Abstract
Objective
This study aimed to evaluate the outcome of the anterior mini-open approach of the hip for femoroacetabular impingement (FAI) at one year post-surgery by use of questionnaires, functional capacity tests and biomechanical studies.
Design
This is a case series prospective study. A total of 14 patients diagnosed of FAI were included. Patients were classified according to Tönnis scale. Hip joint mobility, Faber distance, pain levels (assessed on a visual analogic scale [VAS]), 6-minute walking test (6MWT), Timed up & go test (TUGT), Stairs climbing test, Lequesne functional index, and gait analysis were assessed prior to and 12 months after surgery.
Results
Pain significantly improved following surgery. An improvement of 80% or more was found in 6 patients (42.85% of cases). Improvements were also seen in time support of the affected limb and in the braking force of the contralateral limb, although these are not clinically significant. No statistically significant changes were seen in functional capacity tests. At 12 months after surgery, meralgia paraesthetica presented in 3 patients (21.4%), and a total hip arthroplasty was performed in 1 patient.
Conclusions
There was significant reduction in pain intensity 12 months following mini-open approach for FAI compared to preoperatively. Improvement in gait analysis and functional capacity was also seen, although not statistically significant.
1
Introduction
Femoroacetabular impingement (FAI) was described by Ganz et al. as a condition caused by an abnormal contact between the proximal femur and the acetabular rim, especially in the extremes of range of motion. This can cause chondral and acetabular labrum injuries. Three types have been described (pincer, cam and mixed) , and all have morphological variants on the hip. The condition of FAI has been recognized as a common cause of hip pain and osteoarthritis in young adults . With improved imaging techniques presently available, the diagnosis of FAI and labral injury has increased .
After surgical treatment of FAI it is important to assess the anatomical and functional outcome of the hip. This can be done using biomechanical assessment tests as well as functional and pain scales. The advantage of biomechanical assessment is that it allows an objective measurement of changes in patients.
There are currently few published studies that evaluate prospective short and long-term results for FAI . This study is the first to evaluate the outcome of surgery using biomechanical and functional testing in the same cohort.
The purpose of this study is to evaluate the outcome of patients who underwent FAI surgery by mini-anterior approach of the hip, by use of questionnaires, tests of functional capacity and biomechanical studies.
2
Materials and methods
A prospective study was designed to assess functional results of FAI surgical treatment in active patients at a minimum of one year following surgical intervention. The diagnosis of FAI was confirmed clinically and by radiology. The radiological investigations performed were plain X-rays (AP pelvis, AP and axial Dunn views of the affected hip) as well as magnetic resonance arthrogram (MRA). All patients undergoing treatment for FAI at our institution between November 2009 and January 2012 (total of 48) were assessed to determine whether they were eligible for inclusion in the study.
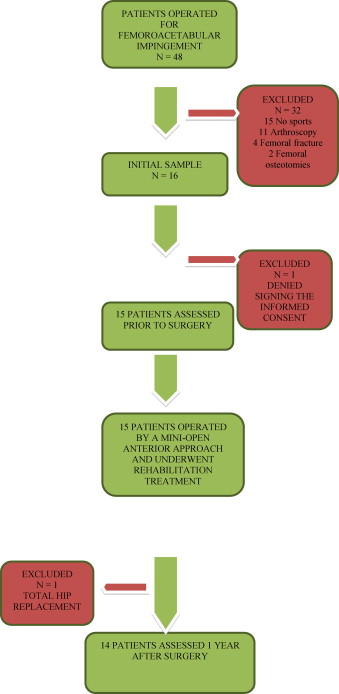
The inclusion criteria for the study were patients with a primary diagnosis of FAI operated by an anterior mini-open approach and functional requirements (measured by sports practice). The exclusion criteria were signs of osteoarthritis (Tönnis 2 and above), insignificant level of sports practice and surgical treatment differing from anterior mini-open approach of the hip (i.e. surgical hip dislocation or arthroscopy). From the original cohort of 48 patients, 14 were eligible for inclusion. Of the 34 patients excluded, 15 denied any sports practice, 11 were treated by arthroscopy, four had femoral fractures in the past, two underwent femoral osteotomies during childhood, one patient declined to sign the informed consent and another had to be revised and underwent surgery for total hip replacement 8 months following the index FAI surgery ( Fig. 1 ). All patients included in the study signed the informed consent meeting the principles of the WMA Declaration of Helsinki and approval was obtained from the Ethics Committee in our institution.
2.1
Procedure and rehabilitation
All procedures were performed by a single surgeon. The procedure involved femoral osteoplasty by means of an anterior mini-open approach. All patients underwent rehabilitation following the same protocol established in our health center.
2.1.1
Surgical technique
The procedure consisted of an anterior mini-open incision of 6–8 cm following the description of Ribas et al. . After capsulotomy is performed full visualization of the joint is obtained without any muscle detachment. The labrum and cartilage were assessed for pathologic changes with intermittent use of traction. When labral tears are identified, labral debridement and partial excision are performed to treat the lesion. In our cases no significant chondral lesions were found to warrant operative treatment. No cases needed acetabular resection and impingement was corrected by different amounts of femoral osteochondroplasty. The capsule and ligaments are closed and the incision sutured leaving a suction drain for the first 24 hours postoperatively. DVT prophylaxis was given as per protocol during 10 days.
2.1.2
Rehabilitation treatment
The rehabilitation protocol in our hospital for patients who undergo surgery for FAI without labral repair is as follows:
- •
during the first 3 weeks post-surgery: ambulation with 2 crutches, active and auto-assisted flexo-extension hip movements, to gain range of motion; isometric quadriceps and gluteus exercises, to gain muscular strength; seated proprioception exercises;
- •
after 3 weeks post-surgery: isotonic hip muscles exercises, to gain muscular strength; bipodal and unipodal proprioception exercises, progressively.
2.2
Variables
After designing a protocol specifically for the study, the patients were assessed before the surgical operation and at 12 months postoperatively.
At the time of the first assessment demographic variables were collected: gender, age, profession and sport(s) participated. Pain characteristics, including onset (acute or chronic), laterality and any previous recalled trauma were registered. The past medical history and any predisposing hip conditions for FAI like Legg Calve Perthes, Developmental Dysplasia of the hip (DDH), Slipped Upper Femoral Epiphysis (SUFE), Protrusio Acetabuli and Retroverted acetabulum were registered. By means of preoperative plain films the presence of the crossover sign, coxa profunda or protrusio acetabuli were assessed, all of them predisposing conditions for Pincer type FAI; as well as the Pistol grip sign, Cervical-Diaphyseal Angle (CDA), Alpha Angle (AA), Head-neck offset (HNO) and Modified proximal femoral angle (MPFA), predisposing for Cam type FAI. Every patient was classified according to Tönnis classification. MRI arthrogram was studied to rule out any further pathologic disease paying attention to the labrum and articular cartilage.
The main variable in this study was the pain level assessed on VAS. Secondary variables were hip range of motion, measurements of functional capacity, Lequesne functional index and gait analysis variables.
The intra and postoperative complications were noted as well as whether any further surgery was required within the first 12 months following the procedure and time until return to sports.
2.2.1
Pain measurement
To assess the subjective intensity of pain the VAS was used, which is considered to be a valid and reliable element to assess the degree of pain. It ranges from 0 (absence of pain) to 10 (unbearable pain). Depending on the pain intensity it is classified into 3 categories: 0–3, mild pain; 4–6, moderate pain; 7–10, intense pain .
2.2.2
Hip range of motion
On physical examination, flexion, extension, abduction, adduction, internal and external rotation at 90° of flexion, as well as impingement test and Faber distance were recorded for the affected and non affected hips. The Faber test or distance is measured with the patient lying supine and the affected extremity placed in the figure-four position of flexion, abduction, and external rotation. Gentle downward force is then applied to the affected leg while a stabilizing force is applied to the contralateral side of the pelvis. The vertical distance from the lateral aspect of the knee to the examination table is recorded . Every examination was performed by the same team using an electronic goniometer and every patient was always assessed by the same examiner for consistency.
2.3
Measurement of functional capacity
2.3.1
Six-minute walking test
The Six-minute walking test (6MWT) is the distance the patient is able to walk in a 6-minute period. This test was initially considered a valid test to measure endurance but more recently considered to measure motion and function in a widest sense related with activities of daily living . The 6MWT in our study was performed in a corridor marking 24 meters in total. Patients walked at a “comfortable pace”, were advised not to talk during the test, and were notified of the remaining minutes. When 6 minutes was reached the total distance walked was recorded.
2.3.2
Timed up and go
The Timed up and go (TUG) is a test that records the time required for the patient to stand up from a chair with armrest, walk 3 meters, turn round and walk back to the chair and sit down. The patients walked around a small cone placed at the 3 meters landmark. The participants were instructed to proceed “as fast as possible with security and without running” .
2.3.3
Stairs climbing test
The Stairs climbing test (SCT) is a measurement of the time spent by a participant to walk up and down stairs made of twelve steps each of a height of 18 cm and a depth of 28 cm . The patients were advised to complete the test as fast as they felt safe and comfortable. They were allowed to use the stairs’ handrail as needed, although encouraged to use only their legs.
2.4
Questionnaire
2.4.1
Lequesne functional index for hip osteoarthritis
The Lequesne functional index is a questionnaire that measures the functional impact of hip and knee osteoarthritis. It can also be used to evaluate the effectiveness of therapeutic interventions. It consists of 10 items in three different sections: pain or discomfort, maximum walked distance, and daily activities. Every section has a score range of 0 to 8. The total score of this index ranges from 0 to 24. Depending on the severity of osteoarthritis, the result might be 0 points: unaffected, 1–3 points: mild, 5–7 points: moderate, 8–10 points: severe and 11–13: very severe; scores of 14 points and higher: extremely severe .
2.5
Biomechanical tests
2.5.1
Gait analysis
The analysis was conducted with the NedAMH/IBV system. This system, used with the Dinascan600/IBV dinamometric platform, biomechanically analyses human gait to functionally evaluate the ability and regularity of the patient’s gait pattern. The following variables were collected: gait speed (m/s 2 ), support time (seconds), and braking force (Nw). The platform Dinascan 600/IBV (Instituto Biomecanico de Valencia. Universidad Politecnica de Valencia. Camino de Vera s/n 46022 Valencia, Spain) is formed by an active rectangular surface measuring 600 × 370 mm with 4 extensiometric anchors in each corner, embeded in the floor, equipped with an A-D converter and controlled by 32 bit applications developed on LabWindows under C++ NedAMH/IBV and NedSVE/IBV interface. NedAMH/IBV is a software application to assist the specialist in biomechanical assessment of the human gait. A functional assessment of the capacity and regularity of gait is compared to normal standards. This system allows for analysis of ground reaction forces and moments performed by the individual on the floor during any human activity.
2.6
Statistical study
For the descriptive analysis, means (standard deviations [SD]) were used for quantitative variables and percentages for qualitative variables. The non-parametric Mann-Whitney U test was used to analyze the association between dependent quantitative variables, whereas the Wilcoxon test was used to study the association between independent quantitative variables. The adjustment was done taking the prognostic value of the variable when the bivariant analysis presented a P < 0.05. Unless otherwise indicated, the statistical significance of P < 0.05 was established.
2
Materials and methods
A prospective study was designed to assess functional results of FAI surgical treatment in active patients at a minimum of one year following surgical intervention. The diagnosis of FAI was confirmed clinically and by radiology. The radiological investigations performed were plain X-rays (AP pelvis, AP and axial Dunn views of the affected hip) as well as magnetic resonance arthrogram (MRA). All patients undergoing treatment for FAI at our institution between November 2009 and January 2012 (total of 48) were assessed to determine whether they were eligible for inclusion in the study.
The inclusion criteria for the study were patients with a primary diagnosis of FAI operated by an anterior mini-open approach and functional requirements (measured by sports practice). The exclusion criteria were signs of osteoarthritis (Tönnis 2 and above), insignificant level of sports practice and surgical treatment differing from anterior mini-open approach of the hip (i.e. surgical hip dislocation or arthroscopy). From the original cohort of 48 patients, 14 were eligible for inclusion. Of the 34 patients excluded, 15 denied any sports practice, 11 were treated by arthroscopy, four had femoral fractures in the past, two underwent femoral osteotomies during childhood, one patient declined to sign the informed consent and another had to be revised and underwent surgery for total hip replacement 8 months following the index FAI surgery ( Fig. 1 ). All patients included in the study signed the informed consent meeting the principles of the WMA Declaration of Helsinki and approval was obtained from the Ethics Committee in our institution.
2.1
Procedure and rehabilitation
All procedures were performed by a single surgeon. The procedure involved femoral osteoplasty by means of an anterior mini-open approach. All patients underwent rehabilitation following the same protocol established in our health center.
2.1.1
Surgical technique
The procedure consisted of an anterior mini-open incision of 6–8 cm following the description of Ribas et al. . After capsulotomy is performed full visualization of the joint is obtained without any muscle detachment. The labrum and cartilage were assessed for pathologic changes with intermittent use of traction. When labral tears are identified, labral debridement and partial excision are performed to treat the lesion. In our cases no significant chondral lesions were found to warrant operative treatment. No cases needed acetabular resection and impingement was corrected by different amounts of femoral osteochondroplasty. The capsule and ligaments are closed and the incision sutured leaving a suction drain for the first 24 hours postoperatively. DVT prophylaxis was given as per protocol during 10 days.
2.1.2
Rehabilitation treatment
The rehabilitation protocol in our hospital for patients who undergo surgery for FAI without labral repair is as follows:
- •
during the first 3 weeks post-surgery: ambulation with 2 crutches, active and auto-assisted flexo-extension hip movements, to gain range of motion; isometric quadriceps and gluteus exercises, to gain muscular strength; seated proprioception exercises;
- •
after 3 weeks post-surgery: isotonic hip muscles exercises, to gain muscular strength; bipodal and unipodal proprioception exercises, progressively.
2.2
Variables
After designing a protocol specifically for the study, the patients were assessed before the surgical operation and at 12 months postoperatively.
At the time of the first assessment demographic variables were collected: gender, age, profession and sport(s) participated. Pain characteristics, including onset (acute or chronic), laterality and any previous recalled trauma were registered. The past medical history and any predisposing hip conditions for FAI like Legg Calve Perthes, Developmental Dysplasia of the hip (DDH), Slipped Upper Femoral Epiphysis (SUFE), Protrusio Acetabuli and Retroverted acetabulum were registered. By means of preoperative plain films the presence of the crossover sign, coxa profunda or protrusio acetabuli were assessed, all of them predisposing conditions for Pincer type FAI; as well as the Pistol grip sign, Cervical-Diaphyseal Angle (CDA), Alpha Angle (AA), Head-neck offset (HNO) and Modified proximal femoral angle (MPFA), predisposing for Cam type FAI. Every patient was classified according to Tönnis classification. MRI arthrogram was studied to rule out any further pathologic disease paying attention to the labrum and articular cartilage.
The main variable in this study was the pain level assessed on VAS. Secondary variables were hip range of motion, measurements of functional capacity, Lequesne functional index and gait analysis variables.
The intra and postoperative complications were noted as well as whether any further surgery was required within the first 12 months following the procedure and time until return to sports.
2.2.1
Pain measurement
To assess the subjective intensity of pain the VAS was used, which is considered to be a valid and reliable element to assess the degree of pain. It ranges from 0 (absence of pain) to 10 (unbearable pain). Depending on the pain intensity it is classified into 3 categories: 0–3, mild pain; 4–6, moderate pain; 7–10, intense pain .
2.2.2
Hip range of motion
On physical examination, flexion, extension, abduction, adduction, internal and external rotation at 90° of flexion, as well as impingement test and Faber distance were recorded for the affected and non affected hips. The Faber test or distance is measured with the patient lying supine and the affected extremity placed in the figure-four position of flexion, abduction, and external rotation. Gentle downward force is then applied to the affected leg while a stabilizing force is applied to the contralateral side of the pelvis. The vertical distance from the lateral aspect of the knee to the examination table is recorded . Every examination was performed by the same team using an electronic goniometer and every patient was always assessed by the same examiner for consistency.
2.3
Measurement of functional capacity
2.3.1
Six-minute walking test
The Six-minute walking test (6MWT) is the distance the patient is able to walk in a 6-minute period. This test was initially considered a valid test to measure endurance but more recently considered to measure motion and function in a widest sense related with activities of daily living . The 6MWT in our study was performed in a corridor marking 24 meters in total. Patients walked at a “comfortable pace”, were advised not to talk during the test, and were notified of the remaining minutes. When 6 minutes was reached the total distance walked was recorded.
2.3.2
Timed up and go
The Timed up and go (TUG) is a test that records the time required for the patient to stand up from a chair with armrest, walk 3 meters, turn round and walk back to the chair and sit down. The patients walked around a small cone placed at the 3 meters landmark. The participants were instructed to proceed “as fast as possible with security and without running” .
2.3.3
Stairs climbing test
The Stairs climbing test (SCT) is a measurement of the time spent by a participant to walk up and down stairs made of twelve steps each of a height of 18 cm and a depth of 28 cm . The patients were advised to complete the test as fast as they felt safe and comfortable. They were allowed to use the stairs’ handrail as needed, although encouraged to use only their legs.
2.4
Questionnaire
2.4.1
Lequesne functional index for hip osteoarthritis
The Lequesne functional index is a questionnaire that measures the functional impact of hip and knee osteoarthritis. It can also be used to evaluate the effectiveness of therapeutic interventions. It consists of 10 items in three different sections: pain or discomfort, maximum walked distance, and daily activities. Every section has a score range of 0 to 8. The total score of this index ranges from 0 to 24. Depending on the severity of osteoarthritis, the result might be 0 points: unaffected, 1–3 points: mild, 5–7 points: moderate, 8–10 points: severe and 11–13: very severe; scores of 14 points and higher: extremely severe .
2.5
Biomechanical tests
2.5.1
Gait analysis
The analysis was conducted with the NedAMH/IBV system. This system, used with the Dinascan600/IBV dinamometric platform, biomechanically analyses human gait to functionally evaluate the ability and regularity of the patient’s gait pattern. The following variables were collected: gait speed (m/s 2 ), support time (seconds), and braking force (Nw). The platform Dinascan 600/IBV (Instituto Biomecanico de Valencia. Universidad Politecnica de Valencia. Camino de Vera s/n 46022 Valencia, Spain) is formed by an active rectangular surface measuring 600 × 370 mm with 4 extensiometric anchors in each corner, embeded in the floor, equipped with an A-D converter and controlled by 32 bit applications developed on LabWindows under C++ NedAMH/IBV and NedSVE/IBV interface. NedAMH/IBV is a software application to assist the specialist in biomechanical assessment of the human gait. A functional assessment of the capacity and regularity of gait is compared to normal standards. This system allows for analysis of ground reaction forces and moments performed by the individual on the floor during any human activity.
2.6
Statistical study
For the descriptive analysis, means (standard deviations [SD]) were used for quantitative variables and percentages for qualitative variables. The non-parametric Mann-Whitney U test was used to analyze the association between dependent quantitative variables, whereas the Wilcoxon test was used to study the association between independent quantitative variables. The adjustment was done taking the prognostic value of the variable when the bivariant analysis presented a P < 0.05. Unless otherwise indicated, the statistical significance of P < 0.05 was established.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






