Elbow dislocations are common injuries in both the adult and pediatric populations. These injuries include simple dislocation with no associated fracture and more complex injuries with bony and ligamentous involvement. Simple dislocations are generally stable after reduction and managed with early mobilization. Complex dislocations are very unstable and operative intervention is usually necessary. Complication risks are greater and outcomes are less optimal with complex dislocations. A thorough knowledge of anatomy and understanding of the osseous and soft tissue mechanics is essential for proper management of these injuries.
Key points
- •
“Elbow instability” includes a wide variety of disorders from simple acute dislocations to complex dislocations with concomitant injuries to osseous and ligamentous structures.
- •
Simple dislocations are the most common and can usually be treated with closed reduction and early active motion to produce excellent outcomes.
- •
Complex elbow dislocations generally require surgical intervention to repair the soft tissue and associated fractures to yield stability and facilitate early active motion.
- •
Residual instability may require dynamic bracing or ligament reconstruction depending on the extent of ligamentous deficiency.
- •
Chronic elbow dislocations require open reduction and hinged external fixation versus static bridging temporary internal fixation to restore stability.
Acute and chronic elbow instability
The elbow is the second most commonly dislocated major joint in adults. It is also the most commonly dislocated major joint in the pediatric population, with dislocations accounting for 10% to 25% of all elbow injuries. The mean age is 30 years and it is more common in males.
Instability of the elbow can range from simple dislocation with no associated fractures to more complex patterns with varying degrees of bony and ligamentous injuries. Chronic instability can present with recurrent subluxation or dislocation owing to incompetence of the lateral ulnar collateral ligament (LUCL).
Understanding elbow instability requires a thorough knowledge of the articular elements, anatomy of the lateral collateral ligament complex, and the mechanism of elbow subluxation and dislocation.
Anatomy
The elbow is a trochoginglymoid joint with 2 principle arcs of motion: flexion–extension and pronation–supination. The ulnohumeral articulation contributes primarily to flexion–extension with pronation–supination occurring through the radiohumeral articulation. The elbow is not a true hinge and simulated motion studies suggest that there are 3° to 4° of potential varus and valgus laxity and axial laxity that may occur through the range of motion of the joint, but for practical purposes it can be considered to move as a uniaxial articulation, except at extremes of range. The axis of rotation passes through the center of the arcs formed by the sulcus of the trochlea and the capitellum.
The elbow is a highly congruent joint and thus has a high degree of inherent stability. The osseous anatomy of the distal humerus and proximal ulna provide most of the inherent stability of the elbow. This stability is based on both static and dynamic constraints. Static restraints are primarily the ulnohumeral articulation, the medial collateral ligament (MCL) and the lateral collateral ligament (LCL), specifically the ulnar part of the LCL. Other static restraints include the radial head, the common flexor and extensor origins, and the capsule.
The major determinant of stability, however, is the ulnohumeral joint, specifically the coronoid. The coronoid process, which consists of a tip, body, anterolateral facet, and anteromedial facet, acts as an anterior buttress, resisting the posteriorly directed forces from the triceps, brachioradialis, or the biceps acting at the elbow joint, resisting subluxation in both flexion and extension. Its role in preventing posteromedial rotatory instability of the elbow has also been described. Interlocking of the coronoid and olecranon processes provides added ulnohumeral stability at extremes of motion. Clinical evidence suggests that at least 50% of the coronoid must be present for the ulnohumeral joint to be functional. Absence of the radial head further and dramatically compromises the elbow with a 50% or greater coronoid deficiency. The radial head should not be removed from a dislocated elbow in which the coronoid is fractured, unless the coronoid and ligaments can be repaired reliably.
The radial head may contribute up to 30% of the stability of the elbow against a valgus stress, and up to 75% with disruption of the MCL complex, where it becomes the primary restraint to valgus stress.
Dynamic stabilizers include muscles crossing the elbow joint that produce compressive forces at the articulation. The muscles contributing most to this stability are the anconeus, triceps, and brachialis. The anconeus originates near the lateral epicondyle, has a broad, fan-shaped insertion on the ulna, and serves as a major dynamic stabilizer of the elbow, preventing posterolateral rotational displacement.
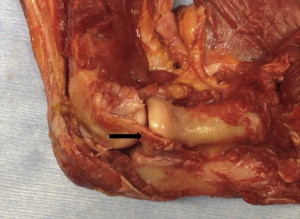
The medial collateral ligament and lateral collateral ligament complexes, in combination with the anterior capsule, the posterior capsule, and the ulnohumeral articulation, provide important static restraints to elbow instability. The medial collateral ligament is composed of the anterior oblique ligament, the posterior oblique ligament, and the transverse ligament. The strongest and most crucial structure of this segment is the anterior oblique ligament ( Fig. 1 ), because it is the primary restraint to applied valgus force in conjunction with the radial head. Studies have demonstrated that as long as there is an intact anterior oblique ligament, there is minimal change in joint stability, even in the absence of an incompetent radial head. In contrast, anterior oblique ligament release combined with excised radial head results in gross instability of the elbow joint.
The lateral collateral ligament complex consists of the radial collateral ligament, the LUCL, and the annular ligament. The radial collateral ligament originates from the lateral epicondyle and terminates by blending into the annular ligament. As a unit, it serves to stabilize the proximal radioulnar joint. The LUCL ( Fig. 2 ), originating from the lateral epicondyle, blends with the fibers from the annular ligament, but arches superficially and distal to it. The LUCL functions as the primary restraint to varus stress and is impaired in posterolateral rotatory instability of the joint.
The anterior capsule of the elbow is thin, but provides a significant stabilizing effect when it is taut in extension, although that decreases as the elbow approaches 90° of flexion. Anteriorly, the capsule attaches to the anterior region of the sigmoid notch as well as the proximal aspect of the olecranon fossa. This capsule has been found to commonly be torn in elbow dislocations.
The thin posterior capsule, composed mainly of transverse fibers, stretches across the olecranon fossae to form a transverse band. On the ulnar aspect of the elbow, the capsule forms the posterior portion of the annular ligament. The attachment of the posterior capsule to the triceps tendon prevents the capsule from getting caught during extension.
The muscles forming the medial complex of the elbow include the flexor carpi ulnaris, flexor carpi radialis, flexor digitorum superficialis, and pronator teres. Together, this group provides a support that is capable of resisting valgus forces. In comparison, the muscles forming the lateral complex of the elbow (extensor carpi ulnaris, extensor digitorum communis, extensor carpi radialis brevis, extensor carpi radialis longus, and anconeus) provide a reinforcement to resist varus forces. This has been found to be significant in cases of lateral collateral ligament deficiency. Together, the medial and lateral musculotendinous complexes contribute to a dynamic stability of the elbow as a result of compression of the joint surfaces against each other. As long as these remain constraints intact, namely the ulnohumeral articulation, lateral collateral ligament, and medial collateral ligament, the elbow will be stable.
Evaluation and Assessment
The most common types of elbow dislocations are those that occur posteriorly. Typically, dislocation refers to the displacement of the radius and ulna relative to the humerus. Some studies explain that dislocations occur most frequently occur as a result of a fall on an outstretched hand, whereas others describe them occurring most commonly from athletic injuries. Either way, instability can be classified by the direction of instability, the presence or absence of fractures (complex vs simple, respectively), and whether they are acute or chronic in nature.
First, however, assessment of elbow instability must be performed owing to the potential high-energy trauma typically associated with elbow dislocations. Obtaining the history should allow one to discern the mechanism of injury, severity of injury, and additional morbidities. After the life- and limb-threatening injuries have been treated, the physical examination should focus on the involved limb. The injured elbow should be assessed for deformities and presence of open injury. A dislocated elbow often appears with the forearm held in varus and supination. Before any manipulation, assessment of neurovascular status should be determined. In particular, entrapment of the brachial artery, median nerve, and ulnar nerve are of concern owing to their increased frequency of injury during manipulation. Associated injuries should be sought out with evaluation of the ipsilateral shoulder and wrist, along with the ipsilateral distal radial–ulnar joint and interosseous membrane. Localized swelling owing to soft tissue disruption is common, and may lead to constriction of the associated fascial compartments, resulting in increased intracompartmental pressures. As such, all patients presenting with an acute dislocation should be initially evaluated for the presence and development of compartment syndrome.
Simple Dislocation
Simple dislocations most commonly occur in a posterior and lateral manner without major fracture ( Fig. 3 ). Ten percent of cases, however, can have a minor avulsion near the epicondyles and/or coronoid process; however, they are not significant. Anterior dislocations, although uncommon, should remain in the differential diagnosis owing to their association with triceps disruption or olecranon fractures. It should also be noted that the even more rare divergent dislocation is typically associated with high-energy trauma. The mechanism of a posterior dislocation is typically a combination of valgus, supination, or external rotation of the forearm, causing an axial load through the elbow. The summation of these forces initiates a sequence of soft tissue injuries from the lateral to medial aspects of the elbow, leading to posterolateral rotation of the forearm relative to the humerus culminating in posterior dislocation of the proximal radius and ulna as the coronoid is displaced posteriorly in relation to the trochlea and can be clinically reproduced by a maneuver known as the “lateral pivot shift test,” which is discussed elsewhere in this article. The resulting tissue disruption has been classified into 3 stages.
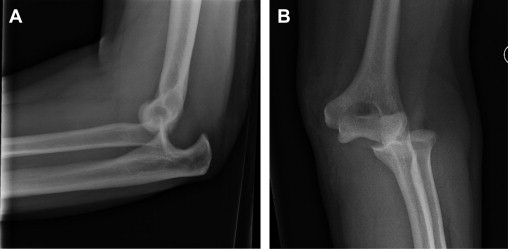
Stage 1 is characterized by partial or complete disruption of the lateral collateral ligament with complete disruption of the ulnar component. The resulting posterolateral subluxation may be reduced spontaneously. In the event of further anterior and posterior capsular disruption, a stage 2 dislocation may occur with the coronoid in a “perched” position on the humeral trochlea; in essence, the coronoid has not slipped behind the trochlea ( Fig. 4 ). This is also known as an incomplete subluxation, and is possible with disruption of the lateral collateral ligament with some maintenance of the medial collateral ligament. A stage 3 dislocation occurs after persistent force has been applied, disrupting the MCL and causing a posterior dislocation. This stage has been subdivided into parts. Stage 3A is characterized by disruption of all the soft tissues around to and including the posterior part of the medial collateral ligament. The anterior band of the medial collateral ligament is intact, allowing for posterior dislocation and pivoting of the elbow around the band. Reduction is completed by manipulation of the elbow while in supination and valgus, which mimics the deformity. In stage 3B , the entire medial collateral complex is disturbed; however, after reduction, valgus, varus, and rotatory instability are still present. Stage 3C is characterized by complete stripping of soft tissues around the distal humerus, resulting in an instability so severe that the elbow is capable of dislocation or subluxation, even in a cast set to flexion of 90°. The most effective reduction is maintained typically by flexion of the elbow past 90° to 110°. In addition to the ligamentous compromise in stage 3C dislocation, the origin of forearm flexor and pronator muscles (which are secondary dynamic stabilizers of the elbow) is compromised.

The primary objective of treatment for a simple dislocation is to provide a stable reduction that allows for early active range of motion. The reduction can be completed with or without sedation. The reduction is performed by flexing the elbow to approximately 25° while applying longitudinal traction combined with supination at the forearm and countertraction at the upper arm provided by an assistant. Valgus and varus instability should be assessed with the elbow in 30° of flexion and full extension. Initial management includes immobilization for approximately 2 to 3 weeks, followed by flexion and extension in a hinged splint for 4 weeks. Afterward, unrestricted flexion and extension may be allowed; however, care should be taken to avoid excessive valgus load. Development of a significant flexion contracture is uncommon in this injury.
After complete dislocations, some instability will be present, given that both medial and lateral ligaments have been disturbed. If dislocation occurs during extension, the elbow should be reassessed with the forearm in pronation. If this position proves to be more stable, a hinged brace should be applied with the forearm placed in pronation. It should be noted that, if greater than 45° of pronation are required to maintain the reduction, operative intervention is indicated.
In the event of surgery, a midline posterior approach is used, although medial and lateral approaches may also be used, depending on surgeon preference. A posterior approach allows for raising fasciocutaneous flaps enabling circumferential access, as well as minimal disruption of local cutaneous nerves. In contrast with lateral and medial incision sites, fewer cutaneous nerves cross in the posterior midline. It is absolutely critical that the ulnar nerve be identified and protected, and transposed anteriorly if necessary. This is standard during any repair procedures involving the medial compartment of the elbow. Complete dislocations almost always include disruption of the medial collateral ligament complex, sometimes even avulsing the overlying flexor–pronator muscular structures. On the opposite side, avulsion of the common extensor origin on the lateral epicondyle can aid in exposing the lateral collateral ligament complex. In both cases, the ligamentous complexes can be repaired with large, braided, nonabsorbable sutures, suture anchors, bone tunnels, or in certain chronic situations autogenous tendon grafts. After surgery, the stability of the elbow must be assessed. If instability persists, a hinged external fixator with skeletal fixation should be applied. This can ensure joint range of motion with maintenance of joint reduction. If the joint is stable after surgery, a hinged brace with our without an extension block can be used for 4 to 6 weeks. In addition to a supervised range-of-motion program, follow-up radiographs should be obtained to ensure that the joint is maintained in appropriate reduction.
Complex Fracture–Dislocation
Appropriately termed the “terrible triad,” the combination of ligamentous injury with coronoid and radial head fractures ( Fig. 5 ) has been found to have a high complication rate. The most effective method to stabilize these injuries requires surgical intervention to allow for return to early motion. Closed reduction often results in redislocation, which may risk further damage. This type of injury can be appropriately assessed with 3-dimensional CT reconstructions to help address each component of the injury. Goals of surgery include restoration of the anterior bony buttress, which consists of the coronoid process and radial head, and repair of the medial collateral ligament and the LUCL. Even small coronoid fractures should be repaired, if possible, because the repair adds an additional reinforcement against dislocation and restoration of function of the anterior capsule. The coronoid can be secured with a combination of suture fixation and/or screw fixation. After repair or replacement of the radial head, the radial extensor mass and lateral collateral ligament can be reattached to the lateral condyle of the humerus ( Fig. 6 ). This is immediately followed by an assessment of stability through a full range of motion. If there is redislocation during elbow extension before reaching 30° to 40° from full extension, it may be necessary to repair the medial collateral ligament and apply a hinged external fixator. If redislocation occurs before the elbow approaches full extension, it will likely also be unstable in a cast or splint.
Chronic Posterolateral Rotatory Instability
Although many structures are disrupted in an elbow dislocation, chronic instability is primarily owing to a deficiency in the lateral collateral ligament resulting in posterolateral rotatory instability. Some studies have reported that nearly one-third of patients with a simple dislocation of the elbow treated by closed reduction had long-term symptoms of instability. Often, these patients present with a history of persistent, recurring pain, and clicking, catching, or subluxation within the range of motion. Patients generally recall 1 episode of trauma that may or may not have resulted in a dislocation, or sometimes even iatrogenic cause, such as an excessively lateral surgical approach as in the release of lateral epicondylitis, can result in posterolateral instability.
Range of motion in these patients is usually pain free, with negative valgus and varus stress testing. The “lateral pivot shift test” is the most sensitive test for clinical diagnosis of posterolateral rotatory instability, and is often performed under general anesthesia ( Fig. 7 ). To recreate the mechanism of instability, the patient lays supine on the examination table and has the involved arm overhead with the shoulder in external rotation. Next, the elbow is placed in extension with the forearm in supination while a valgus load is simultaneously applied. The elbow is then slowly brought from extension into flexion, and the radial head is felt to slip back in place. The test is positive if a visible or palpable clunk is elicited. Even simpler, the patient can be asked to push up from a chair with their forearms in supination. If pain or instability is felt as the elbow proceeds to extension, the test is positive. Another test known as the posterolateral rotatory drawer test has the elbow placed in 40° to 90° of flexion while applying an anteroposterior force on the radius and ulna. This is done to subluxate the forearm away from the humerus on the lateral side. The test is considered positive if subluxation or apprehension is elicited.

Generally, plain radiographs are normal, but sometimes can show avulsion from the lateral epicondyle or widening and/or incongruency of the joint space between the radius and capitellum. Stress radiographs or fluoroscopy can also be useful. When the lateral pivot shift test is performed, the elbow is placed in maximal rotatory subluxation and the ulnohumeral joint space is seen to be widened on lateral and anteroposterior views. Additionally, the lateral view can show posterior subluxation of the radial head. If necessary, MR arthrography and diagnostic elbow arthroscopy can be used to visualize damage to the LCL complex and radial head subluxation, respectively.
Generally, patients with less severe symptoms can be managed with extensor strengthening exercises or athletic neoprene sleeves, whereas patients with more severe symptoms and signs of chronic instability require surgery. Patients requiring an operation often need reconstruction of the LUCL, usually with an autograft or allograft tendon. Various operative techniques successfully using different tendon graft sites have been investigated in the literature, including the palmaris longus, plantaris, gracilis, and semitendinosus.
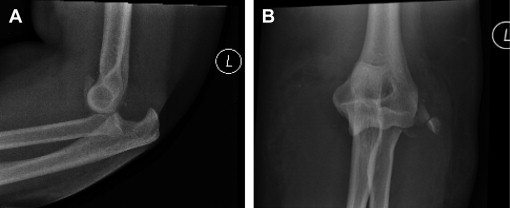
Chronic Elbow Dislocation
A chronic elbow dislocation is a disabling condition associated with severe limitation of elbow function and often significant pain. Neglected elbow dislocations or inadequate assessment after an attempted reduction can lead to a chronic dislocation of the elbow. Arthritic changes occur rapidly if the elbow is not reduced. Radiographs can readily make the diagnosis ( Fig. 8 ); however, CT evaluation should be considered to help with surgical planning. The goals of treatment can be conflicting, because it involves restoring both a stable concentric joint while also facilitating early motion within a satisfactory arc of motion. In the younger population, treatment options vary depending on the degree of posttraumatic arthritis present. If there is mild to moderate arthritis, then open reduction, reconstruction of medial and lateral collateral ligaments, and placement of a hinged external fixator is an option. There is a risk of redislocation, even with hinged external fixation ( Fig. 9 ), and a temporary internal plate may be needed to keep the joint concentrically reduced albeit at the expense of total joint motion ( Fig. 10 ). If there is more severe arthritis, distraction interpositional arthroplasty, or joint fusion may be considered. In the older age group, total elbow arthroplasty is also a good potential option.







