Tendonitis of the Wrist and Hand
General Information
Tendonitis of the hand and wrist is a common upper extremity disorder. Tendonitis should not be used as a “waste basket” term to diagnose generalized wrist and hand pain, but should refer to a specific anatomic site. Three common tendon afflictions are tenosynovitis, tenovaginitis, and tendinosis. Any tendon or group of tendons that have a synovial lining can become inflamed (tenosynovitis). A tendon can be constricted by a tight covering or sheath (tenovaginitis). A tendon origin or insertion can become diseased or degenerated secondary to age, poor blood supply, friction, or overuse (tendinosis). The three conditions may occur as independent entities or in combination.
De Quervain’s Tendonitis
De Quervain’s tendonitis refers to involvement of the tendons of the first dorsal compartment (abductor pollicis longus [APL] and the extensor pollicis brevis [EPB] tendons). Within the compartment, the APL has multiple tendinous slips and is often separated from the EPB by a septum. De Quervain’s tendonitis is associated with repetitive tasks involving the thumb and wrist, as well as with pregnancy and childcare. Patients have tenderness over the first dorsal compartment and pain during a Finkelstein’s test (asking the patient to fully flex the thumb and passively move the wrist into ulnar deviation). This maneuver is positive if it reproduces the patient’s discomfort. Typically, active thumb abduction and extension against resistance is painful. The differential diagnosis for radial-sided wrist pain includes thumb carpometacarpal or scaphotrapezoid joint arthritis, scaphoid fracture or nonunion, radiocarpal arthritis, radial styloid fracture, and radial sensory neuritis (Wartenberg’s syndrome). An x-ray of the wrist should be obtained if there is any question about the diagnosis.
Table 1. Principles of tendon sheath injection | ||
|---|---|---|
|
Treatment
Nonsurgical treatment of De Quervain’s tendonitis includes rest, antiinflammatory medication, stretching exercises, and corticosteroid injections. A forearm-based thumb spica splint immobilizes the APL and EPB tendons. Cortico steroid injection is used to deliver a bolus of antiinflammatory medication to the site of inflammation (Table 1). A steroid preparation that is partially or totally water-soluble is recommended to limit the local effects of steroid deposition; subcutaneous fat atrophy, and cutaneous depigmentation. In addition, passing the needle to the radius and pulling back slightly ensures the injection is deep within the sheath (Fig. 1). Persistent pain that is refractory to nonsurgical treatment warrants surgical release of the extensor compartment by incising the overlying retinaculum.
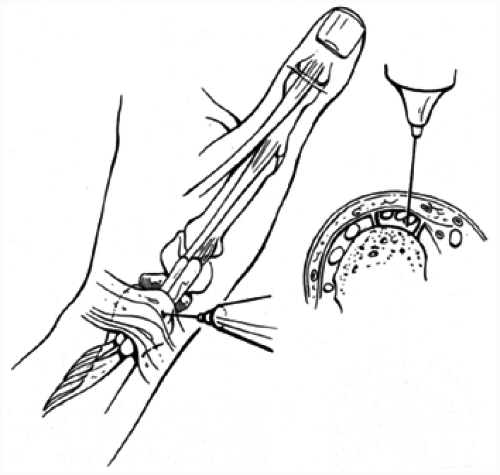 FIG. 1. Intracompartmental injection for De Quervain’s tendonitis is placed just proximal to the radial styloid. Tendons are palpated by having patient perform a resisted thumb abduction maneuver and site is marked. The 25-gauge needle is placed through the tendon to bone, and then pulled back slightly. The medication injection then proceeds without much resistance.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|



