Abstract
Gait and balance disorders are often major causes of handicap in patients with cerebellar ataxia. Although it was thought that postural and balance disorders in cerebellar ataxia were not treatable, recent studies have demonstrated the beneficial effects of rehabilitation programs. This article is the first systematic review on the treatment of postural disorders in cerebellar ataxia. Nineteen articles were selected, of which three were randomized, controlled trials. Various aetiologies of cerebellar ataxia were studied: five studies assessed patients with multiple sclerosis, four assessed patients with degenerative ataxia, two assessed stroke patients and eight assessed patients with various aetiologies. Accurate assessment of postural disorders in cerebellar ataxia is very important in both clinical trials and clinical practice. The Scale for the Assessment and Rating of Ataxia (SARA) is a simple, validated measurement tool, for which 18 of the 40 points are related to postural disorders. This scale is useful for monitoring ataxic patients with postural disorders. There is now moderate level evidence that rehabilitation is efficient to improve postural capacities of patients with cerebellar ataxia – particularly in patients with degenerative ataxia or multiple sclerosis. Intensive rehabilitation programs with balance and coordination exercises are necessary. Although techniques such as virtual reality, biofeedback, treadmill exercises with supported bodyweight and torso weighting appear to be of value, their specific efficacy has to be further investigated. Drugs have only been studied in degenerative ataxia, and the level of evidence is low. There is now a need for large, randomized, controlled trials testing rehabilitation programs suited to postural and gait disorders of patients with cerebellar ataxia.
Résumé
L’ataxie posturale cérébelleuse est source d’incapacité souvent majeure pour les patients. Elle a longtemps eu la réputation de ne pas être accessible au traitement. Plusieurs études récentes suggèrent au contraire que les patients ayant une ataxie posturale cérébelleuse peuvent être améliorés par la rééducation. Cet article est une des premières synthèses de la littérature sur le traitement de l’ataxie posturale cérébelleuse. Dix-neuf articles dont 3 essais randomisés portant sur la rééducation sont analysés. Ces études portent sur des pathologies variées (5 essais portent sur des patients porteurs de sclérose en plaques, 4 sur des patients ayant une ataxie dégénérative, 2 sur des patients après accident vasculaire cérébral et 8 portent sur des étiologies variées). Ceci est une limite pour la généralisation des résultats. Ces études pointent l’intérêt d’une évaluation performante de l’ataxie posturale cérébelleuse, à la fois pour la clinique et la recherche. La Scale for the Assessment and Rating of Ataxia (SARA), validée pour évaluer l’ataxie cérébelleuse, comporte 18 points sur 40 sur l’évaluation de l’ataxie posturale cérébelleuse. Simple d’utilisation et possédant de bonnes qualités métrologiques, elle est utile pour suivre l’évolution des patients. Les résultats des études apportent un niveau de preuve modéré sur l’efficacité de la rééducation, en particulier lors d’une ataxie dégénérative ou d’une sclérose en plaques. Il est à noter qu’il n’y a aucun essai randomisé multicentrique portant sur un grand nombre de patients ; c’est un défi pour les années à venir. Le programme de rééducation comportera des exercices intensifs d’équilibre et de coordination. L’utilisation de techniques de rééducation complémentaires tels que la réalité virtuelle, le biofeedback, la marche en suspension sur tapis roulant ou le lestage semble intéressante mais la place de ces techniques nécessitera d’être mieux définie. Les traitements médicamenteux ont été uniquement étudiés sur les ataxies dégénératives. Le niveau de preuve est faible quant à l’efficacité des traitements proposés.
1
English version
1.1
Introduction
For many years, it was thought that postural and balance disorders in cerebellar ataxia were not treatable. However, the results of several recent studies suggest that rehabilitation can relieve postural disorders in patients with cerebellar ataxia. This article is one of the first to review this recent literature. It covers 19 studies of rehabilitation (including three randomized trials) and eight studies of drug treatment. The aetiology of the postural disorders varied; in the rehabilitation studies, degenerative ataxia and multiple sclerosis (MS) were the most frequently studied conditions ( n = 5 studies for each, including the three randomized trials). This may be a source of bias that prevents the results from being extrapolated to other types of cerebellar syndrome. In terms of drug treatments, only degenerative ataxia has been studied.
The results of the studies examined here suggest that quantitative evaluation of postural disorders in cerebellar ataxia has value for both clinical research and clinical practice. We shall successively address the evaluation of postural disorders, rehabilitation, drug treatments and surgical treatments in the context of postural ataxia. Treatment of the underlying disease and any associated impairments (orthopaedic deformations, sensorimotor impairments, cognitive disorders, etc.) will not be discussed here.
1.2
Evaluation of postural disorders in ataxia
Postural disorders in cerebellar ataxia can be evaluated both qualitatively and quantitatively. Qualitative evaluations are based on a precise assessment of clinical symptoms. The combination of postural instability and a staggering, festinating gait is a sign of cerebellar ataxia. Accurate analysis of clinical symptoms is often omitted because of low levels of physician awareness (given that teaching about gait and gait disorders is not a high priority at medical schools) .
The recent observation of ipsilesional and contralesional deviations of the subjective visual vertical (SVV) in patients with acute, unilateral, cerebellar damage suggests that the sense of verticality may be altered in cerebellar diseases. However, it is possible that this disorder is related to concomitant vestibular damage. An evaluation of several modes of perception of the vertical in patients with cerebellar ataxia should be able to resolve this question. In fact, it is widely acknowledged that vestibular disorders can alter the SVV without greatly affecting the subjective haptic and postural verticals . In theory, there is no reason why perception of the postural vertical should be altered in patients with cerebellar damage alone .
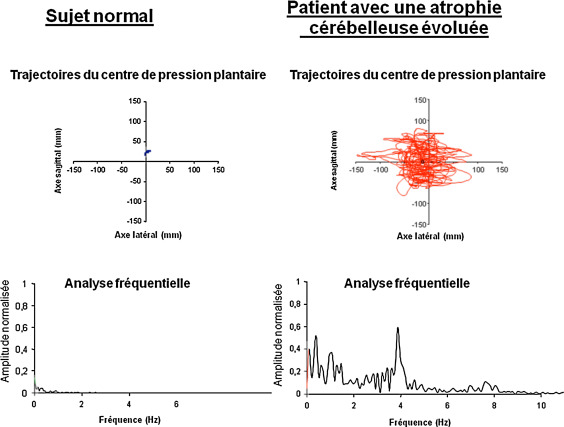
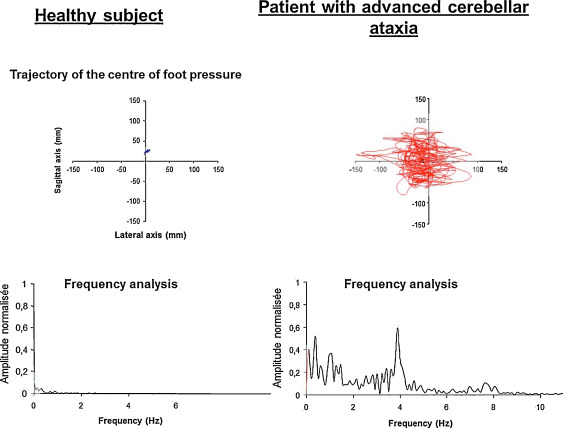
Certain generic evaluations of balance disorders and ordinal scales evaluating the various components of ataxia can be used to quantify the severity of postural disorders in cerebellar ataxia. The generic evaluations of balance include the Berg Balance Scale (BBS), timed standing tests (on one or two legs) and posturography. The latter technique reveals marked oscillations ( Fig. 1 ); a frequency-domain analysis of the posturographic signal shows a peak in the 3 to 5 Hz band that is characteristic of cerebellar tremor. These non-specific evaluations of cerebellar ataxia have been described in detail elsewhere . Generic gait assessments are also useful. In cerebellar ataxia, the basic spatiotemporal gait parameters (stride length, width, duration and direction) are subject to great heterogeneity . The 6-minute Walk Test, gait speed over 10 m and the Timed Up-and-Go Test all provide quantitative estimates of walking ability.
The two most frequently used specific scales for the evaluation of cerebellar ataxia are the recently developed Scale for the Assessment and Rating of Ataxia (SARA) ( Appendix 1 ) and the older International Cooperative Ataxia Rating Scale (ICARS) . Balance is related to 18 of the 40 points in the SARA and 22 of the 100 points in the ICARS. Although the SARA was initially developed and tested for the quantification of ataxia due to spinocerebellar atrophy, it has proven validity in the evaluation of ataxia with other aetiologies . The scale is quick and easy to score and has good metrological qualities . Three items respectively assess balance when sitting, stance and gait. These items are clearly relevant for evaluating balance but have not yet been analyzed separately in clinimetric terms.
These tools have been used for the clinical evaluation of patients (notably for monitoring progress during rehabilitation) and as efficacy criteria in the clinical trials presented below.
1.3
Prevention of falls
Falls are frequent in cerebellar ataxia patients with postural disorders. Fonteyn et al. studied 113 patients with degenerative ataxia over a 1-year period. Eighty-four percent of the patients fell at least once during the study. The traumatic consequences of falls increase with the number of incidents . Fear of falling must also be screened for , since it can accelerate the loss of personal independence. Prevention of falls is thus primordial. To this end, it is necessary to raise awareness among patients and their family, friends and carers. The risk of falling must be explained to all the people concerned. The patient’s living environment may need to be modified, and factors that can aggravate the risk of falls (visual impairments, bowel and bladder disorders, footwear, etc.) must be addressed. A wireless alarm must be provided if the patient is alone all day or part of the day. Automatic fall detection systems are still in the research and development phase . This type of programme has been validated in geriatric populations and patients with neurological disorders but not specifically in patients with cerebellar lesions.
1.4
Rehabilitation of postural disorders in cerebellar ataxia
The cerebellum’s role in motor learning (including postural learning) is now well established . This involvement may therefore limit the effectiveness of rehabilitation programmes in the treatment of balance disorders of cerebellar origin. Nevertheless, patients with cerebellar ataxia have enough learning capacity to benefit from intensive, long-term rehabilitation programmes with good post-treatment efficacy . Fifteen studies have evaluated the efficacy of rehabilitation in cerebellar balance disorders ( Tables 1 and 2 ). These include three randomized trials and a number of case studies with low-quality evidence . We shall describe the studies according to the type of rehabilitation programme used.
| Authors | Aetiology | Number of subjects | Rehabilitation type and intensity | Results |
|---|---|---|---|---|
| Armutlu et al. | MS | 26 | Coordination, balance and walking over uneven ground. One group also tested Johnstone pressure splints on the legs before the rehabilitation sessions 3 times a week for 4 weeks | Improvement in a balance test, gait parameters and the EDSS score in both groups No significant difference between the two groups |
| Miyai et al. | Degenerative ataxia | 42 | Physical therapy focused on balance, gait and muscle strengthening. Occupational therapy focused on activities of daily living and balance. The control group received the same treatment six weeks later 6 sessions a week (totalling 11 hours) for 6 weeks | Improvements in the SARA score, the FIM and gait speed after treatment |
| Widener et al. | MS | 36 | A single session of torso weighting (up to 1.5% of body weight) | Improvements in the 25-Foot Walk Test and the Timed Up-and-Go Test in the torso weighting group |
| Authors | Type of study | Aetiology | Number of subjects | Type and intensity of rehabilitation | Results |
|---|---|---|---|---|---|
| Balliet et al. | Prospective study | Various aetiologies | 5 | Balance and coordination; twice a week for 3 months | Decrease in requirement for walking aids and support during gait |
| Baram and Miller | Prospective study | MS | 14 | Visual feedback during gait; 1 session | Increase in gait speed and stride length during feedback and in a post-treatment evaluation |
| Baram and Miller | Prospective study | MS | 14 | Auditory feedback during gait; 1 session | Increase in gait speed and stride length during feedback and in a post-treatment evaluation |
| Brown et al. | Retrospective study | Various aetiologies | 48 (11 cerebellar ataxia) | Balance and vestibular rehabilitation; 2 to 12 sessions | Improvement in the Dizziness Handicap Inventory score for all subjects but with a smaller change in the cerebellar group |
| Cakrt et al. | Prospective study | Degenerative ataxia | 7 | Tongue electrotactile biofeedback for 2 weeks | Improvement in “eyes shut” posturographic parameters after treatment |
| Cernak et al. | Case study | Stroke | 1 | Treadmill walking with body weight support; 5 times a week for 4 weeks in hospital and then 5 times a week for 4 weeks at home | Improvement of walking abilities |
| Folz and Sinaki | Prospective study | Various aetiologies | 19 | 1 postural rehabilitation session | Improvement in a subjective self-evaluation of balance |
| Freund and Stetts | Prospective study | Traumatic head injury | 1 | Trunk exercises and walking with body weight support; 2 to 3 times a week for 6 weeks | Improvement in the BBS score and gait (Functional Ambulation Category) |
| Gialanella et al. | Retrospective study | Acute phase of stroke | 43 | Conventional rehabilitation; 5 times a week in hospital | Improvement on the Lindmark Scale and in the Trunk Control Test |
| Gill-Body et al. | Case study | Tumour, xanthomatosis | 2 | Balance, walking and coordination exercises; 5 times a week for 6 weeks | Improvement in gait parameters |
| Ilg et al. | Prospective study | Degenerative ataxia | 10 | Kinect ® rehabilitation; 4 supervised sessions a week for 2 weeks, then 6 weeks at home | Decrease in the SARA score (correlated with the intensity of rehabilitation) |
| Ilg et al. | Prospective study | Degenerative ataxia | 16 | Static and dynamic balance, whole body movements, parachute reaction; 3 hours a week for 4 weeks and then self-scheduled | Decrease in the SARA score after rehabilitation, which persisted at 8 weeks and one year |
| Jones et al. | Prospective study | MS | 37 | Balance exercises, and exercises based on activities of daily living; 4 times a week for 2 weeks | Improvements in activities of daily living (the Neuropsychiatric Inventory) and self-reported fatigue and performance levels |
| Perlmutter and Gregory | Case study | Paraneoplastic cerebellar degeneration | 1 | Balance exercises, torso weighting for 3 weeks | Improvement in the FIM (motor items) |
| Stephan et al. | Prospective study | Multiple aetiologies | 4 | Climbing; 2 or 3 times a week for 6 weeks | Improvement in the BBS score in subjects with balance disorders |
| Vaz et al. | Case study | Traumatic head injury | 2 | Gait training on a treadmill; 3 times a week for 4 weeks | Improvement in gait frequency |
In cerebellar ataxia, rehabilitation programmes are based on intensive static and dynamic balance exercises and coordination exercises. The programmes were initially described in case series and have since been evaluated in good-quality, prospective studies (including a randomized trial ).
A prospective study evaluated a rehabilitation programme of this type in 26 patients with ataxic MS : it comprised sessions of coordination exercises, balance exercises and walking over uneven ground three times a week for four weeks. At the end of the programme, balance, gait parameters and the Expanded Disability Status Scale (EDSS) score were improved. This randomized study also assessed the efficacy of 20-minute applications of Johnstone pressure splints (i.e. pressotherapy) prior to the rehabilitation sessions. The goal of pressotherapy is to stimulate the legs’ sensory receptors. However, pressotherapy did not provide any additional benefit. Another prospective study evaluated a rehabilitation programme comprising static and dynamic balance exercises and coordination exercises (with three one-hour sessions a week for four weeks) in 16 patients with degenerative cerebellar disease. An improvement in the SARA score was observed and the effect lasted for up to a year at least .
Lastly, a randomized trial in 42 patients with degenerative cerebellar disease studied the effect of an intensive programme (11 hours a week for 6 weeks) including physical therapy (balance exercises, gait training and muscle strengthening) and occupational therapy focused on balance and activities of daily living. Improvements in the SARA score, gait speed and the Functional Independence Measure (FIM) were noted at 6 weeks, and the effect was still present 24 weeks later.
Multisegment coordination work involves exercises such as climbing. Indeed, one study applied a six-week programme of climbing training to four patients with various conditions . An improvement in the BBS score was observed for the two patients presenting balance disorders.
The use of virtual reality tools also appears to be of value. It requires balance and multisegment coordination, and the game-based aspect facilitates the participants’ adherence to treatment. In a study of 10 patients with degenerative ataxia, use of Kinect ® (a twice-weekly programme supervised for 4 weeks and then self-programmed at home; the games were chosen to specifically work on multisegment coordination, dynamic balance and arm or leg movements towards a target) improved the SARA score (especially when the rehabilitation programme was intense). This finding argues in favour of a dose–effect relationship for rehabilitation.
Torso weighting during rehabilitation has been recommended by Perlmutter and Gregory and was studied in a randomized trial in 36 patients with MS . Torso weighting of 1.5% of body weight improved balance and gait. The mechanism of action of torso weighting has not been established; it may involve an increase in somaesthetic contributions to movement control (including postural control) and a mechanical reduction in the severity of multisegment coordination disorders.
Biofeedback appears to be useful for improving gait and balance; auditory or visual feedback during gait transiently improves gait parameters in patients with MS . Visual feedback was provided, with displacement of a virtual checkerboard (viewed through glasses) as a function of the patient’s head movement. The patient was instructed to walk on the virtual checkerboard’s tiles. Auditory feedback was generated by the patient’s steps. The patient was instructed to walk so that the auditory feedback was as regular as possible. A two-week programme with tongue electrotactile biofeedback (depending on the head position) has been tested in seven patients with cerebellar ataxia. Static balance (as analyzed by posturography) was improved .
Gait rehabilitation on a treadmill (with or without body weight support) may also be of value . Twenty minutes of treadmill training three times a week improved gait parameters in two head injury patients with cerebellar syndrome . Cernak et al. and Freund and Stetts used a treadmill with body weight support for two patients with cerebellar ataxia and who were unable to walk unaided. After the rehabilitation, less assistance with gait was required and the walking distance had increased . These case studies will need to be confirmed by randomized trials. The improvement observed after this type of programme may have been due to the intensive, repeated gait training (i.e. specific task training).
Although the use of walking aids to compensate for balance disorders has not been specifically studied in patients with cerebellar ataxia, the use of a walking stick or walking frame can improve postural stability when balance is poor. However, the use of walking aids is difficult when cerebellar syndrome also affects arm movement. Assistance and training in the use of walking aids are essential because inappropriate use is even associated with an increased risk of falls .
The fact that postural disorders in cerebellar ataxia can have many different aetiologies means that the above-mentioned findings cannot necessarily be extrapolated to other types of cerebellar ataxia. Furthermore, cerebellar syndrome is often combined with other impairments that give rise to balance disorders. The effect of a rehabilitation programme on balance may be due to an improvement in the postural disorder related to cerebellar ataxia and/or other impairments. Intensive programmes (with static and dynamic balance exercises and coordination exercises) have been analyzed in methodologically robust studies of patients with degenerative ataxia and MS; the effect of this type of programme on postural disorders must now be studied in cerebellar ataxia due to other aetiologies.
1.5
Drug treatments for postural disorders in cerebellar ataxia
To date, drug treatment has only been tested in the context of hereditary cerebellar ataxia . Efficacy is generally low and has mainly been documented for the serotonin precursor oxitriptan/5-hydroxytryptophan. In two randomized, placebo-controlled trials, oxitriptan was found to be efficacious for controlling kinetic and static cerebellar syndrome in Friedreich’s ataxia . A case study also reported on the efficacy of oxitriptan in attenuation of cerebellar ataxia . The antioxidant idebenone (an analogue of Q10 coenzyme) was found to have an effect on the myocardial component of Friedreich’s ataxia . Idebenone’s effects on neurological symptoms appear to be moderate, and high doses are required . The improvements concerned nystagmus, dysarthria and, to a lesser extent, postural disorders . Amantadine has a dopaminergic action. In three case studies and one randomized trial, this medication improved gait and independence in the activities of daily living (writing, dressing, etc.) – possibly by improving coordination . The level of evidence for the efficacy of other compounds is low.
1.6
Deep brain stimulation
Bilateral deep brain stimulation (DBS) of the ventral oralis posterior thalamic nuclei and the ventral intermedial nuclei has been reported in only one case . In a patient with spinocerebellar ataxia type 2 and severe tremor, DBS markedly improved sitting and standing postures. The relief of tremor may have been due to stimulation of the nearby cerebellar thalamic afferents. This is an exploratory study, the results of which must be confirmed.
1.7
Conclusion
Postural disorders in cerebellar ataxia constitute a major cause of poor balance. Prior evaluation of cerebellar ataxia is essential for monitoring a patient’s clinical progress and validating therapeutic efficacy in clinical trials. This evaluation involves non-specific tools for balance assessment (the BBS, posturography and basic spatiotemporal gait parameters) and ataxia scales (of which the SARA is most frequently used but which are not focused on postural disorders). Few pharmacological or surgical treatments are available. Intensive rehabilitation (with balance and coordination exercises) improves the patients’ functional abilities (level of proof: moderate). Although techniques such as virtual reality, biofeedback, treadmill exercises with supported body weight and torso weighting appear to be of value, their specific efficacy has yet to be characterized. This body of literature is limited by the wide range of underlying conditions studied and methodological weaknesses (small sample sizes, poorly described rehabilitation protocols, etc.). There are no published data from large, multicentre randomized trials; this will be the challenge for the coming years. Again, the intensity, duration and content of the rehabilitation programmes will have to be better defined.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Appendix 1
Assessment of postural disorders in cerebellar ataxia: items 1 to 3 of the Scale for the Assessment and Rating of Ataxia (SARA)
1) Gait
The subject is asked to walk parallel to a wall, then to turn around and to walk back in tandem (heels to toes) without support:
0 Normal, no difficulty in walking, turning and walking tandem (up to one misstep allowed).
1 Slight difficulties, only visible when walking 10 consecutive steps in tandem.
2 Clearly abnormal, tandem walking >10 steps not possible.
3 Considerable staggering, difficulties in half-turn, but without support.
4 Marked staggering, intermittent support of the wall required.
5 Severe staggering, permanent support of one stick or light support by one arm required.
6 Walking >10 m only with strong support (two special sticks or stroller or accompanying person).
7 Walking <10 m only with strong support (two special sticks or stroller or accompanying person).
8 Unable to walk, even supported.
2) Stance
The subject is asked to stand:
- 1.
in natural position;
- 2.
with feet together in parallel (big toes touching each other);
- 3.
in tandem (both feet on one line, no space between heel and toe).
The subject does not wear shoes, eyes are open. For each condition, three trials are allowed. The best trial is rated:
0 Normal, able to stand in tandem for >10 s.
1 Able to stand with feet together without sway, but not in tandem for >10 s.
2 Able to stand with feet together for >10 s, but only with sway.
3 Able to stand for >10 s without support in natural position, but not with feet together.
4 Able to stand for >10 s in natural position only with intermittent support.
5 Able to stand >10 s in natural position only with constant support of one arm.
6 Unable to stand for >10 s even with constant support of one arm.
3) Sitting
The subject is asked to sit on an examination bed without support of feet, eyes open and arms outstretched to the front:
0 Normal, no difficulties sitting >10 s in this position.
1 Slight difficulties, intermittent sway.
2 Constant sway, but able to sit >10 s without support.
3 Able to sit for >10 s only with intermittent support.
4 Unable to sit for >10 s without continuous support.
2
Version française
2.1
Introduction
L’ataxie posturale cérébelleuse a longtemps eu la réputation de ne pas être accessible au traitement. Plusieurs études récentes suggèrent au contraire que les patients qui ont une ataxie posturale cérébelleuse peuvent être améliorés par la rééducation. Cet article est l’une des premières synthèses de cette littérature, comprenant 19 articles portant sur la rééducation, dont 3 essais randomisés et huit articles portant sur le traitement médicamenteux. Les étiologies des ataxies cérébelleuses posturales sont variées dans les études analysées. Dans les études portant sur la rééducation, les pathologies les mieux analysées sont l’ataxie dégénérative et la sclérose en plaques (SEP), avec 5 études chacune, dont les 3 essais randomisés. Ceci pourra être un biais pour la généralisation des résultats à l’ensemble des ataxies posturales cérébelleuses. Concernant les traitements médicamenteux, seule l’ataxie dégénérative a été analysée.
Ces études pointent l’intérêt d’une évaluation quantifiée de l’ataxie posturale cérébelleuse, à la fois pour la clinique et la recherche. Nous aborderons successivement l’évaluation, la rééducation puis les traitements médicamenteux et chirurgicaux de l’ataxie posturale. Le traitement de la maladie causale, de même que le traitement des éventuels déficits associés (déformations orthopédiques, déficits moteurs ou sensoriels, troubles cognitifs…) ne seront pas abordés ici.
2.2
Évaluation de l’ataxie posturale
L’ataxie posturale cérébelleuse est évaluée de façon qualitative et quantitative. L’évaluation qualitative est basée sur une évaluation sémiologique précise. Une instabilité posturale associée à une démarche ébrieuse et festonnante signe l’ataxie cérébelleuse. Cette analyse sémiologique précise est souvent omise, et méconnue de nombreux médecins du fait d’une insuffisance de l’enseignement de la marche et ses troubles en faculté de médecine .
La question d’une éventuelle altération du sens de verticalité dans les pathologies cérébelleuses a été récemment posée par la mise en évidence d’une déviation (ipsi- ou contralésionnelle) de la verticale visuelle subjective (VVS) lors d’atteintes cérébelleuses unilatérales aiguës . Ce trouble pourrait n’être qu’une manifestation vestibulaire liée à une atteinte vestibulaire concomitante. L’évaluation de plusieurs modalités perceptives de la verticale chez les patients cérébelleux permettrait de répondre à cette question. En effet il est bien admis que la verticale visuelle peut être altérée par des troubles vestibulaires alors que les verticales haptiques et posturales sont peu altérées en pathologie vestibulaire . Il n’y a pas d’argument théorique pour prédire une perception altérée de la verticale posturale lors d’une atteinte purement cérébelleuse .
Des évaluations génériques des troubles de l’équilibre et des échelles ordinales évaluant les différentes composantes de l’ataxie cérébelleuse permettent de quantifier la sévérité de l’ataxie posturale cérébelleuse. Les évaluations génériques de l’équilibre pour l’évaluation de l’ataxie posturale cérébelleuse peuvent faire appel à la Berg Balance Scale (BBS), au temps de maintien d’une posture donnée (équilibre uni- ou bipodal) et à la posturographie. La posturographie retrouve des oscillations importantes ( Fig. 1 ) ; l’analyse fréquentielle du signal posturographique montre un pic de fréquence dans une bande de 3 à 5 Hz caractéristique de l’ataxie cérébelleuse qui correspond au tremblement cérébelleux. Ces évaluations non spécifiques de l’ataxie cérébelleuse sont détaillées ailleurs . Les évaluations génériques de la marche sont également intéressantes. Les paramètres spatiotemporaux élémentaires de la marche (longueur, largeur, durée et direction des pas) de l’ataxie cérébelleuse sont surtout caractérisés par une grande variabilité . Le test de marche des 6 minutes, la vitesse de marche sur 10 m et le Timed Up-and-Go Test permettent une évaluation quantifiée des capacités de déambulation.