Abstract
Objectives
To present a comprehensive approach to the assessment of the severity of the autonomic lesion in spinal cord injury (SCI) patients, with regard to the level of lesion. To discuss how to assess an isolated sympathetic spinal cord that has lost supraspinal control (sympathetically complete lesion).
Method
PubMed was searched for articles related to cardiovascular (mainly cold pressor test, respiratory and postural challenges) and sudomotor (sympathetic skin responses) tests that have been used. The results of these evaluations are analysed with regard to the site of stimulation (above or below the lesion) according to three types of SCI that offer typical autonomic reactions (tetraplegics, paraplegics at T6 and at T10).
Results
Non-invasive cardiovascular and sudomotor testing allows the assessment of the isolated sympathetic spinal cord in SCI patients. Typical responses are found in relation with the level of the sympathetic lesion. Its definition would allow comparison with the somatic motor and sensory level of lesion of SCI patients and provide additional aid to the classification of those patients.
Conclusion
For research purposes on the integrity of the spinal sympathetic pathways, a battery of test approach is probably needed, using a combination of stimuli above and below the lesion, evaluating both cardiovascular and sudomotor pathways.
Résumé
Objectifs
Effectuer une revue des méthodes d’évaluation non invasives du système nerveux autonome du blessé médullaire. Présenter les résultats en termes de niveau lésionnel somatique et orthosympathique et de sévérité de l’atteinte végétative.
Méthode
Revue de la littérature (PubMed) des études sur les tests cardiovasculaires (principalement test au froid, tests posturaux et respiratoires) et sudomoteurs (réponses cutanées sympathiques) chez le blessé médullaire. Présentation des résultats en fonction du site de stimulation (sus- ou sous-lésionnelle) chez trois catégories de blessés médullaires (tétraplégique, paraplégique T6 et T10) aux réactions végétatives caractéristiques.
Résultats et conclusion
Les évaluations non invasives permettent l’évaluation de l’intégrité des voies orthosympathique du blessé médullaire. En cas de lésion sévère, la déconnection de la moelle orthosympathique du contrôle supraspinal peut être totale, isolant la moelle orthosympathique (atteinte orthosympathique complète). Des réponses orthosympathiques spécifiques sont retrouvées en fonction du niveau lésionnel. En association avec le niveau lésionnel somatique, la définition d’un niveau lésionnel orthosympathique affine la classification clinique des blessés médullaires. L’utilisation d’une batterie de tests associant stimulations sus- et sous-lésionnelles et évaluant les voies cholinergiques et adrénergiques est souhaitable si l’on veut explorer l’intégrité du système nerveux orthosympathique.
1
English version
1.1
Introduction
There is increasing evidence that attempts should be made to include the autonomic assessment in the management of spinal cord injury (SCI) individuals . To this purpose, definitions and classifications have recently been developed to document remaining autonomic functions after SCI , but definitions related to the severity of the autonomic lesion are still lacking. The terms “isolated spinal cord” or “complete sympathetic lesion” have sometimes been used to characterise a total loss of supraspinal control on the sympathetic nervous system below the level of lesion. As autonomic disturbances are related to the level of lesion, a sympathetic level of lesion can be defined in such cases .
Autonomic testing has been widely described in autonomic diseases, but sparsely in SCI patients. Cardiovascular and/or sudomotor challenges are most used, as they are non-invasive and standardised procedures. Their systematic use in SCI patients would help clinicians evaluate the severity of the autonomic lesion, its spontaneous evolution with time, and its implication on the clinical presentation of each patient (general, cardiovascular and respiratory autonomic functions, lower urinary tract, bowel and sexual functions) . This autonomic assessment could probably help us understand different clinical features in SCI patients that are still puzzling. For instance, why is it that some patients with a complete somatic lesion above T6 develop slight (or no) increase in blood pressure (BP) following bladder or rectal distension, while others will present severe autonomic dysreflexia (AD) following the same degree of stimulation? Why is it that some SCI patients present with ejaculation without medical assistance, while most don’t? Relations with other clinical aspects of the SCI such as pain or osteogenesis should also be considered.
The autonomic nervous system commonly is subdivided into two major parts: the sympathetic and parasympathetic components. Most of the visceral organs are innervated by both components of the autonomic nervous system :
- •
parasympathetic preganglionic neurons are located within the brain stem and within the sacral spinal segments (S2–S4). Parasympathetic control of the cardiovascular system is through the vagus nerve (X). There is no parasympathetic innervation of the peripheral vasculature except in the pelvic organs;
- •
the sympathetic column is located in the thoracolumbar (T1–L2) spinal cord segments. The target organs include the heart, blood vessels, respiratory tract, sweat glands, sexual organs and smooth muscles within the gut and bladder. Two different sympathetic pathways with specific postganglionic neurotransmitters are considered: the adrenergic pathway to the heart and blood vessels (noradrenaline) and the cholinergic pathway to the sweat glands (acetylcholine).
The activation of the sympathetic nervous system can be performed in different ways that generally include postural and respiratory challenges, as well as pressor and sudomotor tests.
1.1.1
Respiratory and postural challenges
Postural and respiratory challenges create conditions in which the sympathetic nervous system is stimulated to maintain BP homeostasis. The postural challenges (head-up, sit-up tests) and the Valsalva manoeuvre (VM) are reproducible tests of both cardiovagal (heart rate [HR], sinus arrhythmia) and adrenergic (beat-to-beat BP responses) function. In normal subjects, head-up tilt results in minimal changes in BP. There is normally a small to moderate rise in HR during postural change . During the VM, normally, with the rise in intrathoracic pressure the venous return falls along with BP. On releasing intrathoracic pressure there is a BP overshoot because of persistent sympathetic activity. Baroreflex activation then results in a secondary fall in HR to below basal levels .
1.1.2
Pressor tests
Pressor stimuli stimulate the sympathetic efferent pathways in a variety of ways. In a normal individual, these stimuli raise BP and HR, through peripheral vasoconstriction and rise in total peripheral resistance (TPR), and induce sweating . When cutaneous, muscular or visceral receptors are stimulated in the periphery, their afferents travel the spinal cord to the central nervous system (mainly in the hypothalamus and medullary vasomotor centre). When cerebral stimuli are used, such as a sudden sound or mental arithmetic, there is a direct transmission to these higher structures. In both cases, the efferent outflow is mediated by sympathetic nerves to the heart and peripheral blood vessels .
1.1.3
Sudomotor function
Sudomotor function can be assessed by several techniques, e.g. thermoregulatory sweating, quantitative sudomotor axon reflex test (QSART) and sympathetic skin responses (SSR). Thermoregulatory sweat test using quinizarin was described by Guttmann in 1947, requires special facilities, and has not been used in SCI since then . QSART that consists of an axon reflex mediated by the postganglionic sympathetic sudomotor axons has only been studied once in SCI patients . SSR is a simple, quick and reliable test and can be easily carried out in patients with myelopathies of diverse nature in any electrodiagnostic laboratory .
1.1.4
Bedside assessments
Bedside assessments have, so far, little clinical application, except for the skin axon reflex vasodilatation (SkARV) test . The spoon test for assessing sweating , the observation of piloerection , and the pupillary reflex dilation in response to a noxious stimulus of the upper thoracic dermatomes may need reappraising.
1.2
Methods
PubMed was searched for articles related to cardiovascular and sudomotor tests that have been used in SCI patients. The search strategies combined terms for “spinal cord injury” and “autonomic testing”, respectively “spinal cord injury OR tetraplegia OR quadriplegia OR paraplegia” and “cold pressor test OR Valsalva manoeuvre OR postural challenge OR respiratory challenge OR tilt test OR sympathetic skin responses OR sweating”. The main author screened all titles and abstracts identified and acquired the full-text publication of all potentially eligible studies. The bibliographies of all retrieved studies were screened for additional relevant articles.
To be eligible, studies had to:
- •
provide detailed descriptions of the neurological status of the individuals, in particular the level and severity of the lesion;
- •
give a comprehensive description of the tests used;
- •
give full cardiovascular (BP and HR) and sudomotor (hand or foot skin responses) data for each individual;
- •
be published in English.
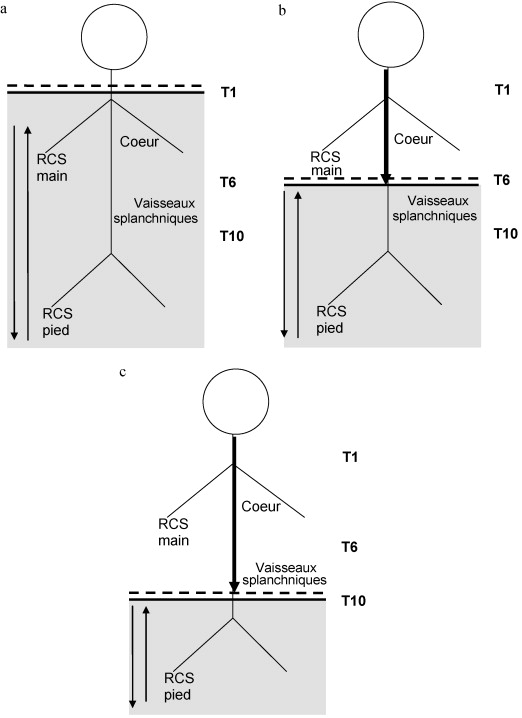
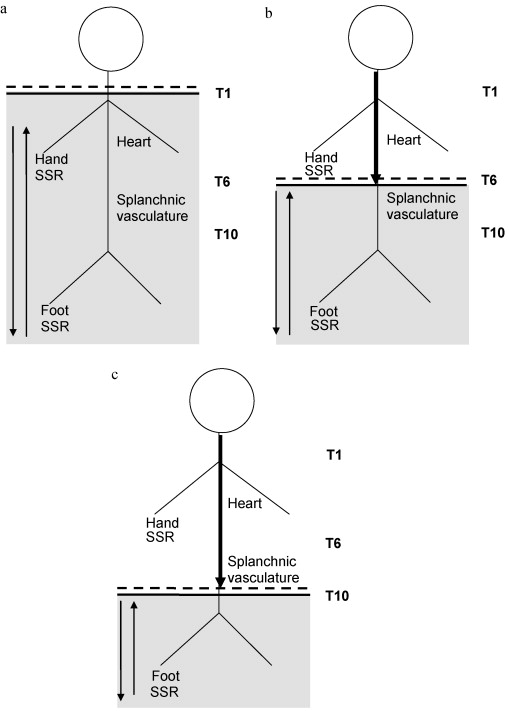
For the sake of the comprehension, we will consider three types of SCI that offer typical autonomic reactions (tetraplegics, paraplegics at T6 and at T10), as the severity of the sympathetic spinal cord lesion is dependent on the level of injury. The T1–T5 and T5–T10 sympathetic outflows project respectively to the heart and to the large splanchnic circulatory bed, and are directly implicated in the cardiovascular control (AD, orthostatic hypotension), whereas the T10–L2 sympathetic outflows is involved in sphincteric functions (lower urinary tract, anorectal and sexual functions).
1.3
Results
The descriptions below largely relate to the chronic stage in complete SCI patients (ASIA Impairment Scale [AIS] A), unless specifically stated.
1.3.1
Tetraplegic patients
In complete tetraplegics, the sympathetic column is totally disconnected from cerebral control ( Fig. 1 a ) . Conversely, all somatic and visceral afferents coming from below the lesion (starting from T1–T2 dermatomes) can reflexively activate the whole sympathetic column.
1.3.1.1
Stimuli above the lesion
Pressor stimuli that either originate in, or are modulated by, the brain (either cerebral or cervical afferents) will have no effect . Corbett et al. found no change in HR and BP following cutaneous (pinprick and forehead cold) or cerebral (mental arithmetic or noise) stimuli above the lesion . Stimulation above the lesion is not accompanied by changes of the peripheral resistance of the leg or vasoconstriction in the calf , of electrodermal activity , or of skin vasomotor reflexes .
However, three studies report conflicting results, with either a small increase in HR following extrinsic stimuli , or an increase in both HR and BP during mental arithmetic or cold hand test . They were observed in a total of 13 tetraplegic patients (nine complete AIS A and four AIS B).
Following stimulation of the median or the supraorbital nerves, the SSR will be absent in the hands and feet .
1.3.1.2
Postural and respiratory challenges
During head-up tilt, there is usually an immediate fall in both systolic and diastolic BP due to the lack of rise in TPR . The pressure may fall to extremely low levels. There is often a rapid rise in HR, which is inversely related to the fall in BP. This is likely to be due to withdrawal of vagal tone in response to unloading of baroreceptor afferents . The HR increase, however, is attenuated and does not usually rise above 110 beats per minute . These individuals fail to increase plasma catecholamine levels in response to these orthostatic challenges .
If tilt is prolonged, the BP tends to partly recover, often with oscillations. This recovery may be related to activation of the renin–angiotensin–aldosterone system or to the activation of spinal reflexes either from stimulation of the skin, the skeletal muscles, or the viscera (see Mathias and Frankel and Claydon and Krassioukov for review). Local myogenic reflex activity plays a pivotal role in peripheral vascular responses upon head-up tilt when central control mechanisms fail . The sit-up manoeuvre is sometimes performed and is better tolerated with lower fall in BP , so that it can be performed in the acute phase .
Similar cardiovascular findings are observed during a static maximum inspiratory breath-hold or the VM . After the VM, the BP overshoot relative to baseline is absent .
1.3.1.3
Stimuli below the lesion
Pressor stimuli below the lesion will activate sympathetic reflex along the isolated spinal cord that can result in AD. AD is a constellation of signs and/or symptoms in SCI at and above T6 in response to noxious or non-noxious stimuli below the level of injury defined by an increase in systolic BP (≥20 mmHg above baseline), and which may include one of the following symptoms: headache, flushing and sweating above the level of the lesion, vasoconstriction below the level of the lesion and dysrhythmias . As some cases of severe morbidity (including cerebral haemorrhage, seizures and pulmonary oedema) have been associated with AD , these tests should be performed with caution and by a trained medical team.
The HR may rise transiently with the elevation in BP or remain unchanged , presumably because of sympathetic stimulation of the heart as a result of spinal cardiac reflexes . There is usually a subsequent fall in HR because of stimulation of sinoaortic baroreceptors and increased vagal efferent activity . This may help dampen the rise in BP during AD, the bradycardia being usually related to the intensity of AD .
During AD, there is a reduction in leg blood flow and an increase in skin vasoconstriction , an activation of electrodermal activity of the extremities and of the face , a rise in legs and arms occluded venous pressure, indicating contractions of capacitance vessels , and an elevation of both stroke volume and cardiac output, suggestive of activation of spinal cardiac reflexes . The remarkable increase in arm muscle blood flow, flushing of the head, and nasal obstruction (Guttmann’s sign) remain puzzling. These signs are only seen in areas in which the somatic sensory nerve supply is intact, and occurs in spite of the fact that the sympathetic supply arises from the isolated cord .
Cold applied to the foot , pinprick of the costal margin , transcutaneous electrical stimulation to the arch of the foot , inflation of a pressure cuff to 220 mmHg on the leg induced mild AD. The abdominal wall seems particularly sensitive to stimulation, with moderate to severe AD following bladder tapping (even without bladder contraction) , cold or electrical stimulation on the T10–T11 dermatomes under the umbilicus . The most severe AD are usually found with vibromassage and ejaculation or bladder contraction in close relation to the peak of the detrusor pressure .
1.3.2
Paraplegic at T6
In T6 paraplegics, there is a normal or near normal supraspinal control on the sympathetic innervation of the heart, lungs and upper limbs ( Fig. 1 b). The isolated spinal cord controls the splanchnic vasculature and the lower limbs .
1.3.2.1
Stimuli above the lesion
Pressor stimuli above the lesion will elevate the HR, generally with a slight rise in BP and skin vasoconstriction . This response is not accompanied by changes below the lesion of the peripheral resistance of the leg , of electrodermal activity or skin vasomotor reflexes .
Following stimulation of the median nerve, the SSR will be absent in the feet (see discussion below). The palmar SSR can be elicited if the T4–T5 spinal cord segment is located above the lesion level .
1.3.2.2
Postural and respiratory challenges
During postural and respiratory challenges, there is usually an initial fall in BP, similar to tetraplegics, but followed by a more pronounced rise in HR that can partially compensate for the fall in BP . However a recent study suggests that, although cardiac autonomic control is intact, there is a blunted sympathetic response to head-up tilt .
During the VM, the BP initially decreases but then remains stable in paraplegics. However, at the end of the VM, the shortfall in BP relative to the baseline is similar in tetraplegics and paraplegics. After the VM, the BP overshoot relative to baseline is observed but significantly smaller in paraplegics than in controls . These findings may indicate that rate and magnitude of BP recovery, and the shortfall in BP relative to baseline at the end of the VM are mainly related to peripheral sympathetic activity to the vessels (absent in tetraplegics and T6 paraplegics), whereas the BP overshoot after the VM is primarily related to cardiac sympathetic activity (intact in T6 paraplegics) .
1.3.2.3
Stimuli below the lesion
As stated earlier, all patients with a lesion above T6 are prone to AD. However, the rise in BP is less severe in these patients than in tetraplegics . It is clear that increased blood flow in the fingers and in the forearm of these T6 paraplegics while the BP rises only slightly, can be regarded as compensatory vasodilatation initiated by the carotid sinus. The large changes in forearm flow also suggest that muscle blood flow is affected by BP regulating mechanisms in these patients, perhaps to a greater extent than it is in normal subjects .
1.3.3
Paraplegic at T10
In low paraplegics at (or below) T10, there is a normal or near normal supraspinal control on the entire sympathetic column ( Fig. 1 c) .
1.3.3.1
Stimuli above the lesion
A normal rise in BP and HR is expected in this group. Near normal vasomotor reflexes on upper and lower limbs have been described following a variety of pressor stimuli .
On median nerve stimulation, plantar SSR are rarely found in T10–T12 patients, but more consistently found with lesion below T12 .
1.3.3.2
Postural and respiratory challenges
Depending upon the level of lesion, i.e. partial or total preservation of the sympathetic outflow to the splanchnic vessels and the legs, near normal or normal cardiovascular responses are expected. During the sit-up manoeuvre, no HR or BP differences were found between a group of low paraplegics (T5–L4, with 20 AIS A and 13 AIS B–D patients) and controls .
1.3.3.3
Stimuli below the lesion
These patients are less at risk of AD, though sporadic cases have been reported . During penile vibratory stimulation, a significant rise in BP can be observed in these patients as well .
Pudendal nerve stimulation failed to elicit plantar SSR in patients with complete lumbar lesions .
1.3.4
Summary
It has been proposed that the term “complete” sympathetic lesion should only be used when the lowest part of the sympathetic spinal cord is isolated from supraspinal control . An isolated sympathetic spinal cord (or “complete” sympathetic lesion) can be assessed in two complementary ways ( Table 1 ):
- •
following stimulation above the lesion , there is a total absence of any sympathetic sudomotor or cardiovascular responses below the lesion in tetraplegic patients as the sympathetic column is totally disconnected from supraspinal control ( Fig. 1 a). In paraplegic patients at T6, normal heart control and sudomotor function of the upper limbs are expected, with normal rise in HR but no rise in BP following mental arithmetic or cold hand, and normal hand SSR ( Fig. 1 b). In paraplegic patients at T10, (near) normal cardiovascular responses are expected, whereas feet SSR will be absent ( Fig. 1 c);
- •
stimulations below the lesion will trigger AD in SCI patients with a lesion at or above T6. The presence of AD and compensatory bradycardia reflects the absence of supraspinal control on the splanchnic vascular bed.
| Normal responses | Tetraplegic | T6 paraplegic | T10 paraplegic | |
|---|---|---|---|---|
| Pressor stimuli above lesion | ||||
| HR | Significant rise | Absent response | Normal response | Normal response |
| BP and TPR | Significant rise | Absent response | Absent response | Near normal responses |
| Pressor stimuli below lesion | ||||
| HR | – | Bradycardia | Bradycardia | Normal response |
| BP and TPR | – | Autonomic dysreflexia | Autonomic dysreflexia | Normal response |
| Valsalva manoeuvre | ||||
| HR and BP | Maintaining or rise in BP after slight initial fall, with rise in HR; BP overshoot with fall in HR after the VM | Continuous fall in BP, not compensate for by a moderate rise in HR; absence of BP overshoot after the VM | Response similar to tetraplegic, but presence of BP overshoot after the VM | Near normal responses |
| TPR | Significant rise | Absent response | Absent response | Near normal responses |
| SSR | ||||
| Hand | Present response | Absent response | Normal response | Normal response |
| Foot | Present response | Absent response | Absent response | Absent response |
1.4
Assessment of the integrity of the sympathetic nervous system in SCI patients
1.4.1
Severity of the sympathetic lesion
Very few studies have focused on the integrity (i.e. completeness or incompleteness) of the sympathetic spinal cord lesion. For most authors, the presence of hands or feet SSR in tetraplegic or feet SSR in paraplegic patients above T6 in response to a stimulus above the lesion is indicative of an incomplete sympathetic lesion . For Baliga et al., a positive pressor response to mental arithmetic and hand cutaneous cold along with the lack of postural hypotension confirm a functionally competent sympathetic outflow in paraplegics below T10 . In paraplegics, the lack of vasoconstriction in the calf during the hand cold pressor test indicates a lack of supraspinal control of sympathetic outflow to the leg vasculature . In tetraplegics, the absence of vasoconstriction of the skin of the hand following a sudden loud noise, pinpricks on the face and neck, or ice applied to the same region test of the completeness of the lesion .
1.4.2
Clinical correlates
1.4.2.1
ASIA Impairment Scale (AIS)
Using supralesion stimuli, SSR are absent in hands and feet of most patients presenting with a complete (AIS A) somatic lesion above T3 or T6 . When studying data from several studies in patients with complete somatic AIS A lesions, it was shown that feet SSR on stimulation above the lesion were absent in 94% of the tetraplegic and 92% of paraplegic patients above T10 . An excellent correspondence between complete somatic (AIS A) and complete sympathetic lesions (100% of paraplegic and 94% of tetraplegic patients) was also found using SkARV test . These results show that an isolated sympathetic spinal cord is very often associated with a complete somatic (AIS A) lesion.
On the other hand, SSR were not reliably predicted by ASIA scale when SSR were provoked by electrical stimulation below the lesion, or when hands SSR are taken into account .
1.4.2.2
Clinical findings
A good relation is found between absence of SSR potentials and presence of AD , symptoms of orthostatic hypotension , cardiovascular response to exercise , absence of psychogenic erection .
1.5
Conclusion
Non-invasive cardiovascular and sudomotor testing allows the assessment of an isolated sympathetic spinal cord in SCI patients. Typical responses are found in relation with the level of the sympathetic lesion. The assessment of sympathetic levels of lesions at T10 and T6 in particular has significant clinical relation, such as cardiovascular control and sphincteric functions. Its definition would allow comparison with the somatic motor and sensory level of lesion of SCI patients and provide additional aid to the classification of those patients.
Recording SSR potentials is most used in SCI patients: it is a simple, non-invasive and reproducible test, but it only assesses the cholinergic sympathetic pathways. Bedside assessments such as SkARV test can give valuable information but have limitations. For research purposes on the integrity of the spinal sympathetic pathways, a battery of test approach is probably needed, using a combination of stimuli above and below the lesion, evaluating both cardiovascular and sudomotor pathways.
Conflict of interest statement
None.
2
Version française
2.1
Introduction
L’évaluation du système nerveux autonome (SNA) du blessé médullaire (BM) suscite un intérêt grandissant . Récemment, de nouvelles définitions et classifications de l’atteinte du SNA ont été proposées par un groupe d’experts, qui suggèrent que cette évaluation soit réalisée de façon régulière . Malheureusement, ce document ne contient aucune définition relative à la sévérité de l’atteinte végétative. Les termes de moelle orthosympathique isolée ou de lésion orthosympathique complète ont été utilisés pour décrire la perte totale du contrôle supraspinal sur les centres nerveux orthosympathiques sous le niveau lésionnel. Dans certains cas, un niveau lésionnel orthosympathique peut être défini .
L’évaluation du SNA est proposée pour le diagnostic de maladies du SNA. À cet effet, des explorations cardiovasculaires ou sudomotrices sont généralement réalisées, car non invasives et standardisées. Ces procédures sont pour l’heure très peu utilisées chez le BM. Leur utilisation systématique permettrait cependant d’évaluer la sévérité de l’atteinte végétative, son évolution spontanée avec le temps, et son importance dans la présentation clinique de chaque patient, sur le plan général, cardiovasculaire et respiratoire, et des fonctions sphinctériennes (bas appareil urinaire, sexuelle et anorectale) . Une meilleure connaissance du SNA devrait nous aider à comprendre des tableaux cliniques qui restent toujours intrigants. Pourquoi, à niveau lésionnel somatique similaire, retrouve-t-on des discordances en termes d’hyperréflexie autonome (HRA), de dyssynergie vessie-col ou d’éjaculation ? Le SNA pourrait également avoir une importance dans les tableaux douloureux et l’ostéogenèse.
Le SNA est constitué des systèmes orthosympathique et parasympathique. La plupart des organes possèdent une double innervation orthosympathique et parasympathique :
- •
les neurones parasympathiques préganglionnaires sont situés dans deux centres intra-axiaux, l’un dans le tronc cérébral et l’autre au niveau de la moelle sacrée (S2–S4). Le contrôle parasympathique du système cardiovasculaire s’effectue via le nerf X (vague ou pneumogastrique). Le système parasympathique n’exerce pas de contrôle sur la vascularisation périphérique, à l’exception des organes pelviens;
- •
le système orthosympathique se caractérise par la topographie exclusivement médullaire des centres intra-axiaux occupant la colonne inter-médiolatérale de T1 à L2. Il innerve le cœur, les vaisseaux sanguins, le système respiratoire, les glandes sudoripares, les organes sexuels et les muscles sphinctériens lisses au niveau de la vessie et des intestins. On distingue deux voies orthosympathiques possédant des neurotransmetteurs spécifiques : la voie adrénergique pour le cœur et les vaisseaux sanguins (noradrénaline) et la voie cholinergique pour les glandes sudoripares (acétylcholine).
L’activation du système orthosympathique peut se faire de différentes façons, qui font généralement appel à des stimulations posturales et respiratoires, à des stress ( pressor tests ) ou des tests sudomoteurs.
2.1.1
Tests posturaux et respiratoires
Lors de tests posturaux et respiratoires, le système orthosympathique est stimulé pour maintenir l’homéostasie cardiovasculaire et la tension artérielle (TA). Les challenges posturaux (verticalisation) et respiratoires comme la manœuvre de Valsalva sont des tests reproductibles et standardisés de la fonction parasympathique cardiovagale (nœud sinusal, fréquence cardiaque [FC]) et orthosympathique adrénergique (variations à court terme de la TA). Chez le sujet normal, la verticalisation engendre des modifications minimes de la TA, compensées par une tachycardie . Le Valsalva produit une augmentation de la pression intrathoracique, qui entraîne une baisse du retour veineux et de la TA. À l’arrêt de la manœuvre, on observe une augmentation réactionnelle de la TA ( overshoot ) lié à la persistance de l’activité orthosympathique. La mise en route du baroréflexe sinocarotidien engendre une baisse secondaire de la (FC) .
2.1.2
Les stress ( pressor tests )
Les stress ( pressor tests ) stimulent le système orthosympathique par différentes voies. Chez le sujet normal, ils augmentent la TA et la FC par vasoconstriction périphérique, stimulation cardiaque et augmentation des résistances périphériques, et induisent une sudation . Lors de stimulations périphériques (cutanées, musculaires ou viscérales), les afférences transitent par la moelle pour atteindre les structures centrales (principalement l’hypothalamus et les centres vasomoteurs bulbaires). Lors de stimulations centrales (calcul mental, bruit soudain), la transmission à ces structures est directe. Dans tous les cas, la voie efférente est constituée des voies orthosympathiques vers le cœur et les vaisseaux périphériques.
2.1.3
La fonction sudomotrice
La fonction sudomotrice peut être évaluée par des tests sudatoires thermiques, par le réflexe d’axone sudomoteur ou par les réponses cutanées sympathiques (RCS). Les tests sudatoires thermiques à la quinizarine ont été décrits par Guttmann en 1947 et le réflexe d’axone (médié par les fibres orthosympathiques postganglionnaires sudomotrices) nécessitent un matériel spécifique et ont été peu utilisés chez le BM. À l’inverse, les RCS constituent un test simple et rapide à réaliser en laboratoires d’électrophysiologie .
Les tests cliniques au lit du malade sont actuellement peu utilisés, en dehors de la raie vasomotrice . L’analyse de la sudation (test de la petite cuiller) , l’observation de la piloérection , le réflexe de dilatation pupillaire lors de stimulation nociceptive thoracique méritent certainement une réévaluation.
2.2
Méthode
La revue de la littérature a porté sur les publications en langue anglaise indexées dans PubMed concernant les tests cardiovasculaires et sudomoteurs chez le BM. Les termes « spinal cord inury » ET « autonomic testing » ont été combinés de la façon suivante : « spinal cord injury OU tetraplegia OU quadriplegia OU paraplegia » ET « cold pressor test OU Valsalva manoeuvre OU postural challenge OU respiratory challenge OU tilt test OU sympathetic skin responses OU sweating ». L’auteur principal a ensuite passé en revue tous les titres et abstracts trouvés, et a acquis les articles des études éligibles. Les bibliographies des articles ont été étudiées pour trouver des articles additionnels.
Pour être éligibles, les études devaient :
- •
présenter une description détaillée des populations étudiées, en particulier leur niveau neurologique et la sévérité de la lésion ;
- •
donner une description adéquate des tests utilisés ;
- •
donner les résultats détaillés des tests sur le plan cardiovasculaire (TA et FC) ou sudomoteur (main ou pied) pour chaque sujet ;
- •
être publiés en anglais.
Par souci de clarté, nous considérons trois niveaux d’atteinte médullaire (tétraplégique, paraplégique T6 et paraplégique T10) : ces patients présentent des réactions végétatives caractéristiques déterminées par leur niveau lésionnel. En effet, le flux efférent orthosympathique T1–T5 (innervation cardiaque) et T5–T10 (innervation du territoire vasculaire splanchnique) sont directement impliqués dans le contrôle cardiovasculaire du BM (HRA, hypotension orthostatique), alors que le flux orthosympathique T10–L2 est impliqué dans le contrôle des fonctions sphinctériennes (bas appareil urinaire, fonctions sexuelles et anorectales).
2.3
Résultats
Sauf indication contraire, la description fait référence à des patients présentant une lésion somatique complète (échelle incapacité ASIA [AIS] A) au stade chronique.
2.3.1
Patients tétraplégiques
Chez le tétraplégique complet, la colonne orthosympathique est totalement déconnectée du contrôle cérébral ( Fig. 1a ) . Toute afférence sous le niveau lésionnel sera susceptible d’activer par voie réflexe l’entièreté de la moelle orthosympathique.