Uncemented femoral implants of various designs have proved to provide stable initial and long-term fixation in patients who undergo total hip arthroplasty. Challenges in primary total hip arthroplasty have led to the evolution of short stem designs. These challenges include proximal/metaphyseal and distal/diaphyseal mismatch; facilitation of less-invasive surgical exposures, especially the direct anterior approach; and bone preservation for potential revision surgery.
Key points
- •
Metaphyseal fit and ingrowth can provide both rotational and axial stability without distal diaphyseal support.
- •
Bone remodeling on radiographic analysis of short stems of various designs show endosteal condensation and cortical hypertrophy in the proximal metaphyseal region of the femur.
- •
Functional Harris Hip Scores (HHS) and Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain scores are equivalent in patients with metaphyseal-engaging short stems compared with stems of conventional length.
- •
Short stem metaphyseal-engaging implants enhance the preservation of proximal femoral bone stock as well as provide an adaptive alternative in minimally invasive anterior approaches.
- •
Metaphyseal-engaging short stems provide an alternative to bone preservation procedures with reproducible and reliable radiographic and clinical outcomes while maintaining a short learning curve.
Introduction
Total hip arthroplasty (THA) has proved clinically and functionally successful in the treatment of end-stage degenerative joint disease of the hip. Porous-coated, uncemented femoral stems were introduced for use in THA in the early 1980s. Uncemented implants rely on diaphyseal or metaphyseal contact and, ultimately, bone fixation to ingrowth or ongrowth surfaces to provide long-term stability and dependable clinical results. Uncemented, porous femoral implants are now routinely used in virtually all patients undergoing primary THA. Uncemented femoral components with a variety of shapes, metallurgy, and surface treatment have been developed to address the broad spectrum of proximal femoral morphology.
Despite the documented success of these implants, current uncemented stems are used in patients whose size, age, level of physical activity, and bone quality present particular challenges for uncemented fixation technologies. These challenges include (1) the preservation of proximal femoral bone stock; (2) the potential need for effective, femoral component revision; (3) proximal-distal mismatch; and (4) the ability to insert implants safely, securely, and reproducibly with specific surgical approaches (eg, the direct anterior) that are currently being evaluated and promoted.
Short stem uncemented femoral implants have been developed to address some of these challenges while maintaining the current level of success achieved by uncemented implants of conventional length ( Fig. 1 ). Short stem implants have been defined as 120 mm in length or less, which approximately correlates to the metadiaphyseal junction of the proximal femur.

The purposes of this article are to (1) explain the evolution to short stem design, (2) describe the rationale and types of short stem implants, (3) provide the benefits of short stem implants, and (4) summarize the clinical results with these implants.
Introduction
Total hip arthroplasty (THA) has proved clinically and functionally successful in the treatment of end-stage degenerative joint disease of the hip. Porous-coated, uncemented femoral stems were introduced for use in THA in the early 1980s. Uncemented implants rely on diaphyseal or metaphyseal contact and, ultimately, bone fixation to ingrowth or ongrowth surfaces to provide long-term stability and dependable clinical results. Uncemented, porous femoral implants are now routinely used in virtually all patients undergoing primary THA. Uncemented femoral components with a variety of shapes, metallurgy, and surface treatment have been developed to address the broad spectrum of proximal femoral morphology.
Despite the documented success of these implants, current uncemented stems are used in patients whose size, age, level of physical activity, and bone quality present particular challenges for uncemented fixation technologies. These challenges include (1) the preservation of proximal femoral bone stock; (2) the potential need for effective, femoral component revision; (3) proximal-distal mismatch; and (4) the ability to insert implants safely, securely, and reproducibly with specific surgical approaches (eg, the direct anterior) that are currently being evaluated and promoted.
Short stem uncemented femoral implants have been developed to address some of these challenges while maintaining the current level of success achieved by uncemented implants of conventional length ( Fig. 1 ). Short stem implants have been defined as 120 mm in length or less, which approximately correlates to the metadiaphyseal junction of the proximal femur.

The purposes of this article are to (1) explain the evolution to short stem design, (2) describe the rationale and types of short stem implants, (3) provide the benefits of short stem implants, and (4) summarize the clinical results with these implants.
Evolution to short stem design
To understand the evolution of uncemented THA to short stem implants, femoral implant design and stability must first be reviewed. Successful THA relies on initial and long-term rotational and axial stability. The diaphyseal portion (cylindrical or tapered) of the femoral implant contributes to the initial stability. Cylindrical, extensively porous-coated implants (eg, AML) achieve durable fixation but can be associated with stress shielding and thigh pain. Cylindrical implants without porous-coated stems achieve varying degrees of initial axial and rotational stability through contact points in the diaphysis but rely on metaphyseal bone contact to enhance their initial rotational stability. Furthermore, these implants seek long-term fixation and stability through bone ingrowth or ongrowth at the metaphysis. Long-term clinical results of these implants have been satisfactory and reliable with an overall lower incidence of thigh pain and proximal stress shielding relative to their extensively coated counterparts. Early concerns with a cylindrical diaphysis, however, inspired investigators to produce tapered stems.
Tapered uncemented implants achieve primary axial fixation through a 3-point contact mechanism with the creation, and ultimate relaxation, of hoop stresses between a tapered stem and cylindrical femur. Rotational stability is achieved in the proximal femur through surface treatment, various shape geometries, and overall fit and fill. Secondary fixation depends on the extent of contact between the ingrowth/ongrowth surfaces of the implant and metaphyseal bone. Many studies have established the long-term clinical and radiographic reliability and durability of tapered femoral implants. These stems have been associated with little thigh pain compared with cylindrical stems.
In these designs, the tapered or uncoated cylindrical diaphyseal portion provides primary axial stability but varying degrees of rotational stability. Rather, rotational stability is attained from metaphyseal bone-implant contact.
Design rationale and types of uncemented short stem metaphyseal-engaging femoral implants
Short stem metaphyseal-engaging implants achieve secure initial fixation in the metaphysis, theoretically making the axial and rotational stability provided by the diaphyseal portion of the femoral implant negligible. Metaphyseal ingrowth or ongrowth secures long-term fixation, with the pattern of bone implant contact varying by implant design. A variety of implants have been introduced over the past few years, leading to the development of a classification system by McTighe and colleagues. The 3 main types of short stem implants are
- 1.
Metaphyseal stabilized (standard neck resection) ( Fig. 2 A )
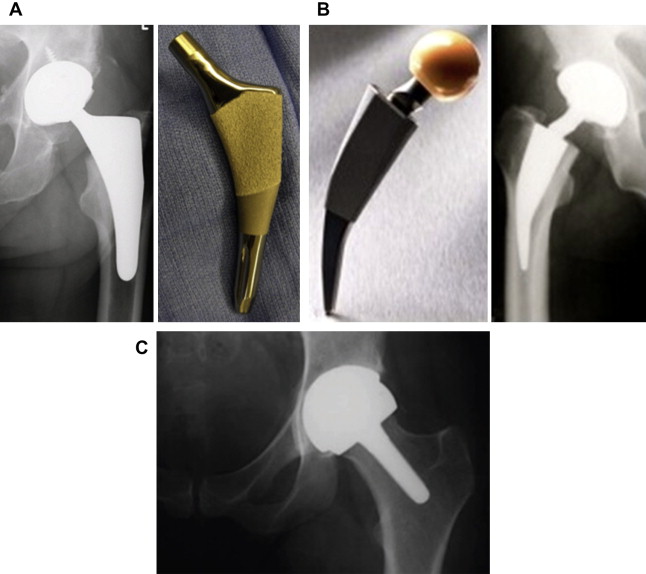
Fig. 2
( A ) Metaphyseal-stabilized implant (standard neck resection). ( B ) Neck-stabilized implant (femoral neck sparing). ( C ) Head-stabilized implant.
- 2.
Neck stabilized (femoral neck sparing) (see Fig. 2 B)
- 3.
Head stabilized (resurfacing-type procedures) (see Fig. 2 C)
Standard neck resection short stem implants can further be classified into (a) anatomic and (b) wedge fit implants. These implants also tend to be shortened versions of conventional uncemented implants. Femoral neck-sparing or neck-preserving implants instead have unique design features to accommodate the native anteversion of the femoral neck. Head-stabilized short stem implants commission a completely different surgical technique and necessitate specific clinical indications; thus, they are not discussed in this article.
Femoral neck-sparing or high femoral neck resection designs seek to optimize proximal load transfer by engaging solely the femoral neck and the metaphysis. A more proximal and horizontal femoral neck osteotomy produces an oval-shaped intramedullary opening compared with a standard cut, which offers a broad opening ( Fig. 3 ). Studies have shown greater resistance to torsional stresses with these high-neck osteotomies. The concept of femoral neck preservation in uncemented designs has been well described since the earliest days of arthroplasty. Proponents of this concept have suggested improved bone and soft tissue preservation. Moreover, soft tissue preservation enhances implant fixation, reduces surgical morbidity, improves abductor function, and preserves bone stock for potential future surgery.
Santori and Santori reported satisfactory midterm results in a high femoral neck resection short stem implant. They performed a complete clinical review at a mean interval of 8 years in their cohort of patients under the age of 60 who underwent THA. Despite other encouraging results reported by the developers of uncemented femoral components inserted with high femoral neck resection, widespread use of these devices has not yet occurred.
Several reasons have been proposed for the slow adoption of this concept:
- 1.
The surgical technique for inserting stems of this design is different from and potentially more difficult than more standard neck resection approaches. The long retained femoral neck can make exposure of the acetabulum difficult.
- 2.
Accurate, reproducible alignment of the femoral stem within the diaphysis may be difficult to accomplish given the native anteversion of neck shaft.
- 3.
The small surface area of bone at the proximal femoral neck makes restoration of accurate leg length and avoidance of lengthening of the extremity difficult to achieve.
- 4.
The high-neck resection limits exposure of the metaphysis and may reduce the extent and reliability with which metaphyseal fit and contact can be achieved.
- 5.
The combination of high-neck resection and short stems may be associated with an increased incidence of proximal femoral fractures.
- 6.
A high femoral neck resection may result in increased bone-bone impingement and, subsequently, a reduction in range of motion.
Initial experimentation with femoral neck preservation short stem implants may have been considered a radical shift in paradigm at the time. Recent renewed interest in these stems is largely due to a natural progression of uncemented femoral components from cylindrical to tapered to shortened designs. Design teams continue to develop high-neck resection implants based on encouraging results from original designs and aim to address some of the design flaws (discussed previously) ( Fig. 4 ). For example, the Fitmore stem (Zimmer, Warsaw, Indiana) has variability in its curve to allow for greater medial calcar contact for enhanced stability ( Fig. 5 ). Development of these devices is spurred by a renewed interest in the use of the direct anterior approach for THA, the desire for surgical and implant approaches that minimize soft tissue and bone trauma, and a concern about proximal bone preservation and positive bone remodeling.
Standard neck resection metaphyseal-engaging short stem implants tend to be shortened versions of commercially available conventional-length uncemented femoral implants ( Fig. 6 ). These stems have shortened tapered or cylindrical diaphyseal-reaching stems and a wide variety of metaphyseal shapes. The 2 main categories of metaphyseal shapes include 2-D or 3-D taper shapes that achieve 2-point wedge fixation in the metaphysis and anatomic shapes that seek to fit and fill the metaphysis. Theoretic studies have shown that the use of a lateral flare configuration reduces distal femoral stress transfer in conventional-length uncemented femoral components by engaging the proximal lateral, medial, and anterior cortices. Use of this rationale has extended into short stem designs.
Proponents of these short stem designs state the proximal metaphyesal fixation achieved is adequate for initial and long-term stability. Various designs have been shown to have reliable fixation and successful clinical and radiographic outcomes up to 8 years postoperatively. Two-point wedge designs attempt to achieve contact and fit at the metaphyseal-diaphyseal junction. Although these implants can be tapered in 2 or 3 dimensions, the wedge-fit is primarily 2-point at the medial and lateral cortices ( Fig. 7 ). Anterior and/or posterior endosteal contact is variable on design. Similarly, anatomic implants attempt fit and fill the metaphysis—in the coronal or sagittal planes or in both.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





