Electrodiagnostic studies play an important role in the evaluation of radiculopathy. This article reviews the use of standard nerve conduction studies, late responses, evoked potentials, and needle electrode examination in the work-up of lumbosacral and cervical radiculopathy.
The clinical diagnosis of radiculitis indicates limb pain emanating from a spinal nerve or spinal nerve root. Objective findings of strength or reflex deficits or electrodiagnostic changes suggest nerve root dysfunction termed radiculopathy . Although commonly caused by structural lesions, such a herniated nucleus pulposus or degenerative spondylosis, radiculopathy can also be caused by inflammatory, infectious, or malignant disorders. Structural causes of radiculopathy may be readily apparent through common imaging modalities, such as MRI or computed axial tomography. However, MRI is associated with a significantly high false-positive rate in asymptomatic individuals and increases with age. In such equivocal cases, imaging may be complemented by electrodiagnostic testing. Electrodiagnostic testing is a functional evaluation of the nervous system. Electrodiagnostic testing also has the added benefit of allowing objective documentation of the chronicity and severity of peripheral nervous system disease.
Definition
Electrodiagnosis is a broad term encompassing multiple electrodiagnostic techniques, including needle electrode examination (NEE); motor and sensory nerve conduction studies (NCS), including late responses; and evoked potentials. These tests are frequently used in various combinations in the evaluation of radiculopathy primarily to rule out other disorders in the peripheral and central nervous system; however, the NEE is considered the crucial component in the electrodiagnostic evaluation of radiculopathy. To meet the electrodiagnostic criteria for a radiculopathy, abnormalities must be demonstrated in at least 2 muscles innervated by the same nerve root but different peripheral nerves with no abnormalities detected in muscles innervated by the adjacent nerve roots.
History and examination
The symptoms of many musculoskeletal and peripheral nerve disorders overlap with the clinical presentation of radiculopathy, therefore electrodiagnostic testing may be ordered for these populations to aide in establishing a diagnosis. Electrodiagnostic testing is not infallible and may be painful and expensive, therefore, as with many other forms of advanced diagnostic testing, electrodiagnosis should only be used as an extension of the history and physical examination. There have been studies done to evaluate the relationship between physical examination and electrodiagnostics. When 170 subjects were referred to an electrodiagnostic laboratory, 32% were diagnosed with a musculoskeletal disorder by standardized physical examination. However, of those subjects with normal electrodiagnostic studies, the prevalence of musculoskeletal disorders increased to 55%. When there was electrodiagnostic evidence of radiculopathy, the presence of a musculoskeletal disorder was still 21%. The significant overlap between the presence of lower-extremity musculoskeletal disorders and lumbosacral radiculopathy suggests that the presence or absence of a musculoskeletal diagnosis does not accurately predict which patients will have normal electrodiagnostic studies. In another study Lauder and colleagues calculated sensitivities, specificities, and predictive values of various symptoms and signs for those with an abnormal electrodiagnostic study. No historical feature was found to be significantly associated with an abnormal electrodiagnostic study. The most sensitive historical feature was the presence of radicular leg pain (86%), though this symptom had a specificity of only 12%. The investigators evaluated several physical examination findings and found the following sensitivities and specificities (sensitivity/specificity): reduced vibration or pinprick sensation (50%/62%), Achilles or patellar reflex deficit (25%/87%), weakness of any muscle (69%/53%), and positive straight leg raise (21%/87%). However, in subjects that had any 4 abnormal physical findings there was a greater than 6 times likelihood that the electromyogram (EMG) study would be abnormal when compared with cases with a normal physical examination.
As with lumbosacral radiculopathies, the value of the history and physical examination in predicting cervical radiculopathies has also been studied. Subjects with symptoms of numbness, tingling, and subjective weakness were more than twice as likely to have abnormal electrodiagnostic testing. Unfortunately, none of these symptoms were significant for radiculopathy specifically. In contrast, the presence of weakness, abnormal reflexes, or abnormal sensation on physical examination indicates a greater than 4 times likelihood of having an abnormal electrodiagnostic study, with a greater than 2 times likelihood of confirming a cervical radiculopathy. A particularly valuable physical examination finding is an abnormal biceps reflex, which increases the odds ratio of making an EMG diagnosis of cervical radiculopathy to 10. In general, the combination of having weakness and a reduced reflex was a strong predictor of both an abnormal electrodiagnostic study, including radiculopathy specifically. Notably, up to 48% of individuals with abnormal electrodiagnostic results will have a normal physical examination, emphasizing the physical examination’s relative lack of sensitivity when using electrodiagnosis as a gold standard.
History and examination
The symptoms of many musculoskeletal and peripheral nerve disorders overlap with the clinical presentation of radiculopathy, therefore electrodiagnostic testing may be ordered for these populations to aide in establishing a diagnosis. Electrodiagnostic testing is not infallible and may be painful and expensive, therefore, as with many other forms of advanced diagnostic testing, electrodiagnosis should only be used as an extension of the history and physical examination. There have been studies done to evaluate the relationship between physical examination and electrodiagnostics. When 170 subjects were referred to an electrodiagnostic laboratory, 32% were diagnosed with a musculoskeletal disorder by standardized physical examination. However, of those subjects with normal electrodiagnostic studies, the prevalence of musculoskeletal disorders increased to 55%. When there was electrodiagnostic evidence of radiculopathy, the presence of a musculoskeletal disorder was still 21%. The significant overlap between the presence of lower-extremity musculoskeletal disorders and lumbosacral radiculopathy suggests that the presence or absence of a musculoskeletal diagnosis does not accurately predict which patients will have normal electrodiagnostic studies. In another study Lauder and colleagues calculated sensitivities, specificities, and predictive values of various symptoms and signs for those with an abnormal electrodiagnostic study. No historical feature was found to be significantly associated with an abnormal electrodiagnostic study. The most sensitive historical feature was the presence of radicular leg pain (86%), though this symptom had a specificity of only 12%. The investigators evaluated several physical examination findings and found the following sensitivities and specificities (sensitivity/specificity): reduced vibration or pinprick sensation (50%/62%), Achilles or patellar reflex deficit (25%/87%), weakness of any muscle (69%/53%), and positive straight leg raise (21%/87%). However, in subjects that had any 4 abnormal physical findings there was a greater than 6 times likelihood that the electromyogram (EMG) study would be abnormal when compared with cases with a normal physical examination.
As with lumbosacral radiculopathies, the value of the history and physical examination in predicting cervical radiculopathies has also been studied. Subjects with symptoms of numbness, tingling, and subjective weakness were more than twice as likely to have abnormal electrodiagnostic testing. Unfortunately, none of these symptoms were significant for radiculopathy specifically. In contrast, the presence of weakness, abnormal reflexes, or abnormal sensation on physical examination indicates a greater than 4 times likelihood of having an abnormal electrodiagnostic study, with a greater than 2 times likelihood of confirming a cervical radiculopathy. A particularly valuable physical examination finding is an abnormal biceps reflex, which increases the odds ratio of making an EMG diagnosis of cervical radiculopathy to 10. In general, the combination of having weakness and a reduced reflex was a strong predictor of both an abnormal electrodiagnostic study, including radiculopathy specifically. Notably, up to 48% of individuals with abnormal electrodiagnostic results will have a normal physical examination, emphasizing the physical examination’s relative lack of sensitivity when using electrodiagnosis as a gold standard.
Nerve root variation
As previously described, the electrodiagnosis of radiculopathy relies upon a myotomal pattern of abnormalities found on NEE. However, variation in the anatomic pattern of nerve roots is known to exist and must be accounted for in the interpretation of the NEE. A study of 200 spontaneously aborted fetuses revealed 107 (53.5%) to show significant variation from the most common arrangement of the brachial plexus. The most common variants of brachial plexus organization are described as the prefixed and postfixed plexus. These variants have been variously defined and emphasize the contributions of the C4 and T2 roots. A prefixed plexus is characterized by a C4 branch that is larger than the branch from T2. The electromyographic implications of this are that C4 may contribute to the innervation of the shoulder girdle musculature, which is more typically C5. In contrast, a postfixed plexus contains a large contribution from T2, and a small contribution from C4. Prefixation may be seen in up to 48% of specimens ; whereas, postfixation is seen in 0.5% to 4.0% of cases.
Precise localization through the NEE is similarly challenged in the electrodiagnosis of lumbosacral radiculopathy. Though the vast majority of lumbosacral radiculopathies occur at either L5 (47.6%) or S1 (30%), both of these nerve roots may show significant variation from normal patterns of innervations. In a study of 50 subjects undergoing lumbar decompression surgery, intraoperative stimulation of the L5 and S1 nerve roots revealed 16% to have significant deviations from normal. Common anomalies in this study include dominant nerve roots that were expressed more heavily in muscles than normal, and such anomalies were more frequent in subjects with transitional vertebral segments. A novel study compared the neurologic symptoms generated by selective nerve root blocks using electrical stimulation in subjects with transitional and normal lumbar segments. In this study, when L5 is sacralized, the function of the L5 nerve root becomes similar to the S1 nerve root. Such normal variations in peripheral nervous system anatomy must be accounted for in the performance of the NEE.
Sensitivity of EMG
Although the diagnosis of radiculopathy hinges upon the NEE, the sensitivity of EMG in detecting radiculopathy is limited by several factors. First this procedure is targeted exclusively toward motor axons. Radiculopathies with predominant sensory root involvement, even if severe, will not elicit any needle electrode abnormalities. However, substantial demyelinating disease may be detected on the NEE by changes in motor unit recruitment. Unfortunately, significant demyelination at the level of the nerve root is uncommon. Secondly, the electrodiagnostic confirmation of a radiculopathy rests upon an identification of a myotomal pattern of abnormalities. Such identification may not occur if axonal compromise is not severe enough to be detected by the needle electrode or widespread enough to localize to a particular myotome. Thirdly, the appearance of fibrillation potentials is time dependent and may not appear in limb muscles several weeks after axonal damage. Therefore, if done too early, an NEE will not appreciate fibrillations because they have not yet developed. Also, if done too late, fibrillation potentials are known to shrink because of muscle atrophy and thus become more difficult to appreciate. This effect has happened 6 months after the onset of cervical radiculopathies and 12 to 18 months after the onset of lumbosacral radiculopathies.
Besides these inherent limitations, measurement of the sensitivity of electrodiagnostic studies is complicated by the lack of a gold standard. In determining the sensitivity of electrodiagnostic testing, various criterion standards have been used, such as clinical, surgical, and radiological findings. The clinical sensitivity of electrodiagnostic testing in lumbosacral radiculopathy ranges between 49% and 84%. Haig and colleagues performed a stringent study using validated, anatomic needle placement into the limb muscles and a quantified “paraspinal mapping” technique to evaluate the sensitivity and specificity of electrodiagnostic testing in lumbar spinal stenosis. The composite limb and paraspinal fibrillation score showed a sensitivity of 47.8% and a specificity of 87.5%. This finding agrees with the 44% sensitivity and 86% specificity obtained by Coster and colleagues using radiological evidence of nerve root compression as a gold standard. In comparison, although the prevalence of both disc bulges and protrusions increases with age, if not stratified by age, MRI of the lumbar spine shows a specificity of 36%; only 36% of people without back pain will have a normal disc at all levels. The much higher sensitivity of MRI justifies its appropriateness as a screening test; whereas, the greater specificity of electrodiagnostics suggests that it is better used as a confirmatory test.
Similar to lumbosacral radiculopathy, the electrodiagnostic evaluation of cervical radiculopathies also shows a wide range of sensitivities, from 50% to 95%. The false positive rate of cervical MRI is somewhat lower, but still significant at 14% of asymptomatic individuals aged less than 40 years and 28% of those aged greater than 40 years. Therefore, electrodiagnostics and MRI can be complementary rather than competing modalities. Electrodiagnostic studies and MRI will agree in 60% of patients with symptoms suggestive of radiculopathy and in 76% of cases when weakness is present.
Sensory nerve conduction studies
Abnormalities in sensory nerve action potentials (SNAP) are not part of the electrodiagnostic criteria of radiculopathy. However, their performance is necessary to evaluate for other disorders that are part of the differential diagnosis of radiculopathy, such as peripheral polyneuropathy or entrapment mononeuropathy. As symptoms of pain are typically mediated by C-fibers, which are too small to be accessible by standard electrodiagnostic techniques, sensory nerve parameters, such as amplitude, distal latency, and nerve conduction velocity, are not expected to be abnormal in radiculopathy. Also, in radiculopathy the usual location of the lesion is proximal to the dorsal root ganglion, and degeneration will proceed centrally rather than peripherally. However, important exceptions to this dictum must be recognized. When pathology extends from the intraspinal space into the neural foramen and affects the dorsal root ganglion, as can happen with malignancy or infection, SNAP amplitude reduction will occur as a result of wallerian degeneration. Additionally, SNAP amplitudes may be reduced when the dorsal root ganglion has an intraspinal location making it vulnerable to lesions resulting from lumbar spondylosis. This reduction may occur in L5 radiculopathies, causing reduction of superficial peroneal nerve amplitudes. Reduction of superficial peroneal nerve amplitudes are seen in 21.1% of patients with L5 radiculopathy who are aged less than 60 years.
Evaluation of possible entrapment mononeuropathy is an important reason to perform nerve conduction studies in the electrodiagnostic evaluation of radiculopathy. For example, the prevalence of carpal tunnel syndrome in patients with cervical radiculopathy has been estimated at 22.1%, which is significantly greater than estimates for the general population (0.52% for men and 1.49% for women). The double crush hypothesis was put forth in 1973 by Upton and McComas and proposes that a proximal lesion along an axon, such as that caused by radiculopathy, predisposes it to injury at a more distal site. Such a mechanism is one hypothesis as to why the incidence of carpal tunnel syndrome seems to be increased in patients with cervical radiculopathy. However, another study did not reveal any correlation between the presence of C6 or C7 radiculopathy and abnormal median sensory responses and C8 radiculopathy and abnormal median motor responses. Prior studies have shown similar results. Other possible reasons why the incidence of carpal tunnel syndrome is increased in patients with cervical radiculopathy is that both disorders have a common etiology, such as osteoarthritis that leads to both cervical foraminal and carpal tunnel stenosis.
Motor nerve conduction studies
Compound muscle action potentials (CMAP) may be abnormal in the presence of a radiculopathy if axon loss is occurring. The amplitude of the CMAP can provide a semiquantitative measure of the number of axons supplying the muscle from which the recording was made. Therefore, L5 and S1 radiculopathies may cause reduction of peroneal CMAPs, recording from the extensor digitorum brevis and the abductor hallucis, respectively. However, the CMAP amplitude is not perfectly sensitive to the presence of a lumbosacral radiculopathy. Significant reduction in CMAP amplitudes occurs with loss of approximately 50% of motor axons and it is rare for this many nerve root fibers to degenerate. Additionally, muscles typically have an overlapping nerve supply, allowing for redundancy even if individual nerve roots are compromised.
Another limitation of using the CMAP amplitude to diagnose is emphasized in the evaluation of cervical radiculopathies. The most commonly performed upper extremity motor nerve conduction studies are the median and ulnar motor nerve conduction studies to the abductor pollicis brevis and the abductor digiti minimi, respectively. These muscles are predominantly subserved by the C8 and T1 nerve roots. However, the most common cervical radiculopathies occur at C7 and C6, implying that the most commonly performed upper extremity motor nerve conduction studies will be insensitive for the most common cervical radiculopathies.
Late responses
Late responses are so named because their latency exceeds that of the more commonly studied M-wave. Their theoretical advantages include their ability to study the proximal nerve segments where the pathology of radiculopathy lies.
H Reflex
The H reflex was first described by Hoffman in 1918 and subsequently hypothesized by Magladery to be a monosynaptic reflex that assesses the afferent Ia sensory nerve and an efferent alpha motor nerve. However, other experimental studies have concluded that the pathways generating the H reflex likely receive an oligosynaptic contribution. In clinical practice, the H reflex is most commonly obtained by stimulating the tibial nerve in the popliteal fossa and recording over the gastroc-soleus to assess the S1 nerve root, although the H reflex may also be obtained from the flexor carpi radialis in the forearm. The H reflex requires a longer-duration stimulus that is optimally between 0.5 and 1.0 ms. The sensitivity of the H reflex for nerve pathology has been estimated to be between 82% and 89%, and can be compromised through preferential sparing of the fibers that mediate the reflex. However, specificity for radiculopathy is compromised by several factors. The entire H reflex arc travels through peripheral nerve, lumbosacral plexus, and spinal nerve roots. Abnormalities in any of these segments can disturb the H reflex and cannot be considered specific for radiculopathy. Additionally, H reflexes may not normalize once they become abnormal, limiting their use in monitoring patients with known S1 radiculopathies. Finally, H reflexes may be abnormal bilaterally in patients aged more than 60 years or secondary to peripheral polyneuropathy. Both latency and amplitude have been used as parameters to evaluate the H reflex. Amplitude has been criticized as less sensitive because of its variation with posture, muscle contracture, age, and temperature. However, comparative studies have suggested amplitude ratio to be a better parameter of S1 radiculopathy, particularly when H reflexes are present bilaterally. Various techniques have been described for eliciting the tibial H reflex ( Figs. 1 and 2 ).

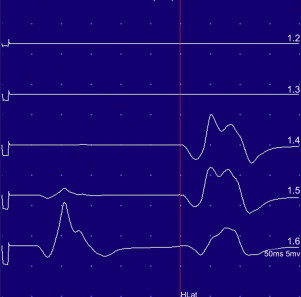
More recently, a simple and reproducible method known as the half and half technique described by Nishida has the advantages of producing a biphasic waveform with initial negative deflection. Such a waveform has easier-to-determine amplitude and latency parameters in comparison to the triphasic waveforms generated by the other methods ( Figs. 3 and 4 ). However, this method has no published normative data and has been criticized as producing nonphysiologic wave-forms; further study will be needed to determine its validity.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





