1
Introduction
Syndrome of the trephined also called “sinking skin flap syndrome” is a rare and late complication of the craniectomy. It appears in the weeks or months (3 months in average) after the surgery and is characterized by a neurological deterioration, not explained by other etiologies. This syndrome also associates various symptoms such as headaches, motor impairments, cognitive disorders, alertness disorders and also in some cases autonomic dysfunction. This clinical picture can be aggravated by orthostatism and dehydration. A characteristic neurological improvement of the patient’s neurological state after having replaced the skull bone flap will validate the diagnosis .
2
Observation
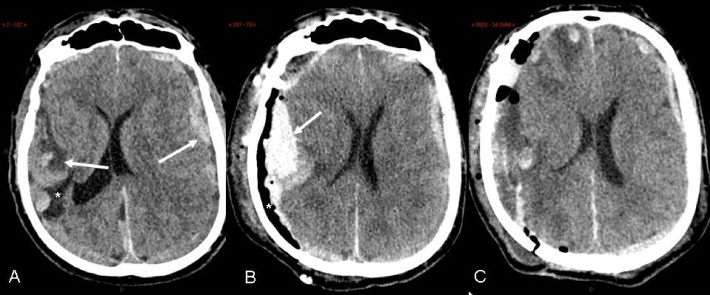
A 76-year-old male came to the emergency room presenting with intense holocranial headaches (pain VAS 9/10) for the past week, with no notion of recent trauma. A brain CT-scan performed as an emergency procedure ( Fig. 1 A) evidenced a bilateral subdural hematoma with a mass effect (subfalcine and left temporal cerebral herniation).
In the patient medical history, we noted an infarct in the right middle cerebral artery, 10 years earlier during surgical management for descending thoracic aorta replacement, which left him with an aphasia characterized mostly by speech disorders.
Two days later, a first drainage was performed by our neurosurgical team via a right fronto-parieto-temporal bone flap approach.
Postoperative care is characterized by a deterioration of the neurological state (sleepiness) in immediate postoperative care, evidenced by a CT-scan ( Fig. 1 B) which unveiled the recurrence of the subdural hematoma.
The next day a second drainage was performed, via the same surgical approach, with transfer to the intensive care unit, where the patient was monitored for 9 days.
After 45 days, the patient was transferred to our neurological rehabilitation center. Upon admission, the clinical evaluation showed major functional deficits with quadriparesis globally scored at 4/5 on the Medical Research Council (MRC) Scale, static gait disorders, and swallowing disorders requiring the placement of a gastrostomy tube (G-tube). Furthermore, the patient’s state of consciousness was preserved with a good understanding of simple orders.
Two and a half months after his admission to the emergency room, he presented with fever and frontal swelling on the right side. A CT-scan performed the same day showed a cerebral empyema right below the surgical site (right fronto-parieto-temporal bone flap). The bone flap was removed and replaced simultaneously during the drainage procedures for the bilateral subdural hematoma. An immediate neurosurgical management of the empyema was performed by removing the bone flap and cement, as well as draining and profusely rinsing the infected area.
A long term IV antibiotic therapy was implemented by the infectious disease team (6 weeks) following the positive result of the cerebrospinal fluid to a multisensitive Staphylococcus aureus .
Following this multidisciplinary care in our neurological rehabilitation center, the patient showed an improvement of his static disorders and quadriparesis (4/5 on the MRC). G-tube feeding was continued due to the severe swallowing disorders.
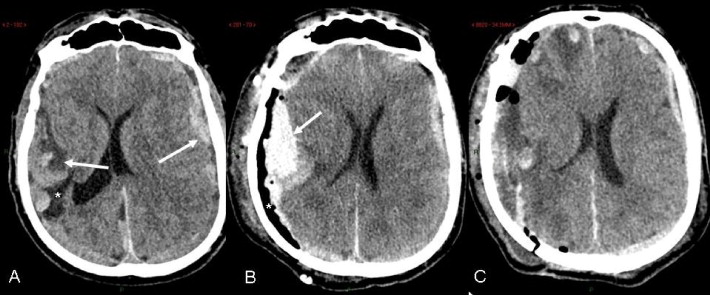
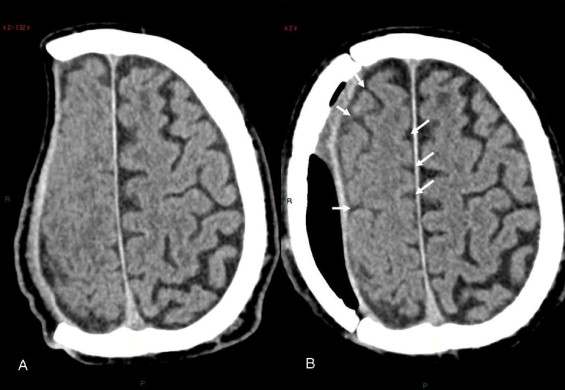
Two months after removing the skull bone flap, the patient presented with a sudden deterioration (< 24 hours) of his neurological state characterized by a state of sleepiness, aggravation of the left hemiparesis globally evaluated at 2/5 on the MRC (previously at 4/5) in a left-handed patient and major balance disorders. Blood tests and infectious results were reassuring. An emergency CT-scan showed a retraction of the cerebral parenchyma with loss of right hemispheric convexity. An NMRI ( Fig. 2 ) performed three days later did not evidence any acute phenomenon that could explain the patient’s symptoms. The NMRI showed the loss of right hemispheric convexity with retraction of the skin flap ( Fig. 2 A), compression of the right superior frontal sulcus and compression of the right hemisphere between the skin flap and the falx cerebri ( Fig. 2 B).
Based on the clinical and imaging data, the neurosurgical and infectious disease teams agreed to replace the bone flap.
Right from the next day after surgery, the patient showed a clear neurological improvement, improved left hemiparesis and balanced disorders; he recovered the neurological status he had prior to his clinical deterioration.
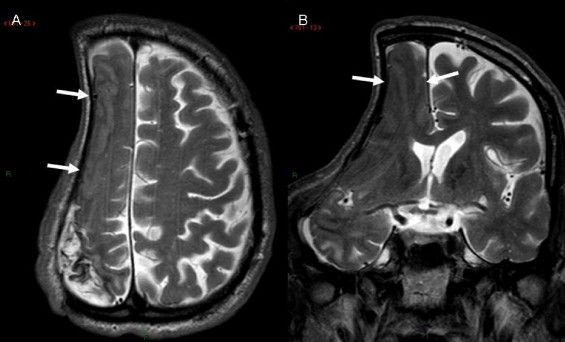
An NMRI evaluation ( Fig. 3 ), performed two months after the bone flap surgery, showed the reappearance of the right hemispheric convexity and sulci, thus underlining the disappearance of the mechanical constraint on the cerebral parenchyma.
2
Observation
A 76-year-old male came to the emergency room presenting with intense holocranial headaches (pain VAS 9/10) for the past week, with no notion of recent trauma. A brain CT-scan performed as an emergency procedure ( Fig. 1 A) evidenced a bilateral subdural hematoma with a mass effect (subfalcine and left temporal cerebral herniation).