The Management of Complications Associated with Treatment of Posttraumatic Deformity of the Thoracolumbar Spine
Kern Singh
Alexander R. Vaccaro
Alberto Di Martino
Michael A. Pahl
INTRODUCTION
Failure to recognize the extent of bony and soft tissue disruption (and therefore instability) in spine injuries may result in inadequate stabilization of an unstable lesion. Despite better methods of spine fracture evaluation and treatment, late deformities are not uncommon, often resulting in pain and neurological compromise. These deformities can be difficult to manage and often require an extensive surgical correction with a high incidence of complications. The incidence of posttraumatic deformity in the setting of thoracolumbar spine injury is not specifically known. The vast majority of unstable spinal injuries are recognized early and managed with either prolonged immobilization or surgical stabilization. However, improperly immobilized unstable injury patterns may lead to long-term morbidity associated with chronic pain and potential neurological compromise. Management goals of posttraumatic deformity are correction of deformity, stabilization, decreasing pain, and improvement of neurological function. As in all settings of revision surgery—and in cases of surgical correction of primary posttraumatic deformities—the incidence of complications is often unavoidably high. The following chapter is an overview of the avoidance and management of complications associated with the treatment of posttraumatic thoracolumbar deformities.
EPIDEMIOLOGY
Though the incidence of thoracolumbar injuries in North America is relatively high (150,000 spine fractures per year), the majority require little or no treatment, and very few result in a progressive deformity (1). Thoracolumbar spine injuries occur in a bimodal distribution, with the first peak occurring in people in the second and third decades of life and the second peak occurring in the sixth decade of life (2,3). Treatment of these injuries has been associated with complications including neurologic deterioration
(1%), spinal instrument failure (2% to 8%), vascular injury, sexual dysfunction, deformity, chronic pain, and infection (3% to 10%) (2,3). The improvements in the acute management of patients who have sustained thoracolumbar spine injuries have, ironically, resulted in an increased incidence of posttraumatic deformity. This is due to both an increased survival rate in the setting of other associated significant injuries, in addition to the presence of a complete or incomplete neurologic injury resulting in unbalanced forces on the spinal axis (4).
(1%), spinal instrument failure (2% to 8%), vascular injury, sexual dysfunction, deformity, chronic pain, and infection (3% to 10%) (2,3). The improvements in the acute management of patients who have sustained thoracolumbar spine injuries have, ironically, resulted in an increased incidence of posttraumatic deformity. This is due to both an increased survival rate in the setting of other associated significant injuries, in addition to the presence of a complete or incomplete neurologic injury resulting in unbalanced forces on the spinal axis (4).
Clinical Presentation of Posttraumatic Deformity
Late spinal deformity is a description that encompasses a broad range of spinal deformities defined by their timing of presentation and magnitude of severity. Following an acute injury, the signs and symptoms associated with an unstable thoracolumbar fracture include persistent pain, worsening deformity due to mechanical instability, and possibly new onset or progressive neurologic deficit. Over time, if unbalanced forces due to normal or abnormal physiologic stresses are present on an unstable spinal axis, a progressive deformity may become clinically evident (5,6).
The most common presenting complaint of a posttraumatic deformity is a dull, aching pain at the apex of the deformity (7,8). Strenuous activity or prolonged sitting or standing generally aggravates the pain (9). Low back pain (radicular or nonradicular) is also a common complaint following a thoracolumbar fracture. Low back pain may be the result of altered muscular dynamics and fatigue due to a compensatory hyperlordosis secondary to thoracolumbar kyphosis at the fracture site or a sequelae of posttraumatic arthritis (10).
Local or referred pain, with or without signs of neurologic irritability, may become pronounced over time as a deformity progresses due to symptoms of sagittal imbalance and neural compromise. Nonoperative treatment regimens (rest, immobilization, bracing) may become ineffective, requiring the need for surgical intervention. Bohlman et al. demonstrated significant pain relief in 41 of 45 patients following late anterior decompression for chronic pain or paralysis after thoracolumbar injuries at an average of 4.5 years follow-up (11). Pain is rarely the sole criterion for surgical intervention, as the majority of patients also have radiographic evidence of deformity progression with or without a static or progressive neurologic deficit.
Malcolm et al. reported on 48 operatively treated patients with posttraumatic deformity, of which 13 (27%) had progressive neurologic deterioration due to spinal cord compression (9). Other causes of neurologic deterioration included the development of a posttraumatic syrinx or progressive posttraumatic cystic myelopathy (12,13).
Other causes of neurologic dysfunction may be tethering of the spinal cord or arachnoiditis. Treatment for cystic expansile lesions of the spinal cord has had limited success with cerebrospinal fluid shunting procedures resulting in a 50% rate of shunt revision (14). A nonprogressive spinal kyphotic deformity without evidence of cystic lesions of the spinal cord is also a rare cause of neurologic deterioration. Abel et al. reported on a group of 68 patients without evidence of spinal cord cystic degeneration, but with progressive neurologic deterioration in the setting of a posttraumatic deformity (2). They noted that the incidence of spinal cord cystic degeneration in patients with 15 degrees of kyphosis or less than 25% spinal canal stenosis was half that of patients with larger deformities. Neurologic deterioration was instead related to the presence of localized stenosis, instability, arachnoiditis, and spinal cord tethering.
Radiographic Evaluation
The radiographic evaluation of late thoracolumbar deformity begins with long-cassette, 36-inch, standing anteroposterior, and lateral x-rays to assess overall coronal and sagittal balance. Particular attention should be paid to the status of the posterior elements to evaluate for the presence of splaying of the spinous processes, which is frequently associated with insufficiency of the posterior ligamentous complex. Flexion-extension and lateral bending radiographs are also useful in assessing the flexibility of the spinal deformity. Comparison of these films to the immediate postinjury and follow-up films will help clearly document changes in spinal alignment over time (5).
Computed tomography is an excellent imaging modality to visualize specific bony anatomy, especially the posterior elements and the posterior wall of the vertebral body, which may be difficult to accurately evaluate on plain radiographs. Obtaining 1- to 3-mm axial cuts, along with sagittal and coronal reconstructions, allows for optimum evaluation of all bony landmarks. Computed tomography can also be combined with myelography to assess the status of the neural elements, especially in situations in which magnetic resonance imaging (MRI) cannot be used or is suboptimal, as in the postsurgical setting or in the presence of internal fixation.
As with any deformity correction, quantifying the degree of neural compression and the presence of intrinsic spinal cord or cauda equina pathology (myelomalacia, syrinx, arachnoiditis, tethering) is an essential step in preventing unexpected neurologic embarrassment during attempted deformity correction. MRI is most useful in evaluating the spinal cord and soft tissues surrounding the vertebral column. It allows the appreciation of subtle changes within the parenchyma of the spinal cord that may be indicative of edema, fluid collections, or scarring. Several authors have noted the prevalence of posttraumatic syringomyelia or progressive cystic myelopathy to be between 3.2% and 40% in spinal cord injury patients (15,16). It also allows for
the evaluation of the integrity of the posterior ligamentous complex, which is often attenuated in chronic posttraumatic deformities
the evaluation of the integrity of the posterior ligamentous complex, which is often attenuated in chronic posttraumatic deformities
BIOMECHANICS OF DEFORMITY
The majority of posttraumatic deformities of the thoracolumbar spine have malalignment of the spinal axis in more than one plane. A three-dimensional deformity involving the sagittal and/or coronal plane may also be associated with a translational and/or rotatory deformity. The majority of these deformities, however, are often characterized by a dominant planar deformity. Therefore, it is imperative that the treating physician fully appreciate the three-dimensional nature of all posttraumatic spinal deformities.
Deformity in the Sagittal Plane
Kyphotic Deformity
A focal posttraumatic kyphotic deformity is generally caused by a flexion- or compression-type injury (17,18,19). There is often a compensatory hyperextension of the adjacent spinal motion segments to correct for the altered sagittal alignment. Injuries such as an unstable burst fracture, flexion-compression injury or flexion-distraction injury are especially prone to posttraumatic deformity. This is especially true at the thoracolumbar junction, even in the setting of appropriate spinal immobilization (20,21,22,23). One of the most frequent operative approaches used in the treatment of significant kyphotic deformities is an anterior decompression and release with or without deformity correction, followed by a posterior segmental stabilization procedure with or without further deformity correction (Fig. 18.1).
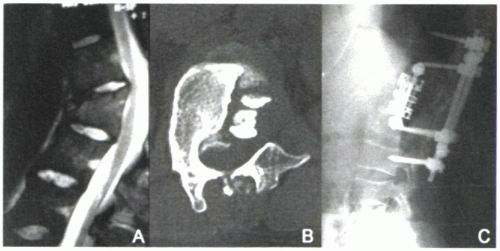 Figure 18.1 Sagittal MRI (A) and axial CT (B) of a traumatic T12 burst fracture with kyphotic deformity, which was treated with an inadequate, left-sided anterior approach and attempted T12 corpectomy. The majority of the T12 vertebral body and retropulsed bony fragments were left within the canal, causing severe compression of the conus medullaris (terminal spinal cord). A revision right-sided T12 corpectomy and fusion using an expandable cage and anterior internal fixation followed by a posterior stabilization procedure [(C) lateral plain radiograph] resulted in correction of the posttraumatic deformity. (Image courtesy of Kim Hammerberg, MD, Rush University Medical Center, Chicago, Illinois.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




