Abstract
Background and objective
Phantom limb pain (PLP) is a major problem after limb amputation. Mirror therapy (MT) is a non-pharmacological treatment using representations of movement, the efficacy of which in reducing PLP remains to be clarified. Here, we present the first systematic review on MT efficacy in PLP and phantom limb movement (PLM) in amputees (lower or upper limb).
Methods
A search on Medline, Cochrane Database and Embase, crossing the keywords “Phantom Limb” and “Mirror Therapy” found studies which were read and analyzed according the PRISMA statement.
Results
Twenty studies were selected, 12 on the subject of MT and PLP, 3 on MT and PLM, 5 on MT and both (PLP and PLM). Among these 20 studies, 5 were randomized controlled trials (163 patients), 6 prospective studies (55 patients), 9 case studies (40 patients) and methodologies were heterogeneous. Seventeen of the 18 studies reported the efficacy of MT on PLP, but with low levels of evidence. One randomized controlled trial did not show any significant effect of MT. As to the effect of MT on PLM, the 8 studies concerned reported effectiveness of MT: 4 with a low level of evidence and 4 with a high level of evidence. An alternative to visual illusion seems to be tactile or auditory stimulation.
Conclusion
We cannot recommend MT as a first intention treatment in PLP. The level of evidence is insufficient. Further research is needed to assess the effect of MT on pain, prosthesis use, and body representation, and to standardize protocols.
1
Introduction
Limb amputation gives rise to pain of different types, among which should be distinguished pains localised on the stump, and projected pains described by the patient as being perceived in the area of the lost limb, known as phantom limb pain (PLP) . These should be differentiated from the mere perception of an amputated limb, which is not painful or disagreeable (known as phantom limb sensation [PLS]). The phantom limb can also be perceived in movement (phantom limb movement [PLM]) . These different types of pain can coexist in a single patient, and the relative place of each type can be difficult to identify, in particular because of the subjective nature of pain and the emotional setting, often seriously affected by the amputation. PLP is thought to affect 50% of patients, appearing in the 6 months following amputation and sometime lasting several years . When PLP becomes chronic, it affects quality-of-life and increases the restrictions in activity caused by the amputation, possibly compromising social and/or professional reintegration .
There are various therapeutic options for PLP. Some are pharmaco-therapeutic: gabapentine, amitriptyline, tricyclic antidepressants, morphine-based reparations, ketamine . Others are based on non-pharmacological treatment–transcutaneous electric nerve stimulation (TENS), transcranial magnetic stimulation, spinal cord stimulation, the use of prostheses, hypnosis, acupuncture etc.
In this second category, mirror therapy (MT) is one of the techniques consisting in representing movement, like motor imagery and movement observation. Using the reflection of voluntary movements in a mirror performed by the intact limb, it consists in creating the visual illusion of non-painful movement in the phantom limb.
The aim, by way of this representation of the missing limb in imaginary movement, is to obtain the restoration of its projection in the corresponding cortical motor and sensory areas, and thus to reduce the pain linked to the breaking-off of sensory information . Indeed, after an amputation, the primary somato-sensory and motor cortical areas connected to the amputated limb are no longer solicited. Functional neuro-imagery has shown that they are progressively replaced by adjacent cortical areas . The extent to which this post-amputation cortical reorganisation occurs could be correlated with pain scores . MT is thought to establish enhanced coherence between motor command and sensory feedback by way of the reflected image , and in the medium term to reduce this deleterious cortical reorganisation . It has also been suggested that the activation of the contra-lesional mirror neurones derived from MT could have a pain-killing function .
MT was initially proposed by Ramachandran et al. for the treatment of PLP , and it was subsequently applied to other chronic pains, such a complex regional pain syndrome and neuropathic limb pain.
We propose here a review of the literature concerning the application of MT to PLP following upper or lower limb amputation, aiming to assess contra-indications, beneficial effects, conditions of application and any deleterious effects.
2
Method
2.1
Study eligibility criteria
A systematic review of the literature was performed with two independent perusals in accordance with the Prisma guidelines ( www.prisma-statement.org/ ). Only articles in English were retained. The eligibility criteria were any articles on the subject of MT applied to patients following amputation of upper or lower limbs. Articles concerning the application of MT to other pathologies such as stroke sequellae, complex regional pain syndrome, brachial plexus lesions, or sequellae of limb fractures were excluded, as were articles on virtual immersion. Literature reviews were not analysed.
2.2
Sources
The Medline, Cochrane and Embase databases for the period 1996 to 2015 were consulted. The words sought in the titles, abstracts and keywords were: phantom limb, mirror therapy.
2.3
Studies selected and data collection procedure
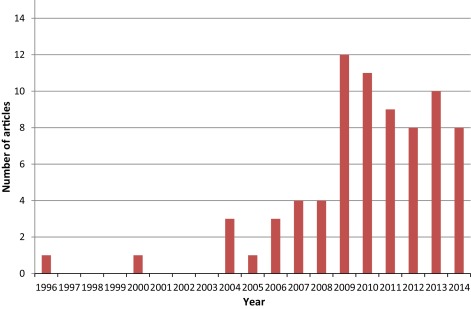
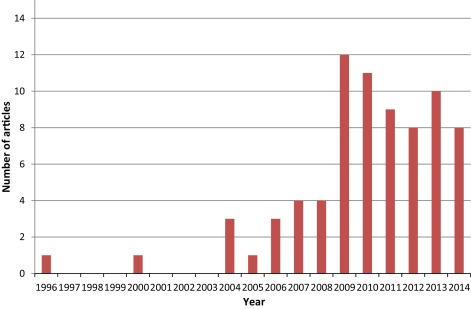
Up to the 26th November 2015, 85 articles were retrieved on the Medline, Cochrane and Embase databases with using the keywords phantom limb and mirror therapy. It was noted that from 2009, the number of articles increased markedly ( Fig. 1 ), showing increased interest in MT following amputation. The flow diagram in Fig. 2 shows the article selection procedure. Among the 85 articles, 5 were literature review . Only one was a review of the literature on MT among amputees . This article is a narrative review of the literature run in parallel with a survey among practitioners and patients. No table synthesising the articles analysed is presented. To our knowledge, our study is the first systematic review to specifically concern MT among amputees.
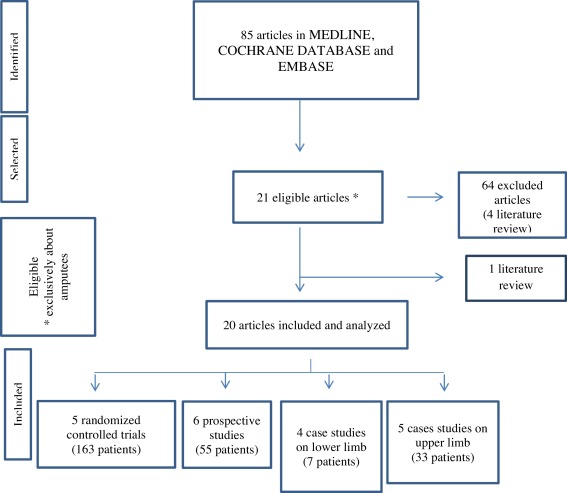
Finally, 20 studies on the subject of MT and PLP and/or PLM in amputees were included and analysed. Twelve were on the subject of MT and PLP, 3 on MT and PLM, and 5 on MT and both PLP and PLM. Among these 20 studies, 5 were randomized controlled trials (163 patients) , 6 prospective studies (55 patients) , 9 case studies (40 patients) and methodologies were heterogeneous.
2
Method
2.1
Study eligibility criteria
A systematic review of the literature was performed with two independent perusals in accordance with the Prisma guidelines ( www.prisma-statement.org/ ). Only articles in English were retained. The eligibility criteria were any articles on the subject of MT applied to patients following amputation of upper or lower limbs. Articles concerning the application of MT to other pathologies such as stroke sequellae, complex regional pain syndrome, brachial plexus lesions, or sequellae of limb fractures were excluded, as were articles on virtual immersion. Literature reviews were not analysed.
2.2
Sources
The Medline, Cochrane and Embase databases for the period 1996 to 2015 were consulted. The words sought in the titles, abstracts and keywords were: phantom limb, mirror therapy.
2.3
Studies selected and data collection procedure
Up to the 26th November 2015, 85 articles were retrieved on the Medline, Cochrane and Embase databases with using the keywords phantom limb and mirror therapy. It was noted that from 2009, the number of articles increased markedly ( Fig. 1 ), showing increased interest in MT following amputation. The flow diagram in Fig. 2 shows the article selection procedure. Among the 85 articles, 5 were literature review . Only one was a review of the literature on MT among amputees . This article is a narrative review of the literature run in parallel with a survey among practitioners and patients. No table synthesising the articles analysed is presented. To our knowledge, our study is the first systematic review to specifically concern MT among amputees.
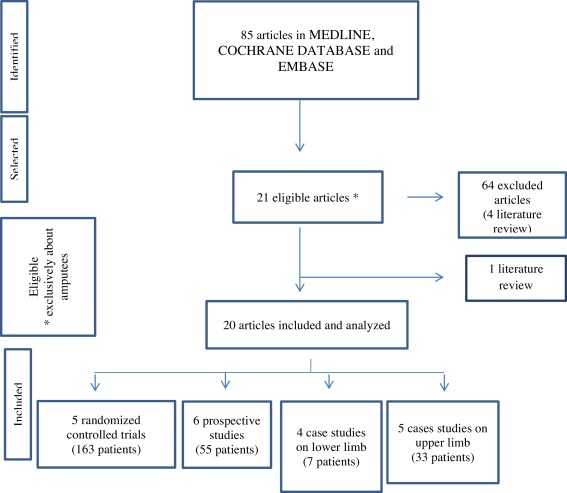
Finally, 20 studies on the subject of MT and PLP and/or PLM in amputees were included and analysed. Twelve were on the subject of MT and PLP, 3 on MT and PLM, and 5 on MT and both PLP and PLM. Among these 20 studies, 5 were randomized controlled trials (163 patients) , 6 prospective studies (55 patients) , 9 case studies (40 patients) and methodologies were heterogeneous.
3
Results
In the 20 articles selected, the following were explored: MT contra-indications, efficacy, terms of application, and side effects in the setting of PLP.
3.1
Contra-indications for the use of MT in PLP
The most frequently mentioned contra-indications were the existence of neurological or psychological comorbidities, pain in the remaining limb, or sight disturbances making visual feedback impossible .
3.2
The efficacy of TM on PLP
This was the main assessment criterion in the 20 studies retained ( Tables 1 and 2 ). Therapeutic efficacy was assessed by applying the criteria recommended by the French Haute Autorité de la santé for the evaluation of the level of scientific proof: 4 levels of proof ranging from 1–the most favourable level–(well-powered, randomised, comparative trials) to 4–the lowest level of proof (comparative studies with marked biases, retrospective studies, case series) .
| Phantom limb studies | PLA | PLS | PLM | PLP | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MT efficacy | + | – | NT | + | – | NT | + | – | NT | + | – | NT |
| Randomized controlled trials (5 studies) | 1 | 0 | 4 | 0 | 1 | 4 | 2 | 0 | 3 | 3 | 1 | 1 |
| Prospective studies (6 studies) | 1 | 0 | 5 | 0 | 0 | 6 | 2 | 0 | 4 | 5 | 0 | 1 |
| Case studies | ||||||||||||
| LL (4 studies) | 0 | 0 | 4 | 0 | 0 | 4 | 2 | 0 | 2 | 4 | 0 | 0 |
| UL (5 studies) | 0 | 0 | 5 | 1 | 0 | 4 | 2 | 0 | 3 | 5 | 0 | 0 |
| Number of studies | 2 | 18 | 1 | 1 | 18 | 8 | 12 | 17 | 1 | 2 | ||
| Studies | Application | |||||
|---|---|---|---|---|---|---|
| Article | Period | Number of sessions | Session duration | Instructions | Addition sensory stimulus | |
| Randomized controlled trial | Chan et al., 2007 | 4W | 1/d | 15 min | BSM | |
| Moseley, 2006 | 6W | NI | NI | 3 phases a | ||
| Tilak et al., 2015 | 4d | 1/d | 20 min | BSM | ||
| Prospective studies | Darnall et al., 2012 | 4W | Every day | 25 min | BSM | |
| Seidel et al., 2011 | 3W | 12 sessions (2/d, 2X/W) | 25–30 min | BSM | ||
| Schmalzl et al., 2013 | 8 sessions | NI | 1 min | BSM | Tactile | |
| Sumitami et al., 2008 | 20.4W | 1/d | 10 min | BSM | ||
| Mercier et al., 2009 | 8W | 2 sessions/W | 10 × 10 mvts–30 min–1 h | BSM | ||
| Case studies | ||||||
| LL | Hanling et al., 2010 | 2W | 1/j, 14 sessions | NI | NI | |
| Darnall 2009 | 3M | 3X/W | 20–30 min | Vacant | Respi | |
| MacLachlan et al., 2004 | 3W | 3X/d, 7/7 d | 10X10 mvts | BSM | ||
| Clerici et al., 2012 | 24W | 1/d | 30 min | BSM | Tactile | |
| UL | Ramachandran et al., 1996 | NI | NI | NI | BSM | Tactile |
| Kim et al., 2012 | 3M | 4X/W | 15 min | BSM | ||
| Wilcher et al., 2011 | NI | 2X/d | 15 min | BSM | Auditory | |
| Ramachandran et al., 2009 | NI | NI | NI | BSM | ||
| Grunert-Pluss et al., 2008 | NI | 5–6X/d | 5–10 min | BSM | Tactile | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





