Abstract
Introduction
The piriformis muscle syndrome (PMS) has remained an ill-defined entity. It is a form of entrapment neuropathy involving compression of the sciatic nerve by the piriformis muscle. Bearing this in mind, a medical examination is likely to be suggestive, as a classical range of symptoms corresponds to truncal sciatica with frequently fluctuating pain, initially in the muscles of the buttocks.
Pathophysiological hypotheses
The piriformis muscle is biarticular, constituting a bridge in front of and below the sacroiliac joint and behind and above the coxo-femoral joint. It is essentially a lateral rotator but also a hip extensor, and assumes a secondary role as an abductor. Its action is nonetheless conditioned by the position of the homolateral coxo-femoral joint, and it can also function as a hip medial rotator, with the hip being flexed at more than 90°. The main clinical manoeuvres are derived from these types of biomechanical considerations. For instance, as it is close to the hip extensors, the piriformis muscle is tested in medial rotation stretching, in resisted contraction in lateral rotation. On the other hand, when hip flexion surpasses 90°, the piriformis muscle is stretched in lateral rotation, and we have consequently laid emphasis on the manoeuvre we have termed Heel Contra-Lateral Knee (HCLK), which must be prolonged several tens of seconds in order to successfully reproduce the buttocks-centred and frequently associated sciatic symptoms.
Conclusion
A PMS diagnosis is exclusively clinical, and the only objective of paraclinical evaluation is to eliminate differential diagnoses. The entity under discussion is real, and we favour the FAIR, HCLK and Freiberg stretching manoeuvres and Beatty’s resisted contraction manoeuvre.
Résumé
Introduction
Le syndrome du muscle piriforme (SMP) est une entité encore mal définie. Il s’agirait d’un syndrome canalaire par compression du nerf ischiatique par le muscle piriforme. Dans ce cadre, l’interrogatoire est évocateur, la symptomatologie clinique correspondant à une sciatalgie tronculaire souvent fluctuante à début fessier.
Hypothèses physiopathologiques
Ce muscle piriforme est bi-articulaire, passant en pont en avant et en dessous de l’articulation sacro-iliaque et en arrière et au-dessus de l’articulation coxo-fémorale. Il est essentiellement rotateur latéral mais aussi extenseur de hanche et participe accessoirement à son abduction. Pour autant son action est conditionnée par la position de l’articulation coxo-fémorale homolatérale. En effet, il deviendrait rotateur médial de hanche, cette dernière étant fléchie au-delà de 90°. De ces considérations biomécaniques découlent les principales manœuvres cliniques. En effet, hanche proche de l’extension, il est testé en étirement en rotation médiale, en contraction contrariée en rotation latérale. En revanche, au-delà de 90° de flexion de hanche, le muscle piriforme est étiré en rotation latérale, et ainsi nous mettons en avant la réalisation d’une manœuvre que nous avons appelé Talon Genou-Contro-Latéral (TG-CL), qu’il faut prolonger plusieurs dizaines de secondes pour reproduire la symptomatologie fessière et souvent sciatique associée.
Conclusion
Le diagnostic de SMP est clinique, le bilan paraclinique n’ayant pour but que d’éliminer un diagnostic différentiel. Son entité est réelle et nous privilégions les manœuvres d’étirement FAIR, TG-CL et de Freiberg, ainsi que la manœuvre de contraction résistée de Beatty.
1
English version
1.1
Introduction
The piriformis muscle syndrome (PMS) is defined as an entrapment neuropathy involving compression of the sciatic nerve by the piriformis muscle and entailing a number of symptoms with truncal sciatic pain, initially in the muscles of the buttocks.
An initial description was given by Yeoman in 1928 . In 1934, Freiberg recognized the signs specific to this syndrome , but it was only in 1947 that Robinson called this clinical entity the “piriformis”, or pyramidal syndrome .
The clinical and paraclinical elements reported in different descriptions of the syndrome have at times been discrepant and called its reality into question . It nonetheless remains one of the rare causes of non-spinal sciatica consecutive to undeniable entrapment neuropathy when the sciatic nerve crosses through the infra-piriformis canal .
The etiologies suggested in considerations of sciatic nerve compression are diversified: inflammatory, traumatic, tumoral and malformative . In most cases, however, the compression is originally muscular, and the piriformis muscle is suspected .
In this work, we have focused upon the PMS originating in the muscles.
Our objective is, on the basis of anatomical descriptions of the piriformis muscle, to provide support for pathophysiological hypotheses and to subsequently discuss the clinical tests most pertinent to diagnosis.
1.2
Method
Based on the anatomical descriptions of the piriformis muscle, dissections were performed in the anatomy laboratory on embalmed adult human cadavers. Dissection was carried out classically, segment by segment, so as to highlight the relations of the external pelvic portion of the piriformis muscle in the external iliac fossa. The different pathophysiological hypotheses were drawn from a review of the existing literature on the syndrome, with biomechanical and functional references included.
The clinical tests were discussed subsequent to review of the literature and of our personal experience, and were premised on muscle biomechanics.
1.3
Anatomy
The piriformis muscle is actually a muscle pair possessing a triangular muscle of which the base is inserted on each side of the ventral surface of the sacrum at the edges of the 2nd and 3rd sacral foramens.
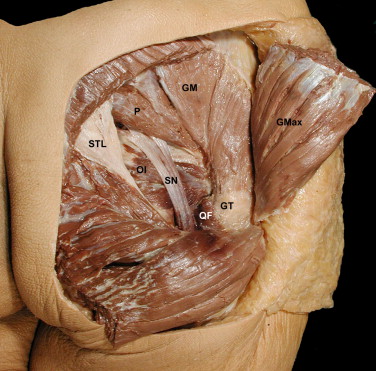
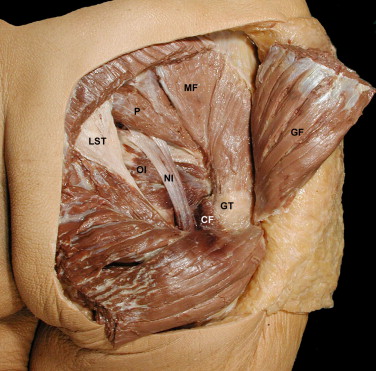
The piriformis muscle exits the pelvic cavity by sliding under the greater sciatic notch of the coxal bone, above the sacral spinal ligament. It then runs diagonally downwards through the gluteal region and culminates on the upper side of the greater trochanter of the femur ( Fig. 1 ). In the gluteal region, it is located under the gluteus maximus and above the internal obturator muscle ending, which is accompanied by the gemelli muscles. So it is that the piriformis muscle delimits the two zones of musculoligamentous passages known as the supra-piriformic and infra-piriformis foramens. The superior gluteal nerves and vessels traverse the supra-piriformis foramen. Along with the inferior gluteal and pudendal nerves, the sciatic nerve passes through the infra-piriformis canal.
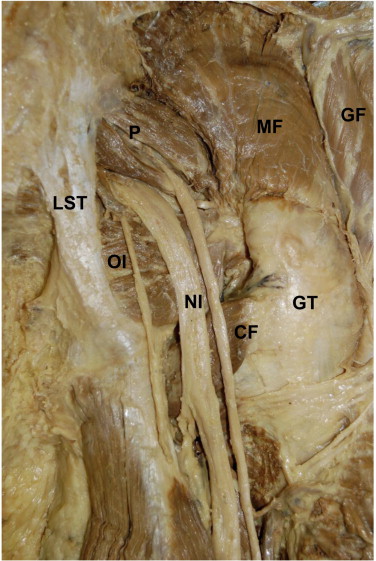
With regard to the traversing of the infra-piriformis foramen by the sciatic nerve, anatomical variations exist, and they specifically involve the traversing of the muscle by the tibial or peroneous contingent of the sciatic nerve (11.7%). The tibial contingent can also run above the piriformis muscle, in the supra-piriformic canal, while the common fibular nerve runs through the infra-piriformic canal (3.3%). Less frequently, the sciatic nerve taken as a whole can go so far as to span the piriformis muscle (0.8%) ( Fig. 2 ) . These anatomical configurations are neither clinically recognizable nor easily identifiable through imagery, yet they are suggested in the event of possible PMS .
The piriformis muscle is essentially a lateral hip rotator, but it is also an extensor. It may take on a secondary role as an abductor when its point of support on the sacrum is proximal .
1.4
Pathophysiological hypotheses
Anatomical acquaintance with the piriformis muscle and its relationships of proximity facilitates comprehension of the pathophysiology of sciatic nerve compression in the PMS. Can a morphological alteration (contracture, hypertrophy) lead to compression of the sciatic nerve? Can the relationships of the different anatomical structures modified by biomechanical constraints shrink the supra-piriformis and infra-piriformis passageways?
Even when not taking into account any possible morphological modifications of the piriformis muscle body, its complex proximal insertion appears likely to create zones of conflict. On this subject, Paturet has described two types of insertion of the muscle on the ventral or pelvic surface of the sacrum . The first and principal type is composed of aponeurotic fascia entwined with the fleshy fibres at the proximal extremity of the muscle. The ventral branches of the 2nd and 3rd sacral spinal nerves emerge from their sacral foramen by passing through the muscle, thereby endowing it with a bundled or fasciculated aspect, and then positioning themselves on the ventral surface of the muscle body, against which they are pressed by its fascia covering.
The second and secondary type of insertion is less widely extended, originating at the upper edge of the greater sciatic notch in front of the sacroiliac joint space and the lateral side of the piriformis muscle tuber (Morestin’s tuber) belonging to the bony ridge. At this level, there also exist aponeurotic insertions on the lateral side of the sacrotuberous ligament at the location where the piriformis muscle exits the greater sciatic notch. According to their development, the insertions may also limit in size the infra- and supra-piriformis foramens.
The distal femoral insertions of the piriformis muscle also constitute the locus of tendinous expansion toward the different structures located at the posterior superior edge of the greater trochanter. In that way, the ending of the internal obturator muscle and the gemelli muscles is closely connected with the ending of the piriformis muscle by means of solid layers of fibrous material. The terminal tendon of the gluteus medius muscle likewise mixes its fibres with the terminal tendons of the preceding muscles.
This mixture of fibres explains the involvement of the piriformis muscle in the complex movements of the hip.
The piriformis muscle is biarticular, constituting a bridge in front of the sacroiliac joint and behind the coxo-femoral joint. And so, in cases of PMS, it is necessary to closely examine coxo-femoral and sacroiliac pain .
Snijders et al. have underlined the stabilizing role of the piriformis muscle on the sacroiliac joint and described its being stretched out in seated and cross-legged positions.
From a qualitative standpoint, a positional factor such as prolonged sitting has often been reported, as from a quantitative standpoint has intense physical activity such as long-distance or cross-country running, at times with a load . In the seated position, especially when the torso is sagitally straight, the pelvis carries out an anteversion movement provoking tension in the sacrotuberal ligament strongly associated with the piriformis muscle. During a footrace, the constraints endured by the sacroiliac joints drive the lower extremity of the sacrum upwards, and yet it is held back by several ligaments, including the sacrotuberal.
1.5
Clinical diagnostic criteria
The symptoms suggesting PMS are clinical, bringing together the patient’s painful functional impairments and the signs reproduced by physical manoeuvres soliciting the piriformis muscle and the environing anatomical structures.
While some of the tests we shall report have been referenced in the literature, others are derived from personal considerations, and have at times involved adaptation of postures taken in the framework of physical rehabilitation .
Telltale warning signs correspond to pain spreading from the buttocks through the sciatic territory; its fluctuating development is favoured by intense effort and, more particularly, by “trigger” postures. In the first place, initial clinical assessment must preclude lombosciatica of discal origin, coxo-femoral joint pain or sacroiliac joint pathology. Anamnesis in a search during the initial interview for vertebral pathologies, a coxo-femoral pathology or a pelvic pathology should include questioning on rhumatological antecedents. Direct trauma in the buttocks region is also to be eliminated, since it can lead to contusion of the structures of the gluteal region. More precisely, it is necessary to seek out contributory factors and stress factors, to specify sports of which the practice is risky (distance running, cycling, horse riding) and exposed professions involving prolonged periods in a seated position (truck driver, taxi driver…) .
Static morphological examination allows for identification of anomalies in sagittal pelvis positioning, in lower limb length or in hip flexion deformity, all of which may favour the appearance of PMS.
Inspection of the patient in a supine recumbent position can reveal an attitude of the lower limb in excessive lateral rotation that may provide evidence of piriformis muscle contracture. An examiner’s attempt to correct this attitude may provoke or intensify recognized pain .
During palpation of the gluteal region and notwithstanding the presence of the gluteus maximus muscle, it is frequently possible to perceive an indurated and painful cord along the trajectory of the piriformis muscle . In a patient in a contralateral lateral decubitus position, the examiner places the hip of the painful lower member at 45° of flexion and in light internal rotation, with the knee propped on the examination table. The piriformis muscle is palpated 1 to 2 cm below the middle third of a line drawn between the posterior superior iliac spine and the upper boundary of the greater trochanter.
Physical examination of a patient suspected of PMS is focused on specific manoeuvres putting the piriformis muscle under stress. These manoeuvres may provoke repercussions on the sciatic nerve and also on the posterior femoral cutaneous nerve, a sensitive branch of the inferior gluteal nerve.
The different manoeuvres are aimed at reproducing the pain experienced by the patient: buttock pain and sciatic tingling or numbness in the limb affected, and accompanied in some cases by distal paresthesia. It is often necessary to prolong these manoeuvres for several tens of seconds so that the sciatic pain may appear.
Five of these manoeuvres have been described in the literature: Freiberg’s forceful internal rotation , the Flexion Adduction and Internal Rotation (FAIR) initially described by Solheim , Pace and Nagle’s resisted contraction manoeuvre , Beatty’s manoeuvre and the Fishman FAIR Test . None of these manoeuvres have had their sensitivity and specificity rigorously validated.
Four other manoeuvres have been derived from the previously presented anatomical, biomechanical and functional considerations. They include the medial rotation stress known as Procubitus Adduction Medial Rotation (PAMR), sensitized Hand Floor Distance (HFD), Lasègue’s sensitized manoeuvre and the lateral rotation stress manoeuvre highlighted by our team and named Heel Contra-Lateral Knee (HCLK) ( Fig. 3 ).

1.5.1
Freiberg manoeuvre
On a patient in recumbent supine position, the examiner provokes internal rotation and adduction of the affected lower limb, with the hip in 30° to 45° flexion and the knee in extension.
1.5.2
FAIR manoeuvre (flexion – adduction – internal rotation)
On a patient in recumbent supine position, the lower limb under examination is taken into adduction and internal rotation, with the hip and the knee in 90° flexion.
1.5.3
Pace and Nagle manoeuvre
With his legs dangling over the edge of the examination table, the seated patient is asked to separate his knees against the manual resistance of the examiner.
1.5.4
Beatty manoeuvre
The patient is placed in lateral decubitus position on the healthy side. On the painful side, the hip and the knee are in flexion, thereby allowing the medial surface of the knee to be propped on the examination table and the foot to be hooked behind the leg of the healthy limb. The patient is asked to carry out a movement of lateral rotation and hip abduction against the manual resistance of the examiner.
1.5.5
Fishman FAIR test (Flexion – Adduction – Internal Rotation test)
The starting position is the same as that of the Beatty manoeuvre, but a foot is hooked behind the heel of the healthy limb. The patient actively raises the foot along the dorsal side of the leg.
1.5.6
Procubitus Adduction Medial Rotation (PAMR) manoeuvre
On a patient in ventral decubitus, adduction coupled with medial rotation of the limb is imposed on the affected lower limb, with the knee in 90° flexion.
1.5.7
Hand Floor Distance (HFD) sensitized manoeuvre in medial rotation
These are forward-flexion tests of the pelvis, with the lower limbs placed in different positions:
- •
feet together and parallel to each other, with the coxo-femoral joints in an intermediate position of rotation;
- •
forefeet directed inwards, with the coxo-femoral joints in medial rotation.
The hand-floor distance at which the gluteal pain and sciatic tingling are reproduced is measured (in centimetres) for the two positions. In PMS cases, HFD is greater in the medial rotation position.
1.5.8
Lasègue’s sensitized manoeuvre
As is not the case with sciatica originating in nerve root impingement, Lasègue’s manoeuvre is most often negative with regard to PMS. On the other hand, suggestively painful symptoms can be reproduced during this sensitive manoeuvre through maximal medial rotation of the affected pelvic limb.
1.5.9
Heel Contra-Lateral Knee (HCLK) manoeuvre
The patient places the heel of the foot of his painful lower limb above the contralateral knee, with the hip of the affected side thereby placed in extreme lateral rotation and flexion, while the knee is likewise in flexion ( Fig. 3 ). The examiner straightens the legs as much as possible.
1.6
Paraclinical diagnostic criteria
Imaging studies (standard X-ray, scanner, MRI) of the spine, the hips and the pelvis facilitates elimination of differential PMS diagnoses.
Moreover, a pelvis MRI scan is necessary when attempting to detect on the affected side a possible hypertrophy of the piriformis muscle, which is a potential source of compression of the sciatic nerve .
In the context of a differential diagnosis, electroneuromyography (ENMG) allows for visualization of electrical signs in connection with a truncal injury of the sciatic or root nerve L5 or S1. As regards a PMS diagnosis, ENMG stimulo-detection involves study of the delayed F reflexes and H responses, which are sensitized by the FAIR test, and thereby facilitates apprehension of proximal nerve conduction .
The authors insist on long H-response latency, which appears on the pathological side. The latency response delay used with regard to a large-scale series is 1.8 ms .
1.7
Discussion
Clinical semiology of PMS is misleading, and a clinician runs the risk of erroneously focusing on spinal, coxal and sacroiliac pathologies. Subsequent to their elimination from clinical consideration and suitable supplementary examinations, PMS may be suggested in the early stages of truncated sciatica starting in the buttock. The normal results of biological examinations counteract any diagnosis of an inflammatory episode along the lines of rheumatoid arthritis or an infectious or neoplastic pathology.
A clinical picture consisting in unilateral gluteal pain associated on the same side with occasionally truncated sciatica developing in fits and starts and depending on positional factors is suggestive of PMS. It is necessary at this point to proceed to a rigorous clinical examination including oriented clinical testing.
The manoeuvres that have been reviewed are aimed at putting the piriformis muscle under stress in a variety of situations. Some of them appear more pertinent because they are particularly apt to reproduce the patient’s pain by precisely targeting the piriformis muscle. Confined in a deep region and in close proximity to other muscles acting similarly, the piriformis is difficult to mobilize. It consequently appears logical to associate reproduction of buttock pain by stretching manoeuvres, resisted contraction manoeuvres and palpation of the piriformis muscle with triggering of sciatic tingling in the symptomatic pelvic limb by prolonging the manoeuvres for several tens of seconds, if necessary.
Palpation is theoretically carried out at the end of the examination so as not to immediately reproduce the pain and thereby falsify the clinical tests.
The piriformis muscle is not only a stabilizer but also a hip extensor; as a result, hip flexion is a means of putting it under stress.
Since this muscle is a lateral rotator of the pelvic limb and the extended hip, it is legitimate to carry out medial rotation so as to put it under stress. Moreover, some studies have shown that pronounced homolateral hip flexion surpassing 90° modifies the moment arms of the muscle, which then becomes a medial rotator . The HCLK manoeuvre draws inspiration from this biomechanical consideration and allows the muscle to be stretched under the just-mentioned conditions of maximal flexion and lateral rotation of the hip. In the final position tested, the fibres constituting the sciatic nerve may be compressed against its resistant fascia covering.
That much said, it is difficult during a clinical examination to dissociate the piriformis muscle from one of its congeners, the internal obturator (lateral rotator of the hip); in fact, the two of them anatomically form a pincer muscle occasioning an alternating trajectory of the sciatic nerve as it crosses the infra-piriformis canal.
The nerve can then be compressed in the narrow muscle nexus located between the lower edge of the piriformis muscle and the internal obturator, gemelli and quadratus femoris muscles around which it is entwined .
Given these biomechanical considerations, we are convinced that it would be worthwhile to associate the Freiberg, FAIR and HCLK manoeuvres. While the first two stretch out the piriformis muscle in medial rotation, the third stretches it out in lateral rotation.
The PAMR manoeuvre does not seem sufficiently pertinent; while it puts the lateral rotator muscles under stress, it fails to rapidly reproduce pain; this is probably because the hip involved is not placed in flexion.
The sensitized HFD and Lasègue manoeuvres are indeed of interest on account of their sensitivity, which nonetheless remains to be assessed. However, given their positivity in situations involving nerve root impingement, their specificity is likely to remain mediocre.
Since the piriformis is one of the pelvi-trochanteric muscles, all of which are lateral rotators of the hip, isolated counteracted contraction of that muscle is hardly conceivable. The action specific to the piriformis muscle cannot be individualized within the muscle nexus. As a result, manoeuvres limited to counteracted contraction in abduction and lateral rotation, such as Pace and Nagle’s or Beatty’s, are useful but not sufficient. Our team has favoured the Beatty manoeuvre.
While there exists no “gold standard” paraclinical examination with regard to PMS, ENMG in stimulo-detection sensitized by the FAIR test is likely to yield interesting information. Published studies have highlighted the pertinence of delayed conduction of the H response with regard to the position of reference . However, the reduced amplitude of the responses obtained does not appear to be a decisive element. After all, the H reflex tests only the tibial component of the sciatic nerve. Just like the fibular component, which has yet to be sufficiently explored, it needs to be evaluated through observation of the F waves sensitized by the FAIR manoeuvres.
Present-day imagery with regard to PMS remains disappointing since it fails to accurately elucidate not only the relationships between the sciatic nerve and the piriformis muscle, but also the positional modifications of the infra-piriformic canal. With MRI, no significant “warning sign” has been detected in cases of PMS with regard to the piriformis muscle or the sciatic nerve.
1.8
Conclusion
Denial of the existence of the PMS is a consequence of the difficulty of its diagnosis, which is essentially clinical and not backed up by specific supplementary tests. From our standpoint, PMS represents an association of the muscle contraction of the piriformis with a positional truncal syndrome compressing the sciatic nerve.
With regard to the piriformis muscle, we have been systematically seeking out a symptomatic triad with passive stretching manoeuvres (Freiberg, FAIR and HCLK), one or more active manoeuvres of more or less resisted contraction (Beatty, Pace and Nagle or the FAIR test) and a palpation test around the piriformis muscle that typically reawakens the painful symptoms.
The clinical manoeuvres we have proposed should be prolonged, at times for several tens of seconds, in order to hopefully reproduce characteristic sciatic tingling.
Supplementary anatomical, clinical and image-based studies will be needed so as to better understand this entity.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
Le syndrome du muscle piriforme (SMP) est défini comme un syndrome canalaire par compression du nerf ischiatique par le muscle piriforme, entraînant une symptomatologie de souffrance tronculaire du nerf ischiatique à début fessier.
La première description en a été faite par Yeoman en 1928 . En 1934, Freiberg a reconnu des signes spécifiques à ce syndrome . Ce n’est qu’en 1947 que Robinson a nommé cette entité clinique « syndrome du pyramidal » .
Les éléments cliniques et paracliniques rapportés dans les descriptions sont parfois discordants et ont fait discuter sa réalité . Pourtant il s’agit d’une des rares causes de sciatalgies non rachidiennes consécutives à un véritable syndrome canalaire lors du passage du nerf ischiatique dans le canal infra-piriforme .
Les étiologies évoquées de la compression du nerf ischiatique sont diverses: inflammatoire, traumatique, tumorale ou malformative . Le plus fréquemment, l’origine de la compression est musculaire mettant en cause le muscle piriforme .
Dans ce travail, nous nous sommes intéressés au SMP d’origine musculaire.
Notre objectif à partir de l’étude anatomique du muscle piriforme est de tenter d’étayer des hypothèses physiopathologiques et ainsi de discuter les tests cliniques les plus pertinents pour le diagnostic.
2.2
Méthode
En se basant sur les descriptions anatomiques du muscle piriforme, des dissections ont été réalisées au laboratoire d’anatomie sur des cadavres embaumés (dons du corps) selon la préparation de Vinckler. La dissection a été faite classiquement plan par plan afin de mettre en évidence les rapports de la partie exopelvienne du muscle piriforme dans la fosse glutéale. Les différentes hypothèses physiopathologiques ont été issues de la revue de littérature effectuée à propos de ce syndrome, en y incluant des références biomécaniques et fonctionnelles.
Les tests cliniques ont été discutés à partir de la revue de la littérature et de notre expérience personnelle en se basant sur la biomécanique musculaire.
2.3
Anatomie
Le muscle piriforme est un muscle pair qui possède un corps musculaire triangulaire dont la base est insérée de chaque côté sur la face ventrale du sacrum au pourtour des 2 e et 3 e foramens sacraux.
Le muscle piriforme sort de la cavité pelvienne en glissant sous la grande incisure ischiatique de l’os coxal, au-dessus du ligament sacro-épineux. Il traverse ensuite obliquement vers le bas la région glutéale pour se terminer sur le bord supérieur du grand trochanter du fémur ( Fig. 1 ). Dans la région glutéale, il est placé sous le muscle grand fessier et au-dessus de la terminaison du muscle obturateur interne accompagnée des muscles jumeaux. Le muscle piriforme délimite ainsi deux zones de passages musculo-ligamentaires appelées foramens supra-piriforme et infra-piriforme. Les vaisseaux et nerfs glutéaux supérieurs passent le foramen supra-piriforme. Dans le canal infra-piriforme, cheminent le nerf ischiatique accompagné des nerfs pudendal et glutéal inférieur.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




