Talus fractures result from high-energy mechanisms and usually occur at the neck. Functional outcome after talar neck fracture worsens with increasing Hawkins grade. The mainstay of treatment for talar neck fractures is anatomic reduction and internal fixation. Prompt reduction of dislocations should be performed. Patients should be taken to the operating room as soon as stabilized. Dual incisions and a combination of minifragment plates and screws should be used. Talar body fractures have a high rate of ankle and subtalar arthritis. Lateral process fractures are frequently missed on radiographs. Complications after talus fractures include osteonecrosis, malunion, post-traumatic arthritis, and infection.
Key points
- •
Talus fractures result from high-energy mechanisms and may be associated with other injuries to the foot and ankle.
- •
Talar neck fractures are most common and are classified using Hawkins classification. Functional outcome scores have been shown to vary inversely with increasing Hawkins grade.
- •
Prompt reduction of dislocation and surgical treatment of open fractures help decrease complications.
- •
Open anatomic reduction and internal fixation using dual incisions should be performed as soon as the patient is stable for the operating room.
- •
Hawkins sign as seen on radiographs at 6 weeks indicates intact blood supply and is a good prognostic indicator.
- •
Long-term complications after talus fractures include osteonecrosis, malunion, and arthritis of ankle and subtalar joints.
Management of talus fractures is a challenge because of the historically poor outcomes and high incidence of complications. Talus fractures account for 2% of all lower extremity injuries and are typically associated with a high-energy mechanism.
Anatomy
Sixty percent of the talar surface is articular cartilage, and no muscles insert on or originate from the talus. The limited nonarticular surface of the talus available for vascular supply potentially contributes to the high risk of osteonecrosis following fractures of the talus.
Osteology
The superior surface of the talar body articulates with the tibial plafond, and the articular surface extends medially and laterally to articulate with the malleoli. The inferior aspect of the body articulates with the posterior facet of the calcaneus, and the talar head articulates with the navicular. The lateral process of the talus is also involved in the articulation with the posterior facet of the calcaneus. The posterior process of the talus is composed of the medial and lateral tubercles between which the flexor hallucis longus traverses. Ligamentous and capsular expansions attach to the talar neck, which is relatively devoid of articular cartilage and is an important location of vascular supply.
Blood Supply
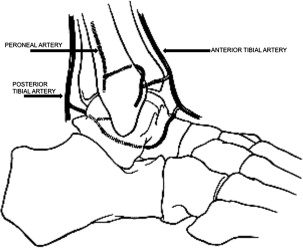
The posterior tibial artery supplies the anastomotic sling of vessels in the tarsal sinus and the tarsal canal that make up the primary arterial blood supply to the talus. These branches enter the talus via the inferior aspect of the neck and course posterolaterally to supply the talar body in a retrograde fashion. A branch of the anterior tibial artery enters the talus at the dorsal aspect of the neck and supplies the talar head, and a branch of the peroneal artery contributes to the artery of the sinus tarsi. The blood supply to the talus is summarized in Fig. 1 .
Anatomy
Sixty percent of the talar surface is articular cartilage, and no muscles insert on or originate from the talus. The limited nonarticular surface of the talus available for vascular supply potentially contributes to the high risk of osteonecrosis following fractures of the talus.
Osteology
The superior surface of the talar body articulates with the tibial plafond, and the articular surface extends medially and laterally to articulate with the malleoli. The inferior aspect of the body articulates with the posterior facet of the calcaneus, and the talar head articulates with the navicular. The lateral process of the talus is also involved in the articulation with the posterior facet of the calcaneus. The posterior process of the talus is composed of the medial and lateral tubercles between which the flexor hallucis longus traverses. Ligamentous and capsular expansions attach to the talar neck, which is relatively devoid of articular cartilage and is an important location of vascular supply.
Blood Supply
The posterior tibial artery supplies the anastomotic sling of vessels in the tarsal sinus and the tarsal canal that make up the primary arterial blood supply to the talus. These branches enter the talus via the inferior aspect of the neck and course posterolaterally to supply the talar body in a retrograde fashion. A branch of the anterior tibial artery enters the talus at the dorsal aspect of the neck and supplies the talar head, and a branch of the peroneal artery contributes to the artery of the sinus tarsi. The blood supply to the talus is summarized in Fig. 1 .
Talar neck fractures
Approximately 45% of talus fractures occur at the neck. The mechanism of injury has been described as hyperdorsiflexion of the ankle and fracture through the talar neck due to impingement of the anterior tibia. There is a rotational component implied by the presence of medial comminution and concurrent medial malleolar fracture in 11% to 28% of cases. The mechanism is typically high energy, as suggested by high rates of associated fractures in 54% to 64% of cases and open fractures in approximately 20% of cases.
Classification
The most commonly used classification system was described by Hawkins and modified by Canale and Kelly ( Fig. 2 ). This classification system has been shown to correlate with prognosis as shown in Table 1 . Use of a computed tomography (CT) scan improves the interobserver correlation of the modified Hawkins classification as compared with radiographs alone.
| Talar Neck Fracture | Associated Joint Subluxation or Dislocation | Rate of Osteonecrosis (%) | |
|---|---|---|---|
| 1 | Nondisplaced | None | 13 |
| 2 | Displaced | Subtalar | 50 |
| 3 | Displaced | Subtalar Tibiotalar | 80 |
| 4 | Displaced | Subtalar Tibiotalar Talonavicular | 50 |
Clinical Evaluation
Patients with talar neck fractures typically present after a high-energy mechanism with foot swelling. There may be gross deformity and skin tenting with associated dislocations. Dislocations of the talus should be reduced urgently to reduce the risk of osteonecrosis and skin compromise. Type 2 fracture dislocation is the most common, and the reduction maneuver is plantar flexion and inversion or eversion. Up to 38% of Hawkins type 3 fractures are open, and in these cases, the talus may be partially or completely extruded. Neurovascular status of the foot should be assessed. The patient should also be evaluated for other injuries given the high-energy mechanism.
Radiographic Evaluation
Radiographic evaluation of the injured extremity should include anteroposterior, oblique, and lateral views of the foot and the ankle. To better visualize the talar neck, an additional view can be obtained as described by Canale and Kelly and shown in Fig. 3 (Canale view). CT scans are useful to assess for comminution, intra-articular fragments, and congruent reduction of subtalar, tibiotalar, and talonavicular joints.
Treatment: Nonoperative
Type 1 fractures are usually amenable to nonoperative treatment if CT scan truly demonstrates no displacement of the talar neck. As little as 2 mm of displacement has been shown to alter contact pressures of the subtalar joint, which can lead to arthritis. The patient is placed in a short-leg cast for 6 weeks with no weight bearing permitted. Weekly radiographic confirmation with a Canale view that no displacement of the talar neck has developed is recommended. After 6 weeks of cast immobilization, the patient can be converted to a fracture boot for an additional 6 weeks with restricted weight bearing.
Treatment: Operative
Anteromedial
The anteromedial approach to the talus is performed using an incision medial to the anterior tibial tendon to visualize the talar neck. An osteotomy of the medial malleolus can be performed using this approach for better visualization of the talar body. Care should be taken to avoid stripping the dorsal aspect of the neck and deltoid ligament attachment to preserve what remains of the blood supply. This approach by itself may be insufficient if there is medial comminution or impaction, because judgment of the reduction may be inadequate without visualizing the lateral aspect of the neck.
Anterolateral
To approach the talar neck using the anterolateral approach, an incision is made lateral to the extensor digitorum longus. If this incision is used in conjunction with the anteromedial approach, an adequate skin bridge should be left to avoid skin necrosis. It is especially important to avoid injury to the vessels in the tarsal sinus when utilizing this approach. Provisional fixation with Kirschner wires is performed, and then medial and/or lateral screws and plates are placed from a point just off the articular surface of the head and directed posteriorly into the body. Cannulated screws are useful to better control the position of the screw.
Posterolateral
Screws can also be placed from posterior to anterior, allowing for a configuration that is perpendicular to the fracture line. The approach is lateral to the Achilles tendon between the flexor hallucis longus and peroneal tendons, revealing the posterior process of the talus. The ideal location of the screws is starting at the lateral tubercle and angled anteromedially. Risks of this approach include screw penetration of the subtalar joint, involvement of the talonavicular joint, and injury to the peroneal artery and saphenous nerve.
Percutaneous fixation
Displaced talar neck fractures should be fixed in anatomic position. Closed reduction is sometimes achieved with the foot in equinus, but this can lead to contracture. If closed reduction is possible, and there is no significant comminution, percutaneous screw fixation is an option. Low rates of osteonecrosis and malunion have been described when closed reduction is performed using Schanz screws, and percutaneous screw fixation is performed in Hawkins grades 2, 3, and 4. Percutaneous screw fixation can also be performed in nondisplaced talar neck fractures to begin early range of motion. Screws (usually 4.5 mm diameter) can be placed from a posterolateral or anterior approach. In general, when using screws to fix talar neck fractures, the surgeon should consider using titanium screws so that magnetic resonance imaging (MRI) can be used postoperatively to assess for bony healing and/or avascular necrosis.
Open reduction and internal fixation
Anterior-to-posterior screws versus posterior-to-anterior screws
If the decision is made to use screw fixation, Swanson and colleagues showed superior mechanical strength using the posterior-to-anterior technique. A trend toward increased strength of posterior-to-anterior compared with anterior-to-posterior screws was also found by Attiah and colleagues in a biomechanical study.
Screws alone versus plate and screws
Plate fixation is performed in a bridging fashion if there is significant comminution as shown in Fig. 4 . The plate may be placed medially or laterally depending on the location of comminution. Plate fixation has been shown to effect a more precise reduction and avoids malalignment due to compression through areas of comminution that can occur when using only compression screws. Combined plate and screw fixation is not as strong as using screws alone as measured by Charlson and colleagues in a biomechanical cadaver study, but this difference is not clinically significant. Another cadaveric study found no significant difference in strength when comparing various screw combinations to screw with medial plate fixation.







