Surgical Treatment of Three-part Proximal Humeral Fractures with Plate Fixation
Andrew S. Neviaser
Dean G. Lorich
Proximal humerus fractures (PHFs) account for 5% of all fractures and typically occur in patients older than 60 years (1). Eighty percent of these are nondisplaced and stable (2). They can be treated nonoperatively with acceptable outcomes. The nonoperative treatment of three- and four-part fractures yields distinctly worse results than less severe injuries, however (3). Although there is general agreement that surgical intervention is required for these injuries, many different techniques have been described and there is no consensus regarding which is best. The advent of locking plate technology has led to a renewed interest in open reduction and internal plate fixation. Complication rates associated with locking plates have been higher than expected, however, ranging from 9% to 36% and are highest in elderly patients (4, 5, 6, 7). Among the most frequent are varus collapse, intra-articular screw penetration, and avascular necrosis (AVN). When these complications are avoided, clinical outcomes after locking plate reconstruction can be quite satisfactory and are superior to outcomes after other procedures such as humeral head replacement (8, 9, 10). We have developed a comprehensive treatment protocol for displaced PHFs. It aims to minimize the complications frequently associated with locking plates, maximize the stability of fixation, and allow for early range of motion exercises.
INDICATIONS/CONTRAINDICATIONS
The most common pattern of three-part injury is a displaced fracture of the greater tuberosity and separation of the humeral shaft from the head at the surgical neck (three-part greater tuberosity fracture). Much less frequently, the lesser tuberosity is fractured rather than the greater (three-part lesser tuberosity fracture). It is important to note that many patients with fractures of one tuberosity and the surgical neck that are nondisplaced can be managed nonoperatively, but these are quite different from true three-part fractures. In devising his classification, Neer defined a “part” as being displaced 1 cm or angulated more than 45 degrees, and hence, there are no nondisplaced three-part fractures by this definition. The choice between operative and nonoperative treatment is made based on the characteristics of the fracture (i.e., displacement and angulation of the parts) and the patient.
Displacement is dictated by the pull of the muscular attachments about the proximal humerus, and a three-part fracture often results in greater displacement than other fracture patterns. When the humeral head is separated from the shaft and can rotate freely, disruption of the force couple between the anterior and posterior rotator cuff produced by fracture of one tuberosity leads to significant displacement of the avulsed
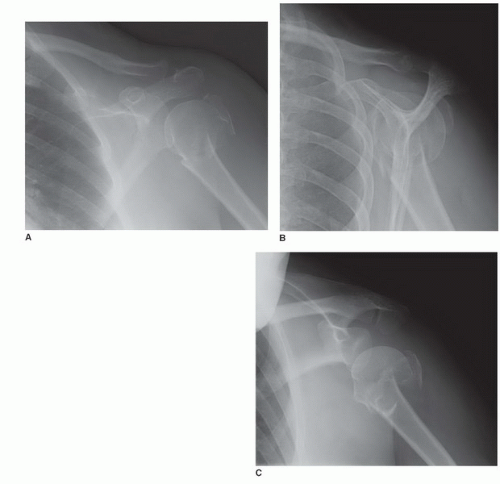
tuberosity as the head is rotated away from it by the pull of the cuff muscle(s) attached to the other, intact tuberosity (Fig. 30-1A-C). The humeral shaft is displaced anteromedially by the pull of the pectoralis major and proximally by the pull of the deltoid.
tuberosity as the head is rotated away from it by the pull of the cuff muscle(s) attached to the other, intact tuberosity (Fig. 30-1A-C). The humeral shaft is displaced anteromedially by the pull of the pectoralis major and proximally by the pull of the deltoid.
Nonoperative treatment of these fractures yields limited function and unpredictable pain relief. It should be limited to those patients who are unfit for anesthesia and those unwilling to participate in postoperative rehabilitation. Our experience has been that patients who are unwilling or unable to engage in postoperative therapy, due to either physical or mental illness, do not receive sufficient benefit from operative treatment to warrant its undertaking.
Numerous operative techniques have been described to treat these fractures. Although many authors suggest “bone quality” is a factor in determining treatment methods, poor bone quality is not a contraindication to joint-preserving procedures. With an aging population, PHFs will likely become more common and treatment methods must account for the diminished bone quality that comes with advancing age. In elderly patients with significant osteoporosis, the central portion of the proximal humeral metaphysis is relatively hollow with few trabeculae. The humeral head is frequently a shell of subchondral bone whose center is empty either due to osteoporosis or from the impaction of the humeral shaft. Successful open reduction and internal fixation of poor quality bone requires both medial and lateral column support which cannot be achieved with a lateral locking plate alone (11, 12). We routinely establish bicolumnar support with an endosteal cortical strut graft, most commonly an allograft fibula. This mechanical augmentation permits open reduction and internal fixation to be performed successfully even in severely osteoporotic bone.
AV N of the humeral head is also a concern in determining treatment, but the use of humeral head replacement for three-part fractures is generally not justified based on this risk. Recent advances in our understanding of head perfusion have provided greater insight into AV N and suggest that it can be minimized by appropriate surgical technique. Several authors have suggested that the anterolateral branch of the anterior humeral circumflex artery is the main nutrient artery of the proximal humerus (13). However, this vessel is disrupted in 80% of PHFs, whereas the posterior humeral circumflex artery is preserved in a similar percentage (14). Rates of AV N cannot be explained simply by compromise of the anterior vessels. Using gadolinium-enhanced MRI, we have recently shown that the posterior humeral circumflex artery provides perfusion to a majority of the humeral head (64%), whereas the anterior humeral circumflex artery supplies a smaller portion (36%) (15). Crosby et al. (16) have demonstrated that humeral head perfusion is maintained even in three- and four-part fractures. Yet, rates of postoperative AV N range from 3% to 37%, and preoperative prediction of this complication has been largely inaccurate (17, 18, 19). Intraoperative and postoperative factors likely account for this variability rather than the initial injury. Some authors have found that open treatment of fractures doubled the rate of AV N as compared to closed treatment. Perfusion can be disrupted during dissection, manipulation of fracture pieces, and osteosynthesis and by postoperative thrombosis (17). Careful surgical technique and appropriate fixation can minimize this complication. We have developed a minimally invasive anterolateral approach that provides direct access to the lateral hypovascular plating zone of the humerus and may reduce the risk of AV N (20). Humeral head replacement should therefore be limited to only those who have significant preexisting glenohumeral arthritis. There may be some patients in whom tuberosity healing via osteosynthesis is so fraught with uncertainty that a primary reverse shoulder arthroplasty may be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree