal flexion is advised in the setting of disk herniation, and avoidance of excessive lumbar extension is advised if there is compromise of the neural foramen by the posterior elements.
Anatomic principles of spinal stability
Ligaments and Osseous Structures
The ligaments and osseous structures combine to provide passive stiffness to the spine. The posterior osseous elements of the spine include the zygapophyseal (facet) joints, pedicles, lamina, and pars interarticularis. These structures have limited flexibility and are known to fail with repetitive loading through excessive lumbar flexion and extension. The portion of the spine that is anterior to the spinal cord is composed of the vertebral bodies, the intervertebral disks, and the anterior and posterior longitudinal ligaments. The intervertebral disk is composed of the annulus fibrosis, which encircles the nucleus pulposus. The end plates form a boundary between the disk and vertebral body. The disk can be injured through both compressive and shearing loads that cause injury initially to the end plates and ultimately to the annulus, thereby permitting disk herniation.
The ligaments of the spine include the supraspinous, interspinous, and intertransverse ligaments posteriorly; the elastic ligamentum flavum; and the anterior and posterior longitudinal ligaments on the anterior and posterior sides of the vertebral body, respectively. The anterior and posterior longitudinal ligaments may offer some protection from disk herniation. The combination of a strong anterior longitudinal ligament and limited lumbar extension makes anterior disk herniations rare. The posterior longitudinal ligament provides some protection from a pure posterior herniation, and most herniations occur in the posterolateral direction where the ligament thins and blends with the annulus fibrosis. As a whole, these ligaments seem to provide minimal inherent stability. In fact, it has been demonstrated that a cadaver with bones and ligaments intact but muscles removed buckles under about 9 kg. The role of these ligaments seems to be to provide some kinesthetic awareness as well as to serve as attachments and continuations of the back musculature and fascial planes.
Local Core Musculature
The major source of spinal stability arises from the activation and endurance of the core musculature, which is composed of several muscle groups. The deepest and smallest local spinal muscles include the multifidus, interspinales, and intertransversarii muscles. These muscles span only 2 or 3 spinal segments, and because of their short moment arm, these muscles are not thought to be involved in gross spinal movement. However, the organization of their fibers suggests stabilization of the spine in resisting unopposed lumbar flexion. In addition, their rich composition of muscle spindles suggests that these muscles act as segmental proprioceptive sensors of the spine.
Along with the multifidi, the TA has received attention in its stabilizing role in back pain. The TA runs in a hooplike fashion around the abdomen and attaches broadly to the thoracolumbar fascia. In healthy individuals, the deep fibers of the multifidi and the TA are the first fibers to activate when a limb is moved in response to visual stimulus, firing independently of limb movement direction to control intervertebral movement. In addition to stabilizing the core in preparation for limb movement, the TA has also been shown to increase the stiffness of the lumbar spine and the sacroiliac joints when activated. The multifidi and TA are found to atrophy in people with LBP, and there is evidence that the TA becomes dysfunctional in the setting of LBP. Laasonen studied postoperative patients with unilateral LBP and found that paraspinals were 10% to 30% smaller on the affected side when compared with the unaffected side. In patients with LBP and functional inactivity, biopsy results show selective type 2 atrophy of the multifidi and structural changes in type I fibers. Antigravity postural muscles have been shown to atrophy to a greater extent than lower extremity muscles in microgravity simulation models.
These changes in muscle composition in healthy individuals who stopped normal repetitive low-level activity patterns are thought to result in transformation of the muscle toward a more fatigable type of muscle fiber. All these studies suggest that these muscles are selectively vulnerable to atrophy and dysfunction in the setting of back pain. However, there is some evidence that with exercise training multifidi atrophy can be reversed.
Global Muscles Affecting the Core
Lateral to the multifidi is the erector spinae complex, which in the lumbar spine is composed of the longissimus and iliocostalis muscles. These are predominantly thoracic muscles, which attach directly by broad flat tendinous insertions (known as the erector spinae aponeurosis) to the iliac crests. In addition, the lumbar portions of the longissimus and iliocostalis originate from the lumbar vertebrae and attach on the ilium. These muscles provide lumbar extension and increase in lordosis when acting bilaterally and lateral bending when activated unilaterally. These muscles also act in opposition to spinal rotation. Patients with LBP have been shown to have decreased lumbar extensor endurance when compared with controls and to have abnormal trunk flexor to extensor strength ratios. The quadratus lumborum lies deep to the erector spinae and spans the regions from the 12th rib to the ilium, with interwoven portions to the expansive thoracolumbar fascia. It has been proposed to be a lumbar extensor as well as to provide lateral bending, and dysfunction can occur with weakness as well as unilateral shortening. The quadratus lumborum can be targeted in physical therapy for lumbar stabilization and is thought to be a key component in a core stabilization program. Anterior to the quadratus lumborum lies the psoas muscles, which arise from the anterior transverse processes and intervertebral disks of the thoracolumbar spine and insert on the femurs, acting primarily as a hip flexor. The psoas muscles may also increase lumbar lordosis when tight and may increase compressive loads of the lumbar spine when acting on the hip. Along with the TA, other circumferential muscles of the abdominal wall include the internal and external obliques. The rectus abdominis is located anteriorly and generally results in flexion of the lumbar spine and is less targeted in a core stabilization program. The internal obliques have a similar orientation of fibers to the TA, but they have received much less attention in the literature. The external obliques act as a check on the anterior pelvic tilt. Together these obliques act to allow for axial rotation and can be thought of as a stabilizing force to counter unwanted axial rotation as well.
The diaphragm and pelvic floor have also been shown to affect the lumbar spine. McGill and colleagues showed that ventilatory challenges may cause diaphragmatic dysfunction and thus lead to increased compressive loads on the lumbar spine. It has also been demonstrated that patients with sacroiliac joint pain have impaired recruitment in both the diaphragm and pelvic floor.
Discussion of the key core muscles is not complete without special attention paid to the thoracolumbar fascia and its associated musculature. This broad multilayered fascial sheath acts as an anchor for multiple muscles and allows for the distribution of kinetic chain forces from the lower to the upper extremities. Caudally it blends with the fascia of the gluteus maximus; cranially its attachments to the latissimus dorsi emphasize the importance of broadening the scope of the rehabilitation treatment plan to include functionally engaging tasks with the upper and lower extremities. In addition, this fascial sheath is also crucial to recall the role of the hip musculature. The hips transfer forces from the lower extremity to the spine during upright activities. Poor endurance in the hip extensors (gluteus maximus) and abductors (gluteus medius) has been noted in people with LBP. There has been a demonstrated association of hip extensor strength and subsequent occurrence of LBP in athletes tested in preparticipation physical examination. Asymmetries in hip extensor strength have also been found in female athletes with LBP.
Spinal Flexibility
Correction of spinal inflexibilities in addition to muscular imbalances has been advocated as an important component of rehabilitation of the spine. However, evidence is limited regarding the role of spine flexibility and injuries in the setting of lumbosacral radiculopathy. In addition, review of the literature yields conflicting reports as to the role of spine flexibility and range of motion in the treatment of spine injuries.
Several recent studies have suggested that there is no correlation between spinal flexibility and disability or function. Kuukkanen and Mälkiä suggested that in individuals with less severe back pain, flexibility did not play a role in the individuals’ overall functional ability. Similarly, a study by Sullivan and colleagues suggested that active lumbar spine flexion should not be used as a treatment goal. Kujala and colleagues looked at a 3-year longitudinal study in which specifically targeted training showed no increase in maximal lumbar extension in adolescent athletes. Moreover, the investigators suggested that aggressive attempts to increase lumbar flexibility could cause unnecessary stress to structures such as the intervertebral disks or the pars interarticularis.
In contrast, other studies have suggested that specific programs can help improve spinal flexibility. Magnusson and colleagues studied a group of patients with chronic LBP and suggested that increased trunk motion could be achieved by participation in a 2-week full-time rehabilitation program. The investigators noted that patients initially demonstrated a pain avoidance behavior but were able to achieve the confidence to recover despite their pain. Kibler and Chandler observed a specific conditioning program that effectively increased the lumbar flexibility in 51 tennis players. Kujala and colleagues also looked at lumbar flexibility and associated LBP between male and female athletes and controls. The investigators found that although no differences were observed between male athletes and controls, the female athletes (gymnasts and figure skaters) had increased overall and lower lumbar range of motion. In addition, decreased lumbar range of motion and decreased maximal extension were predictive of increased LBP in women. Despite the conflicting data regarding the effect of spinal flexibility programs on recovery, it seems reasonable to focus on specific areas of deficits.
Common stretching programs include both spine-specific stretching exercises and lower extremity stretching exercises ( Fig. 1 ). Avoidance of aggravating positions in the setting of radiculopathy is prudent and should be addressed by the clinician when initiating a core stabilization program. Generally, avoidance of spinal flexion is advised in the setting of disk herniation, and avoidance of excessive lumbar extension is advised if there is compromise of the neural foramen by the posterior elements.







