Surgical Off-loading External Fixation and Plastic Reconstruction of the Foot and Ankle
Crystal L. Ramanujam
Zacharia Facaros
Thomas Zgonis
Introduction
Surgical off-loading external fixation serves as a unique method for protection and stabilization of soft tissue and osseous reconstruction in the lower extremity. This technique provides a means for effective immobilization that is particularly useful in plastic reconstruction. The survivability of soft tissue reconstruction can easily be compromised by pressures induced postoperatively, most commonly associated with weight bearing and premature joint motion. In addition to being well tolerated by the carefully selected patient, off-loading external fixation avoids complications often caused by traditional casting and splinting methods while also permitting easy accessibility for wound and/or flap care. Surgical off-loading external fixation can be adapted for scenarios requiring simultaneous flap management and deformity correction. Plastic reconstruction for the foot and ankle includes a wide array of options extending from skin grafts, orthobiologics and negative pressure wound therapy (NPWT) to local flaps, pedicle flaps, and free tissue transfer. Utilization of extensive plastic reconstruction with off-loading external fixation should be accomplished through a multidisciplinary approach tailored for the individual patient. The authors present a stepwise approach to applying surgical off-loading external fixation for various plastic reconstructive procedures in the foot and ankle.
Indications/Contraindications
Surgical off-loading external fixation is indicated for protection of plastic reconstruction that is not amenable to conventional casting or splinting. Furthermore, advanced soft tissue and osseous procedures at weight bearing or decubitus surfaces are better off-loaded with external fixation techniques since the limb is fully suspended in a rigid construct. For scenarios in which there is anticipated noncompliance with a non–weight bearing status, off-loading external fixation provides an ideal environment for immobilization and postoperative care. History of extensive bone resection for osteomyelitis or skeletal realignment for deformity correction does not preclude the use of external fixation, rather these situations benefit from stable bone and joint alignment established by the device. In addition, this method can be incorporated to stabilize fractures involving the foot and/or ankle while simultaneously providing off-loading of any plastic flap coverage required in cases of traumatic soft tissue loss. Most common external fixation constructs for fracture stabilization can be easily modified for off-loading components to prevent further soft tissue compromise caused by excessive contact pressures during the postoperative period.
The indications for specific types of plastic reconstruction vary on the basis of the clinical scenario and in many cases a combination of techniques can be successfully used. It is useful to base the surgical approach on the rationale behind the reconstructive soft tissue ladder or pyramid, with the least invasive options considered first prior to the complicated, more invasive methods. Once infection and/or bone pathology have been addressed, wounds can initially be considered for primary closure. However, wounds left behind following extensive soft tissue and bone resection will most likely require more advanced closure techniques. For larger, deep wounds with exposed tendon or bone, NPWT to facilitate proper granulation and prepare the wound for later definitive coverage may be used.
Extensive proximal amputation at the central rays of the foot for treatment of osteomyelitis and/or necrosis often leads to creation of a cleft-foot deformity. Although these amputations are technically easy to perform, the resultant foot may lead to recurrent wounds, transfer lesions, and instability. Several options have been described regarding closure of the defects through narrowing of the forefoot via manual compressive techniques. The use of an off-loading external fixation after central ray resection creates stable compression of the remaining metatarsals in order to close the defect without tension. This technique can also be combined with NPWT, skin grafting, or the use of orthobiologic matrices. The use of orthobiologic materials such as bioengineered skin substitute tissues may be employed if the soft tissue defect is located in an area that is unsuitable for a skin flap, and often over exposed neurovascular structures and tendons to prevent desiccation.
Split-thickness skin grafting (STSG) provides a quick and effective method for closure of well granulated wounds in non–weight bearing or sometimes if necessary in weight bearing areas of the foot. These are especially useful for coverage of wounds left behind following rotation and insetting of pedicle flaps. Local random flaps, which vary among advancement, rotational or transpositional types, are ideal for closure of small to moderately sized wounds with adequate perfusion. If a wound has surrounding soft tissue that demonstrates good elasticity by way of the pinch test, a local random flap is often an appropriate closure option. These flaps are suitable for coverage of plantar cuboid ulcerations associated with Charcot neuroarthropathy as well as sub-metatarsal head ulcerations.
Muscle flaps, which are based on their pattern of blood supply, can provide bulk for larger defects and excellent coverage at exposed bone, thereby facilitating local antibiotic delivery. The abductor hallucis (ABH) muscle flap is ideal for coverage of defects on the plantar and medial aspects of the foot and ankle, possibly extended to the medial malleolus region if necessary. The flexor digitorum brevis (FDB) muscle flap is favored for plantar central wounds, often allowing for the donor site to be closed primarily as result of its location. The abductor digiti minimi (ABDM) muscle flap is utilized for tissue loss about the lateral aspect of the mid- and rearfoot, often employed to close proximal and plantar lateral defects, and the extensor digitorum brevis (EDB) muscle flap is favored for large dorsal and proximal foot and ankle wounds.
Pedicle flaps are indicated when the aforementioned options are not viable. These flaps provide coverage of moderate to large size defects and are harvested from non–weight bearing surfaces. Neurovascular pedicle flaps such as the medial plantar artery (MPA) flap or reverse flow sural artery neurofasciocutaneous (SAN) flap are ideal for restoring sensation on weight bearing surfaces of the foot. The MPA flap is useful for defects located to the dorsal-medial or plantar-lateral regions of the midfoot and heel, providing structurally similar tissue to the plantar foot, posterior heel, and ankle defects with its thick glabrous plantar skin and shock-absorbing fibroadipose, subcutaneous tissue. The reverse flow SAN flap is preferred when attempting to cover extensive tissue loss around the heel, ankle, and lower leg. Pedicle flaps in combination with off-loading external fixation are extremely useful since these flaps are compromised in areas of movement or variable tension. Pedicle flaps may also be helpful harvested from the opposite extremity and thus creating the cross-leg or cross-foot pedicle flap.
Free tissue transfer is one of the final options for soft tissue coverage in the foot and ankle, ideal for providing stable wound coverage in larger defects and allows for optimal functional outcomes with less donor site morbidity when compared to pedicle flaps. However, in patients with multiple comorbidities free tissue transfer may not be indicated since the procedures often require longer operating times, prolonged hospital stays, intensive care unit monitoring, and the possible need for additional surgery to recontour the reconstructed area.
Contraindications for the use of surgical off-loading external fixation include preexisting internal fixation that prohibits proper wire insertion and poor bone quality or pathology that precludes pin fixation. Off-loading external fixation and plastic reconstruction may be delayed in certain patients with peripheral vascular disease until optimal circulation for healing can be established. These techniques are not ideal for patients who are unable to maintain a non–weight bearing status during the postoperative period or those who cannot undergo frequent monitoring for wound and pin site care.
Preoperative Considerations
Appropriate patient selection and surgical timing are vital to the success of plastic reconstruction of the foot and ankle with surgical off-loading external fixation. A multidisciplinary team approach is most successful for the comprehensive management of these patients. An extensive workup, keeping in mind the presence of infection, vascular status, patient age, associated comorbidities, level of deformity, as well as knowledge of compliance are crucial to surgical planning. The surgeon also needs to consider the patient’s psychosocial status and home support system since these can impact surgical expectations, especially regarding the postoperative course.
Once the patient is medically optimized, infectious processes must be addressed through adequate surgical debridement and appropriate antibiotic therapy. Staging of procedures is typically most ideal for the long-term success of plastic surgical techniques in the lower extremity. The presence of peripheral vascular disease must be assessed for improvement in healing potential prior to reconstruction. Basic noninvasive vascular testing is completed on a routine basis to ensure adequate perfusion to the affected area. Patency and direction of flow at the proposed artery to be included in the pedicle is tested using a Doppler ultrasound. A formal consultation with the vascular surgery team is obtained if more extensive workup is warranted. Diagnostic angiography can be performed to more closely evaluate arterial patency, while vein mapping is specifically done for the reverse flow SAN flap in order to determine the location and diameter of the lesser saphenous vein to delineate skin incision placement and guide surgical dissection.
Skeletal bone and joint stabilization is often recommended when combining plastic reconstruction and off-loading external fixation of the foot and ankle. This technique significantly aids in maintaining the foot and lower leg in a well-aligned position, allowing the soft tissue reconstruction to heal in the proper orientation in preparation for functional restoration. This phenomenon is important particularly to the plantar aspect of the foot, where the replaced soft tissue structures must be able to withstand and endure the absorption and shear forces applied during gait. Ordinarily following insetting of the flap, any premature movement or disruption before healing will compromise the area, commonly leading to surgical wound dehiscence. The off-loading external fixation device alleviates most of this potential adverse effect and when combined with skeletal bone and joint stabilization it provides adequate immobilization which is mostly useful for noncompliant or heavier patients who at times will disrupt the external fixation construct inadvertently. Skeletal bone and joint stabilization is frequently performed with single or multiple Steinmann pins, sizes of which vary depending on the location and anatomy targeted, common sizes ranging from 2.7 to 3.5 mm. The more common articulations stabilized tend to be the medial and
lateral columns of the foot, rearfoot, talocalcaneal and tibiotalar joints. The necessary external pin is usually inserted in a percutaneous fashion, from the plantar proximal aspect of the foot, oriented in a vertical fashion and oriented proximally and superiorly through the aforementioned joints while maintaining neutral alignment. C-arm fluoroscopy is commonly utilized to confirm accurate placement and alignment. Multiple external percutaneous pins are generally used and appropriately cut at the entry point, and exposed portions are protected by pin caps. This percutaneous skeletal bone and joint stabilization technique is usually recommended before the application of the surgical off-loading external fixation device.
lateral columns of the foot, rearfoot, talocalcaneal and tibiotalar joints. The necessary external pin is usually inserted in a percutaneous fashion, from the plantar proximal aspect of the foot, oriented in a vertical fashion and oriented proximally and superiorly through the aforementioned joints while maintaining neutral alignment. C-arm fluoroscopy is commonly utilized to confirm accurate placement and alignment. Multiple external percutaneous pins are generally used and appropriately cut at the entry point, and exposed portions are protected by pin caps. This percutaneous skeletal bone and joint stabilization technique is usually recommended before the application of the surgical off-loading external fixation device.
Characteristics of the particular external fixation system are important factors when considering biomechanical obligations for the specific pathology. For instance, the desirable mechanics for fracture repair can be oriented to allow for control of interfragmentary movement, whereas for deformity correction, the individual components and external fixation configurations provide stability and neutralization of forces to maintain correction. Prior to reconstructive surgery, significant soft tissue loss or vascular injury, when present, requires a stable external fixation construct that will allow for further debridement procedures or vascular repair if needed. Furthermore, in those instances that require plastic reconstruction, surgical off-loading external fixators become applicable to allow for proper healing time without disruption of the underlying correction.
Detailed Surgical Technique
The primary objective is to achieve closure of a wound after establishing a healthy, noninfected wound bed, well perfused and biomechanically stable with functional anatomy. In order to do so, concomitant osseous reconstructive procedures may be required to correct any underlying deformity that can support the overlying soft tissue reconstruction. Whether the soft tissue correction is located at the plantar aspect of the foot or more proximally on a non-plantigrade aspect, off-loading external fixation is a useful adjunct to stabilize the overall reconstruction. Although osseous deformity correction and realignment procedures are important for maintenance of soft tissue coverage and long-term durability, this chapter will mostly focus on specific creative soft tissue procedures with concomitant off-loading external fixation.
Negative Pressure Wound Therapy
Prior to the application of the NPWT device, wound bed preparation is typically achieved through sharp debridement. In many cases, the Versajet Hydrosurgery System (Smith & Nephew, Cambridge, UK) is used to precisely debride the wound base and avoid excessive tissue loss. Local hemostasis can be achieved through application of topical thrombin. The most frequently used NPWT device is the VAC system (Kinetic Concepts, Inc., San Antonio, TX); however, several other devices are also currently available on the market. The VAC system consists of an open-celled foam, adhesive tape, vacuum tube, and therapy unit with collecting canister. Two types of foam are available, including the traditional GranuFoam™ (with or without silver) and the Versa White Foam™. The first foam is used on typical full-thickness granular wounds, whereas the second foam is optimal for wounds with undermining or exposed avascular structures. After the wound is prepared through debridement, the appropriate foam is cut to fit the wound and placed directly against the wound base. The foam is then secured in place with the provided adhesive tape followed by application of the vacuum tube in direct contact with the foam, usually via a small slit cut into the adhesive tape overlying the foam. Adequate seal can be tested by first connecting the vacuum tube to the suction device. Once no leaks are found, the vacuum tube is then connected directly to the VAC therapy unit preset to 125 mmHg continuous therapy. If the VAC therapy is used over a STSG or any orthobiologic materials, it is usually left intact for continuous 3 to 5 days at a lower pressure. Bridging techniques are available for multiple wounds requiring NPWT or in cases where the vacuum tube cannot be placed directly over the wound itself.
Prior to the application of the off-loading external fixation, the use of a tourniquet if applied is deflated and a new sterile field is set up and the operative team changes their outer gloves to prevent contamination during application of the external fixation device. One or two tibia circular ring(s) is placed 10 to 15 cm proximal to the ankle joint making sure that the circular ring is well aligned within the lower extremity with adequate space permitting any postoperative edema. The first transosseous wire is inserted from a lateral-to-medial direction on the undersurface of the ring and is perpendicular at 90 degrees to the longitudinal axis of the leg in the frontal plane, while the second transosseous wire is inserted from a medial-to-lateral direction on the top surface of the ring at a 45- to 60-degree angle to the longitudinal axis of the leg. These transosseous wires are manually tightened to the periphery of the circular ring via wire fixation nuts and bolts from the side they were inserted, followed by tensioning and tightening from the opposite sides of the ring. Tensioning for the tibia transosseous wires ranges between 110 and 130 kg of force. At that point, cutting of the tibia wires after appropriate bending is performed. Next, a second circular ring is placed located over the midfoot/forefoot region and secured by the insertion of two smooth or olive transosseous wires each at approximately 45- to 60-degree angle in opposing fashion. These midfoot/forefoot transosseous wires are manually tightened and secured to the circular ring followed by appropriate tightening with the wrenches. Next, multiple threaded hinges are incorporated between the two rings or between the midfoot/forefoot ring and the tibial block which may be consisted of two circular rings and securely fastened into place. Distally threaded rods are then inserted on the medial and lateral aspects of the device and are secured posteriorly with carbon fiber bars to off-load the extremity in the appropriate fashion. A final bar-to-clamp apparatus is secured at the bottom of the off-loading surgical fixation for further stability and rigidity of the entire construct (Figure 20.1).
Finally, after the application of the external fixation device bridging techniques may be useful to connect the VAC system so that transosseous wires can be appropriately inserted at anatomic safe zones without sacrificing stability of the VAC dressing. NPWT is extremely versatile and can be used adjunctively over several types of plastic soft tissue reconstruction to facilitate wound healing in conjunction with off-loading external fixation (Clinical Case I).
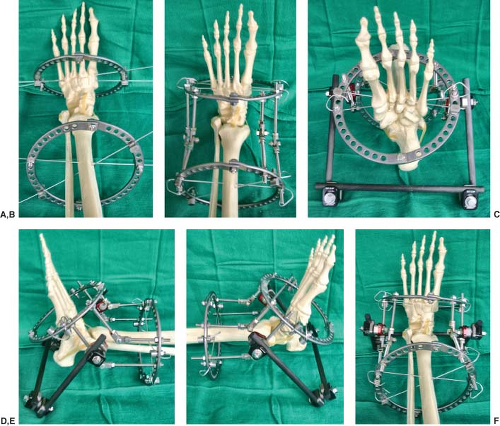 Figure 20.1. One or two tibia circular ring(s) is placed 10 to 15 cm proximal to the ankle joint making sure that the circular ring is well aligned within the lower extremity with adequate space permitting any postoperative edema. The first transosseous wire is inserted from a lateral-to-medial direction on the undersurface of the ring and is perpendicular at 90 degrees to the longitudinal axis of the leg in the frontal plane, while the second transosseous wire is inserted from a medial-to-lateral direction on the top surface of the ring at a 45- to 60-degree angle to the longitudinal axis of the leg (A). These transosseous wires are manually tightened to the periphery of the circular ring via wire fixation nuts and bolts from the side they were inserted, followed by tensioning and tightening from the opposite sides of the ring. Tensioning for the tibia transosseous wires ranges between 110 and 130 kg of force. Next, a second circular ring is placed located over the midfoot/forefoot region and secured by the insertion of two smooth or olive transosseous wires each at approximately 45- to 60-degree angle in opposing fashion. These midfoot/forefoot transosseous wires are manually tightened and secured to the circular ring followed by appropriate tightening with the wrenches (A). Next, multiple threaded hinges are incorporated between the two rings or between the midfoot/forefoot ring and the tibial block which may be consisted of two circular rings and securely fastened into place (B). Distally carbon fiber bars are then inserted on the medial and lateral aspects of the device (C) and are secured posteriorly with carbon fiber bars to off-load the extremity in the appropriate fashion (D, E). A final bar-to-clamp apparatus is secured at the bottom of the off-loading surgical fixation for further stability and rigidity of the entire construct (F).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





