Correct acetabular cup position is critical to successful total hip replacement. Unfortunately, malposition of acetabular cups is common and leads to increased rates of dislocation, wear, and ion toxicity. Despite the popularity of Lewinnek’s safe zone, the exact target of acetabular abduction and version remains elusive. Differences in functional pelvic position, surgical approach, and femoral anteversion affect the optimal cup position for individual patients. Surgeons need to be aware of pelvic position changes from the supine to lateral decubitus position.
- •
Acetabular component placement is a critical part of total hip arthroplasty.
- •
Improper placement can lead to increased dislocation rate, accelerated bearing surface wear, limited range of motion, and higher revision rates.
- •
Factors that cause poor acetabular component placement include poor visualization, increased BMI, surgeon volume, inherent inaccuracies of external positioning guides, and the inability to consistently obtain and maintain patient position.
- •
Many surgical techniques can aid in proper acetabular cup position, such as using boney landmarks, computer navigation, and preoperative templating.
Introduction
Correct acetabular component position is a critical part of a successful total hip arthroplasty (THA). Improper acetabular orientation leads to an increased dislocation rate, accelerated bearing surface wear, limited range of motion, and higher revision rates. Many factors can cause poor acetabular component placement, including poor visualization of the acetabulum and surrounding anatomy, increased body mass index (BMI), surgeon volume, inherent inaccuracies of external positioning guides, and the inability to consistently obtain and maintain precise patient positioning during the procedure. This article discusses the adverse events associated with malposition, the multiple etiologies of acetabular component malposition, and the surgical techniques available to obtain accurate acetabular component placement in THA.
Acetabular component malposition: adverse effects
Dislocation
Dislocation is a devastating complication after total hip arthroplasty. Many inherent patient factors predispose to postoperative dislocation, such as previous surgery and neurologic impairment. Although these factors can be considered outside the surgeon’s direct control, acetabular component orientation can and should be optimized by the surgeon.
Multiple surgeons have described a safe range that optimizes stability and decreases potential for hip dislocation. Lewinnek and colleagues defined the anatomic safe zone for acetabular component position after reviewing a series of 300 THAs that had a dislocation rate of 3%. After precisely measuring the orientation of the acetabular component, they found that anterior dislocations were associated with increased acetabular component anteversion and defined a safe range of 15° ± 10° anteversion and 40° ± 10° of lateral opening (acetabular abduction inclination angle). They noted a 1.5% dislocation rate when the cup was placed in the safe zone versus a 6.1% dislocation rate when the cup was positioned outside of the safe zone. McCollum and Gray also described a safe range for acetabular component position. They reviewed 441 THAs performed using a posterior approach with a dislocation rate of 1.14%. To prevent impingement and dislocation, they determined that the safest range for cup position was between 30° and 50° of abduction and between 20° and 40° of anteversion.
Other surgeons suggest that patient factors seem to be more important than cup position in determining the incidence of dislocation. Pierchon and colleagues thought that muscular imbalance rather than malposition of the components was the major factor determining dislocation. They reviewed the radiographs and computed tomography (CT) scans of 38 total hip arthroplasties that had dislocated (36 posteriorly and 2 anteriorly) and compared the alignment of the prosthetic components with those of 14 uncomplicated arthroplasties. They found no difference in alignment of the prosthetic components when the 2 groups were compared. In the 7 patients who did have reoperations, the cause of dislocation diagnosed by CT was confirmed in only 2 cases (1 retroversion of the cup and 1 protruding osteophytes).
Paterno and colleagues reviewed 446 patients who had 391 primary THAs and 169 revision THAs to determine the influence of patient-related, operative factors and the position of the acetabular component on the rate of dislocation. Dislocation occurred after 32 (6%) of the 560 THAs: 17 (4%) of the 391 primary procedures and 15 (9%) of the 169 revisions ( P = .046). Radiographic analysis was performed for the 32 hips that had dislocated, and results were compared with 32 matched hips that had not dislocated. They did not detect an association between either acetabular component version or abduction inclination angle and the incidence of dislocation. In fact, 30 of 32 hips in each group had an abduction angle of the acetabular component that was in the so-called safe range of 30°–50°. They did note an association with excessive alcohol intake in the hips that dislocated.
In a multivariate analysis, Jolles and colleagues evaluated the relative influence of various mechanical and patient-related factors on the incidence of dislocation after primary THA. Of 2023 THAs, 21 patients who had at least one 1 dislocation were compared with a control group of 21 patients without dislocation, matched for age, sex, pathology, and year of surgery. Implant positioning, seniority of the surgeon, American Society of Anesthesiologists score, and diminished motor coordination were recorded. Data analysis included univariate and multivariate methods. The dislocation risk was 6.9 times higher if combined femoral-acetabular anteversion was not between 40° and 60° and 10 times higher in patients with high American Society of Anesthesiologists scores.
Increased Wear and Periprosthetic Osteolysis
Acetabular component malposition is associated with increased wear rates in polyethylene bearings. Little and colleagues evaluated 43 THAs that had been treated with conventional polyethylene at a 49-month mean follow-up. They found that hips with an acetabular component abduction angle of less than 45° had a mean wear rate of 0.12 mm/y, whereas those with an abduction angle of greater than 45° had a mean wear rate of 0.18 mm/year ( P = .012) ( Fig. 1 ). Patil and colleagues used a finite-element model to compute contact stress during the normal gait cycle with the acetabular component oriented to simulate 45° versus 55° of abduction. In a corresponding clinical study, these investigators followed 60 THAs for as long as five years. Radiographs were used to analyze the abduction inclination angle of the acetabular component as well as polyethylene wear. The finite-element analysis predicted increased peak contact stresses with increased abduction angle and reduced peak contact stresses with an increased anteversion angle. A 40% increase in mean linear polyethylene wear was noted in acetabular components positioned with an abduction angle of greater than 45°.

A more horizontal cup position may lead to decreased pelvic osteolysis. Kennedy and colleagues noted a decreased incidence of pelvic osteolysis with more horizontal placement of an acetabular component. They reviewed 75 THAs to examine the effect of acetabular component position. In group A, 38 components were placed in a vertical position with a mean angle of inclination of 61.9°. Three of these patients had recurrent dislocations necessitating acetabular component revision. In group B, 37 components were placed in a more horizontal orientation with a mean inclination of 49.7°. Only one 1 of these hips dislocated and required revision. Radiographs at 4-year follow up showed pelvic osteolysis in 24% of the hips in group A versus 13% of the hips in group B. Asymmetric polyethylene wear was observed in 5.1% of the hips in group A and in none of the THAs in group B.
Del Schutte and colleagues, on the other hand, evaluated the wear rates of cemented all-polyethylene acetabular components in 364 THAs to determine the effect of the acetabular abduction angle. The polyethylene wear rates were calculated by measuring the shortest radius from the center of the prosthetic femoral head to a point on the outer surface of the acetabular cup. An immediate standardized postoperative radiograph was compared with a follow-up radiograph at least 9.5 years later. The mean abduction inclination angle was 44.1° (standard deviation, 9.2°) with a median of 44°. The range of abduction was from 0° to 85°. The analysis did not show a correlation between the amount of acetabular abduction and polyethylene wear rates (Pearson’s correlation coefficient, 0.0679).
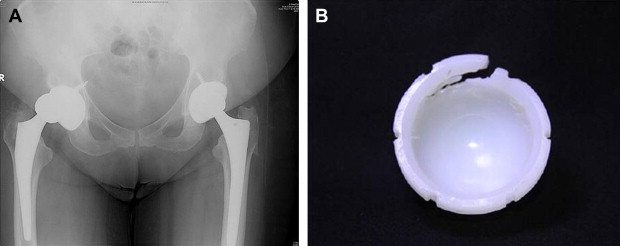
Catastrophic Polyethylene Failure
Vertical acetabular component placement can lead to catastrophic failure of THAs. Waewsawangwong and Goodman presented the unexpected failure of a highly cross-linked polyethylene liner in a THA at 20 months. Operative findings showed a fracture of the superior rim at the locking groove of the liner. The investigators concluded that the failure was related to the decreased mechanical properties of highly cross-linked polyethylene, a vertical acetabular component (abduction angle 65°), and use of large femoral head resulting in reduced polyethylene thickness ( Fig. 2 ). Tower and colleagues also reported fatigue fracture at the superior rim of 4 retrieved highly cross-linked liners. They postulated that the failure of the liners was caused by thin polyethylene at the cup rim, vertical cup alignment (abduction angles >65°), and decreased mechanical properties of highly cross-linked polyethylene. Crowninshield and colleagues used finite-element analysis to predict the location of maximum tensile stress in acetabular components. They found that for a 40-mm head size, the maximum tensile stress in the polyethylene liner is more than 5 times greater in a vertical cup under a subluxation scenario than a stable cup with an abduction angle of 45°.
Alternative Bearing Wear
Malposition of acetabular components also increases wear rates in alternative bearings. Hart and colleagues reviewed the orientation of acetabular and femoral components in 45 patients who had undergone revision of metal-on-metal hip resurfacings using 3-dimensional CT scans. Abduction angles greater than 55° strongly correlated with increased wear rates. They also noted that high wear components were typically implanted outside Lewinnek’s safe zone. De Haan and colleagues examined the relationships between the serum levels of chromium and cobalt ions and the inclination angle of the acetabular component in 214 patients implanted with a metal-on-metal resurfacing hip replacement. They found that steeply inclined acetabular components, with abduction angles greater than 55°, combined with a small size of component, were likely to give rise to higher serum levels of cobalt and chromium.
The squeaking of ceramic-on-ceramic total hip replacements has been associated with acetabular cup malposition. Sexton and colleagues reviewed 2406 primary total hip replacements with ceramic-on-ceramic bearing surfaces and identified 74 squeaking hips at a mean follow up of 9.5 years. High acetabular component inclination, high femoral offset, lateralization of the hip center, and either high or low acetabular component anteversion were good predictors of squeaking.
Limited Hip Range of Motion
Acetabular component malposition decreases hip range of motion. Kummer and colleagues evaluated how the orientation of the acetabular component affected the range and amount of rotation in a sawbone hemipelvis model. They found that parameters that allowed for maximal range of rotation were an acetabular component angle of inclination between 35° and 45° and cup anteversion between zero and 10°. They concluded that cup anteversion angles greater than 20° and cup abduction inclination greater than 45° limited internal and external rotation, particularly in hip flexion greater than 60°.
D’Lima and colleagues found that acetabular abduction angles between 45° and 55°, when combined with appropriate acetabular and femoral anteversion, resulted in a maximum overall range of motion and stability with respect to prosthetic impingement. They used a computer model to determine the effects of the positions of the acetabular and femoral components and of varying head/neck ratios on impingement and range of motion. They noted that acetabular abduction angles of less than 45° decreased flexion and abduction of the hip, whereas higher angles decreased adduction and rotation. Femoral and acetabular anteversion increased flexion but decreased extension.
Higher Revision Rate
Acetabular component malposition is associated with a higher revision rate. Sugano and colleagues compared the midterm results of 53 ceramic-on-ceramic bearing couples placed with CT-based navigation with 111 ceramic-on-ceramic bearing couples placed without navigation at 6-year follow-up. With navigation, all acetabular components were placed within the safe zone defined by Lewinnek and colleagues. 3 Without navigation, 31 of the components were placed outside this zone. Hips treated without navigation had a higher rate of dislocation. Revision was performed in 2 nonnavigated cases, one for aseptic loosening and one for fracture of the ceramic liner. Both showed evidence of neck impingement. Five cases undertaken without navigation showed erosion of the posterior aspect of the neck of the femoral component on the lateral radiographs. These 7 impingement-related mechanical problems correlated with malorientation of the acetabular component.
Pain after THA
Pain after THA can be caused by conditions such as infection, aseptic loosening, heterotopic ossification, referred pain, and soft tissue inflammation. Trousdale and colleagues reported 2 cases of persistent iliopsoas tendinitis after THA. They believed the pain was related to psoas tendon impingement against a malpositioned (retroverted), uncemented, metal-backed acetabular component in which the anterior rim of the malpositioned acetabular component resulted in chronic irritation of the tendon.
Acetabular component malposition: adverse effects
Dislocation
Dislocation is a devastating complication after total hip arthroplasty. Many inherent patient factors predispose to postoperative dislocation, such as previous surgery and neurologic impairment. Although these factors can be considered outside the surgeon’s direct control, acetabular component orientation can and should be optimized by the surgeon.
Multiple surgeons have described a safe range that optimizes stability and decreases potential for hip dislocation. Lewinnek and colleagues defined the anatomic safe zone for acetabular component position after reviewing a series of 300 THAs that had a dislocation rate of 3%. After precisely measuring the orientation of the acetabular component, they found that anterior dislocations were associated with increased acetabular component anteversion and defined a safe range of 15° ± 10° anteversion and 40° ± 10° of lateral opening (acetabular abduction inclination angle). They noted a 1.5% dislocation rate when the cup was placed in the safe zone versus a 6.1% dislocation rate when the cup was positioned outside of the safe zone. McCollum and Gray also described a safe range for acetabular component position. They reviewed 441 THAs performed using a posterior approach with a dislocation rate of 1.14%. To prevent impingement and dislocation, they determined that the safest range for cup position was between 30° and 50° of abduction and between 20° and 40° of anteversion.
Other surgeons suggest that patient factors seem to be more important than cup position in determining the incidence of dislocation. Pierchon and colleagues thought that muscular imbalance rather than malposition of the components was the major factor determining dislocation. They reviewed the radiographs and computed tomography (CT) scans of 38 total hip arthroplasties that had dislocated (36 posteriorly and 2 anteriorly) and compared the alignment of the prosthetic components with those of 14 uncomplicated arthroplasties. They found no difference in alignment of the prosthetic components when the 2 groups were compared. In the 7 patients who did have reoperations, the cause of dislocation diagnosed by CT was confirmed in only 2 cases (1 retroversion of the cup and 1 protruding osteophytes).
Paterno and colleagues reviewed 446 patients who had 391 primary THAs and 169 revision THAs to determine the influence of patient-related, operative factors and the position of the acetabular component on the rate of dislocation. Dislocation occurred after 32 (6%) of the 560 THAs: 17 (4%) of the 391 primary procedures and 15 (9%) of the 169 revisions ( P = .046). Radiographic analysis was performed for the 32 hips that had dislocated, and results were compared with 32 matched hips that had not dislocated. They did not detect an association between either acetabular component version or abduction inclination angle and the incidence of dislocation. In fact, 30 of 32 hips in each group had an abduction angle of the acetabular component that was in the so-called safe range of 30°–50°. They did note an association with excessive alcohol intake in the hips that dislocated.
In a multivariate analysis, Jolles and colleagues evaluated the relative influence of various mechanical and patient-related factors on the incidence of dislocation after primary THA. Of 2023 THAs, 21 patients who had at least one 1 dislocation were compared with a control group of 21 patients without dislocation, matched for age, sex, pathology, and year of surgery. Implant positioning, seniority of the surgeon, American Society of Anesthesiologists score, and diminished motor coordination were recorded. Data analysis included univariate and multivariate methods. The dislocation risk was 6.9 times higher if combined femoral-acetabular anteversion was not between 40° and 60° and 10 times higher in patients with high American Society of Anesthesiologists scores.
Increased Wear and Periprosthetic Osteolysis
Acetabular component malposition is associated with increased wear rates in polyethylene bearings. Little and colleagues evaluated 43 THAs that had been treated with conventional polyethylene at a 49-month mean follow-up. They found that hips with an acetabular component abduction angle of less than 45° had a mean wear rate of 0.12 mm/y, whereas those with an abduction angle of greater than 45° had a mean wear rate of 0.18 mm/year ( P = .012) ( Fig. 1 ). Patil and colleagues used a finite-element model to compute contact stress during the normal gait cycle with the acetabular component oriented to simulate 45° versus 55° of abduction. In a corresponding clinical study, these investigators followed 60 THAs for as long as five years. Radiographs were used to analyze the abduction inclination angle of the acetabular component as well as polyethylene wear. The finite-element analysis predicted increased peak contact stresses with increased abduction angle and reduced peak contact stresses with an increased anteversion angle. A 40% increase in mean linear polyethylene wear was noted in acetabular components positioned with an abduction angle of greater than 45°.
A more horizontal cup position may lead to decreased pelvic osteolysis. Kennedy and colleagues noted a decreased incidence of pelvic osteolysis with more horizontal placement of an acetabular component. They reviewed 75 THAs to examine the effect of acetabular component position. In group A, 38 components were placed in a vertical position with a mean angle of inclination of 61.9°. Three of these patients had recurrent dislocations necessitating acetabular component revision. In group B, 37 components were placed in a more horizontal orientation with a mean inclination of 49.7°. Only one 1 of these hips dislocated and required revision. Radiographs at 4-year follow up showed pelvic osteolysis in 24% of the hips in group A versus 13% of the hips in group B. Asymmetric polyethylene wear was observed in 5.1% of the hips in group A and in none of the THAs in group B.
Del Schutte and colleagues, on the other hand, evaluated the wear rates of cemented all-polyethylene acetabular components in 364 THAs to determine the effect of the acetabular abduction angle. The polyethylene wear rates were calculated by measuring the shortest radius from the center of the prosthetic femoral head to a point on the outer surface of the acetabular cup. An immediate standardized postoperative radiograph was compared with a follow-up radiograph at least 9.5 years later. The mean abduction inclination angle was 44.1° (standard deviation, 9.2°) with a median of 44°. The range of abduction was from 0° to 85°. The analysis did not show a correlation between the amount of acetabular abduction and polyethylene wear rates (Pearson’s correlation coefficient, 0.0679).
Catastrophic Polyethylene Failure
Vertical acetabular component placement can lead to catastrophic failure of THAs. Waewsawangwong and Goodman presented the unexpected failure of a highly cross-linked polyethylene liner in a THA at 20 months. Operative findings showed a fracture of the superior rim at the locking groove of the liner. The investigators concluded that the failure was related to the decreased mechanical properties of highly cross-linked polyethylene, a vertical acetabular component (abduction angle 65°), and use of large femoral head resulting in reduced polyethylene thickness ( Fig. 2 ). Tower and colleagues also reported fatigue fracture at the superior rim of 4 retrieved highly cross-linked liners. They postulated that the failure of the liners was caused by thin polyethylene at the cup rim, vertical cup alignment (abduction angles >65°), and decreased mechanical properties of highly cross-linked polyethylene. Crowninshield and colleagues used finite-element analysis to predict the location of maximum tensile stress in acetabular components. They found that for a 40-mm head size, the maximum tensile stress in the polyethylene liner is more than 5 times greater in a vertical cup under a subluxation scenario than a stable cup with an abduction angle of 45°.





