Surgical Techniques for Failed Instability Surgery Including the Latarjet Procedure
Joshua S. Dines
David M. Dines
INDICATIONS AND CONTRAINDICATIONS
Complications after glenohumeral stabilization include recurrent instability, loss of range of motion (ROM), hardware failure, degenerative joint disease, infection, and neurovascular injury. The causes of recurrence are complex and often multifactorial including technical error, hardware and/or suture failure, misdiagnosis of type or direction of instability, new traumatic injury, and improper postoperative protection or rehabilitation. To appropriately treat recurrent instability, it is imperative to identify the causes that led to failure after the index procedure.
Occasionally, the cause of recurrent instability is preordained, predicated on inaccurate diagnosis before the index procedure. Failure to recognize multidirectional instability or to inaccurately diagnose the direction of instability can both lead to failed stabilization surgery. Additionally, failure to recognize and treat significant glenoid bone loss or engaging Hill-Sachs lesions at index surgery is a common cause of failure (1). Technical errors can include inappropriate anchor placement, failure to properly mobilize and shift the capsulolabral complex, and/or insecure knots.
In some cases, patients will fail to comply with postoperative instructions or will be exposed to improper postoperative rehabilitation leading to failure of stabilization. Occasionally, despite appropriate treatment and rehabilitation, a new traumatic injury can cause the recurrence.
PREOPERATIVE PLANNING
Patients who fail primary stabilization can present a very difficult diagnostic challenge. It is imperative to define the cause of the recurrence by taking a careful, thorough history including direction, mechanism, and quality of the instability pattern. In cases of a new traumatic injury, the degree of trauma that created the recurrence should be defined.
Details of the index operation including technique, hardware used, and postoperative care must be obtained by the treating surgeon. This includes evaluation of the index operative report, postoperative management, and preoperative imaging when available. In some cases, reevaluation of these records and studies will help define the cause of failure, such as in cases of an inaccurate diagnosis or of a failure to recognize significant glenoid bone loss. The technique
at index operation will impact on and may even define or limit the options for revision stabilization. For example, primary arthroscopic stabilizations rarely limit revision options as much as a prior Latarjet or Bristow procedure.
at index operation will impact on and may even define or limit the options for revision stabilization. For example, primary arthroscopic stabilizations rarely limit revision options as much as a prior Latarjet or Bristow procedure.
A comprehensive physical examination must be performed and may demonstrate apprehension in another direction or an unrecognized multidirectional component. Underlying muscular damage, such as subscapularis failure after an open procedure, or nerve injury may also be identified as a cause of failure.
Imaging of the glenohumeral joint and soft tissues is mandatory and critical for proper diagnosis. Plain x-ray views including axillary or West Point views can be helpful in assessing bone loss, but in most cases, MRI and/or CT scans with or without contrast will better define soft-tissue abnormalities. Younger patients, in whom the risk of rotator cuff tears complicating the dislocation is lower, may benefit more from a CT scan. CT scans can better delineate the degree of bone loss, an important factor in attempting to define the most appropriate treatment (Fig. 23-1).
In many cases, arthroscopic evaluation can be a valuable diagnostic tool to accurately visualize the intra-articular structures, both bony and soft tissue, following failed open and/or arthroscopic stabilization procedures. At arthroscopy, diagnosis of glenoid bone loss, as well as capsular and labral damage, can be identified. In some cases, the soft-tissue injury/insufficiency can be treated concurrently. Implant failure (either anchor or suture) may be readily identifiable as well. Furthermore, less common pathology such as an untreated HAGL (humeral avulsion glenohumeral ligament) lesion often can be identified and an appropriate surgical treatment plan initiated (Table 23-1).
SURGERY
Revision Shoulder Stabilization Technique
The surgical treatment for recurrent glenohumeral instability in all cases should begin with a careful examination under anesthesia to assess direction and degree of recurrent instability. A load-and-shift maneuver will indicate the direction. The degree may be quantified as follows:
1+ humeral head to the rim
2+ humeral head over the rim
3+ humeral head locked over the rim
Inferior instability is quantified by a sulcus sign defined by the distance of the “hollow” below the acromion when inferior traction is applied to the arm.
After examining the patient under anesthesia, we routinely perform a diagnostic arthroscopy. Arthroscopy can be performed in the beach-chair or lateral decubitus position, which should be determined based on surgeon preference. This allows for assessment of the degree of bone and soft-tissue injury/deficiency. A careful assessment of the articular cartilage, bone loss, and capsular integrity is necessary to plan the definitive open or arthroscopic
revision and also to be able to identify the presence of, or risk of developing, secondary osteoarthritis. The proper identification and treatment of HAGL lesions or ALPSA (anterior labral periosteal sleeve avulsions) lesions are critical for successful outcomes of revision stabilization. If not identified or misdiagnosed, these lesions may lead to failure of the revision surgery as well, with the consequence that the clinical instability continues unabated. If a significant Hill-Sachs lesion is present, the position of engagement should be ascertained.
revision and also to be able to identify the presence of, or risk of developing, secondary osteoarthritis. The proper identification and treatment of HAGL lesions or ALPSA (anterior labral periosteal sleeve avulsions) lesions are critical for successful outcomes of revision stabilization. If not identified or misdiagnosed, these lesions may lead to failure of the revision surgery as well, with the consequence that the clinical instability continues unabated. If a significant Hill-Sachs lesion is present, the position of engagement should be ascertained.
TABLE 23-1 Treatment Options | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
When the diagnostic arthroscopy is completed, the definitive revision stabilization is carried out. The ideal technique to use is based on the type of pathology that must be corrected, the surgeon’s comfort level with open versus arthroscopic techniques, and the patient’s activity demands.
The first decision to make is whether a soft-tissue or bony repair/reconstruction is necessary.
If a soft-tissue reconstruction is a viable option, then the choice of open or arthroscopic approach is often made based on surgeon comfort level with either procedure and the best means of completely treating all pathology. While our preference is to perform an arthroscopic soft-tissue reconstruction, the surgeon should use the soft-tissue techniques that will result in the best outcome for the patient. The decision is not merely based on surgical approach but also on what pathologic process predominates. While soft-tissue lesions can often be repaired or reconstructed effectively by arthroscopy, some pathologic lesions may defeat even the most skilled arthroscopist. For example, the remaining tissue post thermal capsular stabilization is often of such poor quality that grafting techniques may be required, and, if so, this is usually more predictably done open. Though arthroscopic repair of HAGL lesions has been described, this is technically demanding, and, for this reason, this lesion is often treated through open surgery. Bone graft/block procedures most frequently require open surgical techniques, although arthroscopic techniques have been described.
Soft-tissue Revision Reconstructions
After determination of specific pathology has been made by a combination of preoperative workup, imaging, examination under anesthesia, and diagnostic arthroscopy, the surgeon must systematically address all pathology encountered, including loose bodies, chondral lesions, loose hardware, and suture material. In revision open techniques, this may include “undoing” the prior procedure, attempting to create near-normal anatomy, and “starting over.” For example, after a Magnuson-Stack lateral transfer of the subscapularis, this may entail taking down this muscle-tendon unit from its transferred position, correcting capsular pathology, and rerepairing subscapularis. The surgery after a failed Bristow repair requires decision making about whether the prior bone graft must be taken down or can be left in place.
Arthroscopic Revision Anterior Stabilization
A number of technical considerations peculiar to arthroscopic revision surgery directly related to recurrent procedures require emphasis.
Arthroscopic stabilization procedures can be done in the lateral decubitus or beach-chair position. One advantage to arthroscopy in the beach-chair position is that it can be more easily converted to an open approach, if necessary.
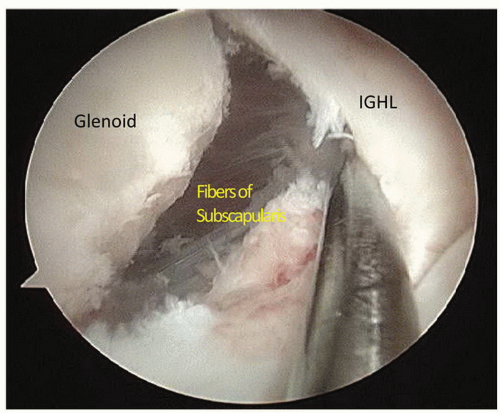
After a complete diagnostic arthroscopic evaluation, the surgeon must proceed with an appropriate capsulolabral reconstruction. Utilizing appropriate portal placement, the surgeon must carefully release the scarred and malpositioned capsulolabral complex completely from its attachment to the glenoid. The IGHL is mobilized using arthroscopic elevators. In order to do this properly, the capsule and remaining labrum must be released down to at least the 6 o’clock position. At this point, the subscapularis muscle should be visible to ensure appropriate release. While having the arthroscope in the posterior portal to visualize the entire joint and identify
extent of pathology, it is often useful to perform this labral and capsular mobilization from an anterior portal while visualizing from anterior-lateral (rotator interval) portal (Fig. 23-2).
extent of pathology, it is often useful to perform this labral and capsular mobilization from an anterior portal while visualizing from anterior-lateral (rotator interval) portal (Fig. 23-2).
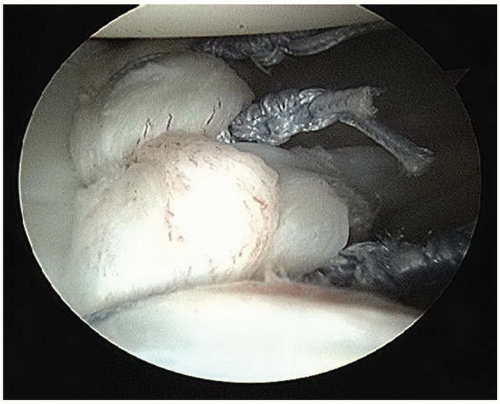
Next, the IGHL complex must be advanced superiorly to reestablish normal tension in the ligament. It should be properly fixed to a well-prepared surface of the glenoid rim. Well-fixed suture anchors and secure tying techniques are critical for success (Fig. 23-3). In cases of an incompetent rotator interval, frequently identified clinically by a positive sulcus sign, a reefing of the interval may be required.
Bone Deficiency
Unrecognized bony defects are a common cause of failed glenohumeral stabilization procedures. Bone defects occur both on the glenoid and humeral head (Hill-Sachs lesion) (Fig. 23-4). Significant glenoid bone loss is the most common cause of recurrence. However, studies have shown a higher recurrent instability rate if a Hill-Sachs defect is deeper than 15% of the radius of the humerus (i.e., ≥4 mm) (2). This is because these two lesions may engage more easily once a critical size is reached. The degree of bony involvement will determine the appropriate surgical procedure. For this reason, quantification of bone loss is mandatory for proper treatment. CT scans and measurements of bone loss during diagnostic arthroscopy are helpful in this assessment.
Minor Glenoid Bone Loss (Less Than 15%)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree