Intrathecal baclofen (ITB) infusion is a common treatment for patients with diffuse lower-limb and truncal spasticity after central nervous system injury (spinal cord or traumatic brain injury, stroke, multiple sclerosis and cerebral palsy) . An acute treatment disruption, caused by a pump or catheter dysfunction, can cause a withdrawal syndrome. Clinical features of baclofen withdrawal syndrome (BWS) are well described, and the severity can range from pruritus and delirium to multi-system organ failure leading to death . Severe manifestations of BWS such as reversible cardiomyopathy and cardiac arrest have been described, with few clues as to the pathophysiology. Nonetheless, we report the first case of a specific, reversible acute cardiac failure, Takotsubo syndrome (TTS), which gives insights into the putative mechanisms of acute cardiac failure in BWS.
A 55-year-old man, regularly followed for posttraumatic complete thoracic level 2 (Th2) paraplegia (American Spinal Injury Association Impairment Scale-A), underwent surgery to replace an end-of-life intrathecal baclofen pump (Medtronic, Dublin, Ireland). He was admitted to our physical medicine and rehabilitation department 1 month later for progressive diffuse supralesional pruritus that had started 2 days before, general discomfort, and sublesional spasms in the lower limbs for the last 24 h, which highly suggested BWS. Abdominal radiography revealed that the distal extremity of the catheter had moved out of the intrathecal space ( Fig. 1 A ). Despite the administration of oral baclofen (30 mg 3 times/day) and benzodiazepine (diazepam, 5 mg 3 times/day), withdrawal symptoms did not disappear.
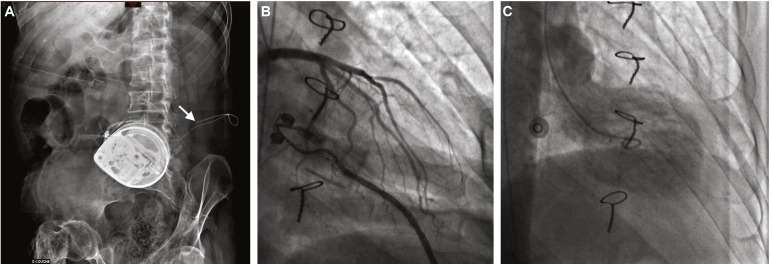
Three days after admission, the patient reported an acute left chest pain. Heart rate was 90 bpm and arterial blood pressure 160/100 mmHg (baseline 65 bpm and 90/60 mmHg). Electrocardiography (ECG) revealed elevated ST segment in inferior and apical territories, with troponin elevation up to 3 ng/mL (normally < 0.05 ng/mL). The patient was transferred to a cardiology intensive care unit; coronary angiography did not reveal any artery abnormalities, but ventriculography revealed abnormal left ventricle apical kinetics with a ballooning aspect that was compatible with TTS ( Fig. 1 B, C). Transthoracic echocardiography revealed left ventricular ejection fraction 35%, with apical and median kinetic abnormalities. The patient received conversion enzyme inhibitors and beta-blockers, which slightly improved the left cardiac failure, with surgical replacement of the intrathecal catheter the following week. He fully recovered after restoration of ITB delivery, and cardiogenic drugs were progressively withdrawn. The course of clinical events is summarized in Fig. 2 .
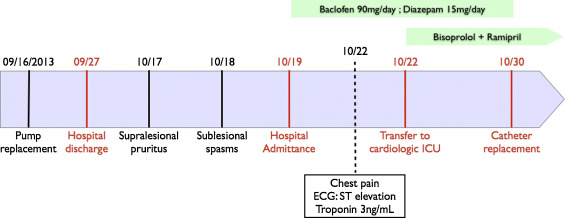
Because we ruled out another possible etiology for the TTS (no specific cardiovascular risk factor and negative toxicologic screening) and restoration of drug delivery improved the left ventricular function, we concluded acute reversible cardiomyopathy secondary to baclofen withdrawal.
TTS is a particular reversible cardiomyopathy named after the shape of an antique Japanese amphora (two-handled jug) . This morphologic description is due to kinetic abnormalities in apical territories of the left ventricle. The clinical presentation mimics acute anterior coronary syndrome, with ST segment elevation on ECG and high cardiac biomarker levels but no coronary lesions on cardiac angiography. The pathophysiology and underlying mechanisms are not well described. However, adrenergic mechanisms could explain this idiopathic syndrome . In a systematic review by Gianni, 74% of patients with TTS had elevated catecholamine plasma level, 2 to 3 times higher than that for patients presenting at the emergency room for myocardial infarction . Furthermore, β2-adrenoreceptors, predominant on apical territories, can switch from Gs to Gi protein coupling at high epinephrine concentrations, thereby resulting in a loss of myocyte contraction . Adrenergic mechanisms could also lead to microvascular coronary dysfunction, which is controversial .
Baclofen, a GABAb receptor agonist commonly prescribed to treat spasticity, acts by blocking some spinal cord reflexes. Recent findings have implicated GABA receptors in modulating spinal cord sympathetic outflow, with a direct effect on sympathetic preganglionic neurons . Wang et al. first demonstrated that GABA receptor agonists could elicit a tonic inhibition of preganglionic cells within the inter-mediolateral column . The same team secondarily showed that specific GABAb-receptor activation with small doses of baclofen could modulate the postsynaptic response in sympathetic preganglionic neurons with different responses . From their findings, at high thoracic spinal levels (cardiac sympathetic innervation from Th1 to Th4), GABAb activation by baclofen could decrease the adrenergic outflow.
From the excitatory–inhibitory ratio model , chronic ITB infusion could modify the sympathetic/parasympathetic (∑/p∑) balance. Thus, the acute discontinuation of ITB could generate a shift toward a high ∑/p∑ ratio, thereby leading to acute cardiomyopathy. BWS never occurs after ITB trials or within the first 3 months after pump implantation, and Mathias et al., in describing a high response to low-dose norepinephrine, first hypothesized that spinal cord injury could sensitize peripheral adrenergic receptors . Another hypothesis could be the potentiation of hypersensitivity of central adrenergic receptors, well described for substance P and pruritus . Hence, Takotsubo cardiomyopathy could have occurred in our patient by direct stimulation of sublesional cardiac innervation at Th4, thereby leading to apical kinetic dysfunction of the myocardium or secondarily to myocardial adrenoreceptor sensitization, overwhelmed by an acute overactivation of the sympathetic celiac plexus and adrenal secretions.
Unbalanced ∑/p∑ ratio may result from acute BWS in patients with complete spinal cord injury whose spasticity is treated with intrathecal infusion. Systematic ECG should be mandatory for patients with BWS, because they do not usually experience chest pain, have attenuated symptoms, and are at high risk of fatal outcome, to look for pre-symptomatic cardiac dysfunction. The level of cardiac biomarkers such as troponin and brain natriuretic peptide as well as plasma catecholamines usually helps in the diagnosis of Takotsubo cardiomyopathy. In these cases, the first treatment is restoration of intrathecal drug delivery. Small doses of selective beta-blockers should also be considered as additional therapy. Further studies are needed to better understand the pathophysiology and establish a proper management of this adverse event.
Ethical approval
The patient gave informed consent for the publication of this case report.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





