Suprascapular and Axillary Nerve Injuries
Eric J. Strauss
Michael J. Alaia
Young W. Kwon
SUPRASCAPULAR NERVE INJURIES
Anatomy
The suprascapular nerve is a mixed motor and sensory nerve arising from the superior trunk of the brachial plexus. Although cadaveric dissections have found contributions from the fourth cervical nerve in up to 22% of specimens, the suprascapular nerve receives its fibers predominantly from the fifth and sixth cervical nerves.1,71
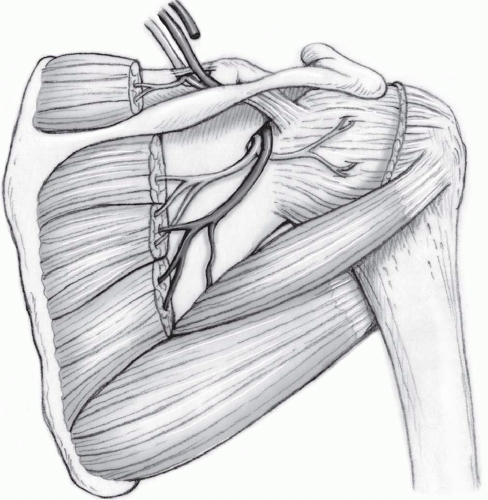
After leaving the superior trunk of the brachial plexus, the suprascapular nerve courses across the posterior cervical triangle parallel to the omohyoid muscle, deep to the trapezius muscle, and adjacent to the posterior surface of the clavicle. Proximally, the nerve is located lateral to the brachial plexus. As it heads toward the superior edge of the scapula and the suprascapular notch, however, the nerve migrates posterior to the plexus. At this location, the nerve runs through the suprascapular notch, most often staying deep to the superior transverse scapular ligament. The suprascapular artery and vein, which travel with the nerve, typically course superior to the ligament. Although rare, there are reports of the suprascapular artery traveling with the nerve inferior to the ligament.34,104 As it passes through the suprascapular notch, the nerve lies approximately 3.0 cm medial to the supraglenoid tubercle.9 The nerve then proceeds to run inferiorly along the posterior neck of the scapula, sending motor branches to the supraspinatus muscle, before turning medially around the spinoglenoid notch and under the spinoglenoid (inferior transverse scapular) ligament. Finally, it travels along the scapular body and terminates in several branches innervating the infraspinatus muscle (Fig. 33-1).27,98,109 There has been some controversy regarding the presence of a true spinoglenoid ligament. In their cadaveric study, Cummins et al. demonstrated that a true ligament existed in only 20% of their specimens and that 60% of the specimens contained just a thin fibrous band at that site.26 A more recent study of 58 cadavers, however, revealed a 100% prevalence of a true spinoglenoid ligament, composed of deep and superficial attachments to the glenoid, with superficial fibers also blending in with fibers of the posterior glenohumeral capsule.97 These authors attributed the differences in their results to different methods of specimen preparation.
The suprascapular nerve has been shown to provide sensory branches to the acromioclavicular (AC) joint, the glenohumeral joint, coracoacromial ligament, subacromial bursa, and the overlying skin.9,34,128,129 Vorster et al. also demonstrated a sensory branch that provided input to the posterior glenohumeral capsule in 87.1% of their specimens as well as a second acromial branch in 74.2%.128 Ebraheim et al. found a sensory
branch to the AC joint and subacromial bursa in all of their 12 specimens.34 This recent insight into the anatomic variation of the nerve may help explain the variable pattern of pain in patients with suprascapular nerve injury.
branch to the AC joint and subacromial bursa in all of their 12 specimens.34 This recent insight into the anatomic variation of the nerve may help explain the variable pattern of pain in patients with suprascapular nerve injury.
Classification and Etiology
Injuries to the suprascapular nerve are primarily classified according to their location and etiology. Additionally, they may be characterized by the degree of intraneural damage. The nerve can be injured at any point along its path including (1) the supraclavicular or infraclavicular region prior to entering the suprascapular notch, (2) the suprascapular notch, (3) the posterior scapular neck, and (4) the spinoglenoid notch. Suprascapular nerve injuries can be caused by traction, extrinsic compression, and direct trauma. The injuries may be iatrogenic or associated with a generalized brachial plexus disorder.109
One of the most common causes of extrinsic compression of the suprascapular nerve is a ganglion cyst. These cysts originate from the glenohumeral joint and are often associated with tears of the superior or posterior labrum. The size of the cysts may vary which, in turn, impact the clinical presentation. In rare instances, other masses such as synovial sarcomas, Ewing’s sarcoma, chondrosarcoma, renal cell carcinoma, and schwannoma have all been reported to cause suprascapular nerve compression along the course of the nerve.40,115
In some instances, the suprascapular nerve can be compressed without a pathological structure. As discussed previously, compression of the nerve may occur at the suprascapular and the spinoglenoid notches by anatomic structures. In addition, extreme shoulder abduction and external rotation occurring with overhead sports — volleyball,37,38,55,70,112 pitching,106 tennis29— can cause compression of the nerve at the suprascapular or spinoglenoid notches. In fact, elite-level volleyball players have been shown to have an incidence of suprascapular neuropathy or infraspinatus atrophy ranging from 12.5% to 33%.37,55,70
Traction injuries are believed to occur most commonly at the suprascapular and the spinoglenoid notches as the nerve has little excursion at these sites.27,115 Furthermore, variations in the osseous and ligamentous anatomy may limit the available space for the nerve. A cadaveric study demonstrated that cross-body adduction and internal rotation of the shoulder tightened the spinoglenoid ligament and posterior capsule which, in turn, stretched the underlying suprascapular nerve.32 First described by Kopell and Thompson in 1959, these types of traction injuries may occur following repetitive overhead activities.64 Anatomic variations in the suprascapular notch have been investigated extensively by Rengachary et al. who created a classification of these variations based on bony and ligamentous morphology (Fig. 33-2).105 The implication of this classification is that the likelihood of a traction injury is related to the available space for the nerve and the sharpness of the bony edges. These anatomic characteristics may be more accentuated when the shoulder is hyper-abducted, as this would increase the contact between the nerve and the edge of the notch.105 Rengachary et al. described this mechanism as “the sling effect.” Subsequently, clinical case reports of suprascapular nerve injuries have supported these proposed mechanisms of injury.16,105,113
Trauma has also been implicated as a cause of suprascapular nerve injury. Penetrating injuries, for example, can directly lacerate the nerve.132 More commonly, however, suprascapular nerve injuries have been associated with blunt and more generalized trauma to the shoulder girdle such as glenohumeral fractures and dislocations. Nearby fractures of the scapula, particularly those involving the scapula neck or the suprascapular notch, have caused suprascapular nerve injuries including traction and transection.11,117
Other more rare causes of suprascapular nerve injury include vascular insult and infection. The proposed mechanism for a vascular etiology involves intimal injury to the suprascapular artery following repetitive overhead activities. The vascular injury, in turn, is believed to produce microemboli that eventually compromise the blood supply to the vasa nervorum and cause an ischemic injury to the nerve.106 However, this hypothesis has not been substantiated clinically.27 Isolated injury to the suprascapular nerve from infection has not been documented. However, acute brachial neuritis (Parsonage-Turner syndrome) has been documented to include suprascapular neuropathy in approximately 97% of the cases.41
Rare instances of iatrogenic suprascapular nerve injury have also been reported in the literature. Mallon et al. reported on two cases of suprascapular nerve injury following distal clavicle resection. In both cases, excessive medial resection of the clavicle was believed to have caused the injury. Hence, the authors recommended that the distal clavicle not be resected beyond 1 cm.77 Yoo et al. also described iatrogenic injury following superior labrum anterior posterior (SLAP) repair, in which improper anchor insertion through the anterosuperior portal caused a suprascapular neuropathy below the
spinoglenoid notch.137 In an anatomic study, Chan et al. reported 6 medial glenoid vault perforations in 42 cadaveric specimens when drilling the low posterosuperior drill hole through the portal of Wilmington for a SLAP repair. Four of these six perforations caused direct injury to the suprascapular nerve.18 The nerve may also be vulnerable during posterior approaches to the scapula and the glenohumeral joint.133 Cadaveric studies have established a “safe zone” for avoiding the nerve. The average distance from the supraglenoid tubercle to the nerve is between 23 and 30 mm. At the base of the spine, as the nerve courses around the spinoglenoid notch, this distance shortens to 14 to 18 mm. Therefore, surgical exposure should remain lateral to this area in order to avoid an injury to the suprascapular nerve.9,116
spinoglenoid notch.137 In an anatomic study, Chan et al. reported 6 medial glenoid vault perforations in 42 cadaveric specimens when drilling the low posterosuperior drill hole through the portal of Wilmington for a SLAP repair. Four of these six perforations caused direct injury to the suprascapular nerve.18 The nerve may also be vulnerable during posterior approaches to the scapula and the glenohumeral joint.133 Cadaveric studies have established a “safe zone” for avoiding the nerve. The average distance from the supraglenoid tubercle to the nerve is between 23 and 30 mm. At the base of the spine, as the nerve courses around the spinoglenoid notch, this distance shortens to 14 to 18 mm. Therefore, surgical exposure should remain lateral to this area in order to avoid an injury to the suprascapular nerve.9,116
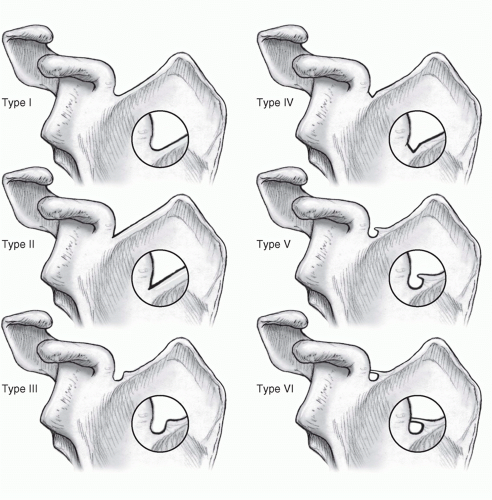 FIGURE 33-2. Classification of suprascapular notch morphology as described by Rengachary et al.105 With varying bony and soft tissue anatomy, the potential for nerve injury may be increased at this site. |
More recently, rotator cuff injury and associated surgical treatment have also been implicated in the pathogenesis of suprascapular nerve palsies.2,25,30,44,47,54,78,107,124,139 Albritton et al., for example, found that 5 cm medial retraction of the supraspinatus tendon insertion alters the course of the suprascapular nerve motor branch to the supraspinatus from 142.6 to 34.6 degrees. This drastic change in the nerve position may cause intrinsic damage to the nerve. In fact, these authors noted that the motor branch was under tension even after 2 to 3 cm of supraspinatus tendon retraction in all of their specimens.2 An electromyographic (EMG) analysis on 25 patients with full thickness rotator cuff tears found two cases with suprascapular neuropathy.124 Similarly, EMG analysis of eight patients with massive rotator cuff tears with greater than 5 cm of retraction demonstrated evidence of suprascapular neuropathy in all patients.78 Of these patients, two followed up with a repeat EMG following surgical repair, and both demonstrated significant renervation potentials (signs of nerve recovery).
In addition to these data, other authors have suggested that excessive lateral advancement of the rotator cuff tendons during surgical repair can also alter the orientation of the nerve’s terminal branches by up to 180 degrees and cause injury. Therefore, these authors recommended limiting lateral advancement of the rotator cuff tendons to 3 cm as further lateralization of the tendon (e.g., repair of massive rotator cuff tendons) may lead to suprascapular nerve injuries.44 Although the anatomic data are compelling, clinical reports following massive rotator cuff repairs with significant lateral advancement have not substantiated these concerns.25,47,54,107,139 Hoellrich et al., for example, demonstrated that the tendon can be advanced up to 3.5 cm without postoperative EMG changes consistent with neuropathy.54 In fact, patients with massive rotator cuff tear and suprascapular neuropathy demonstrated full or partial recovery of the nerve after repair of the rotator cuff.25,139
Clinical Symptoms
Despite the numerous etiologies of suprascapular nerve injury, most patients present with similar symptoms. Often, the patients complain of poorly localized, but constant “achy” pain about the posterior and lateral aspects of the shoulder.
Although the onset of pain may be associated with a specific trauma or change in activity level, most patients report an insidious onset. Activities that involve repetitive overhead motion may exacerbate these symptoms. Pain and weakness tend to be more severe in patients with a proximal nerve lesion. In contrast, patients with a distal lesion often complain of weakness only and may report minimal or no pain. This finding is consistent with the anatomic distribution of the sensory nerve fibers. In rare instances, the patients may be completely asymptomatic. As such, the nerve lesions may represent an incidental finding of unknown significance.27,37,98,109
Although the onset of pain may be associated with a specific trauma or change in activity level, most patients report an insidious onset. Activities that involve repetitive overhead motion may exacerbate these symptoms. Pain and weakness tend to be more severe in patients with a proximal nerve lesion. In contrast, patients with a distal lesion often complain of weakness only and may report minimal or no pain. This finding is consistent with the anatomic distribution of the sensory nerve fibers. In rare instances, the patients may be completely asymptomatic. As such, the nerve lesions may represent an incidental finding of unknown significance.27,37,98,109
Clinical Evaluation
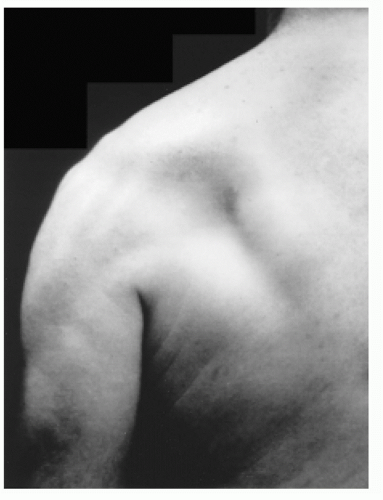
In addition to a deliberate shoulder examination, a thorough upper extremity and cervical spine examination must be performed in all patients. During early stages following a suprascapular nerve injury, the examination may only yield nonspecific findings. Chronic nerve injuries, however, may reveal asymmetry of the shoulder girdle musculature, noting atrophy of the supraspinatus and/or the infraspinatus muscles. Due to the overlying trapezius muscle, atrophy of the supraspinatus muscle may be difficult to appreciate in some patients. Atrophy of the infraspinatus muscle, however, is often readily apparent (Fig. 33-3). Palpation along the course of the nerve can reveal focal tenderness at the site of compression. Examination may also reveal mild to moderate loss of strength in shoulder abduction and external rotation. Abduction weakness will occur only with lesions involving the supraspinatus muscle as it acts in concert with the deltoid to elevate and abduct to the humerus.57 Involvement of the infraspinatus muscle does not always result in external rotation weakness as some patients can compensate with the teres minor and posterior deltoid muscles.37,49
Unlike other peripheral neuropathies, there are no specific provocative maneuvers to accentuate the symptoms of a suprascapular nerve lesion. Cross-arm adduction of the shoulder may place the nerve under increased tension as it passes under the spinoglenoid ligament. Hence, if a patient notes increased pain or discomfort with this maneuver, a suprascapular nerve injury may be suspected.16 It is important to differentiate the exact location of pain, however, as AC joint pathology may also cause similar pain with this provocative maneuver.36 For some patients whose presentation is suspicious for a suprascapular nerve lesion, a diagnostic injection can be considered. Injection of the suprascapular notch, for example, may provide alleviation of pain. Unfortunately, by itself, this test is not specific for the nerve lesion as patients with other types of shoulder pathology may also find pain relief from a suprascapular nerve block.98,102,109
Electrodiagnostic Studies
Clinical suspicion for a suprascapular nerve injury should be confirmed with electrodiagnostic studies. Indications for EMG include isolated weakness of the rotator cuff musculature or unexplained fatty atrophy of the rotator cuff muscle on magnetic resonance imaging (MRI). The mean normal latencies between Erb’s point (formed by the union of the C5 and C6 nerve roots) and points in the supraspinatus and infraspinatus muscles have been determined to be between 2.7 and 3.3 milliseconds, respectively. Increased latency on nerve conduction velocity studies may signify a nerve lesion such as entrapment or extrinsic compression.65 Denervation injuries typically reveal increased spontaneous activity, polyphasic signals, muscle fibrillations, positive sharp waves, and amplitude reduction on EMG.17,62,98, It must be noted, however, that these tests are both invasive and operator-dependent. In addition, positive results will not always accurately define the location or the pathological nature of the nerve lesion.27,98,109 According to a study of patients with pre-existing denervation injuries, preoperative EMG changes were predictive of patient outcome after nerve exploration and/or repair. Surprisingly, the least improvements were observed in patients with minor preoperative EMG changes. These authors hypothesized that more severe denervation was usually associated with significant intra-articular or extra-articular pathology that can be addressed at the time of surgery and that less severe damage may not improve with nerve decompression alone.3
Imaging Studies
Several imaging modalities can be utilized to identify potential sites of nerve injury. Standard radiographs of the cervical spine and the shoulder are typically the initial imaging studies to be evaluated. When clinically indicated, dedicated clavicle views may also be useful. A “Stryker Notch” view, an anteroposterior view of the scapula with the beam directed cephalad 15 to 30 degrees, allows improved visualization of the suprascapular notch. In general, radiographs are particularly useful for
patients with a suspected fracture. In the acute setting, fracture lines may be observed near the anatomically sensitive regions. In more chronic cases, callous or fibrous tissue may compress or entrap the nerve.
patients with a suspected fracture. In the acute setting, fracture lines may be observed near the anatomically sensitive regions. In more chronic cases, callous or fibrous tissue may compress or entrap the nerve.
In the majority of patients, however, radiographs are likely to be unremarkable.27,100,109 Computed tomography (CT scan) offers better delineation of the osseous architecture and may note the presence of an occult fracture or an ossified transverse scapular ligament. Unfortunately, similar to radiographs, CT scans are often unremarkable and may provide little additional diagnostic value.53
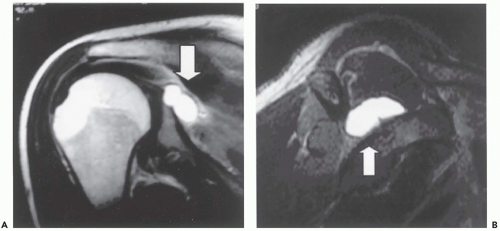
For most patients with a nerve injury, MRI often yields the most valuable information. MRI allows clear identification of various intra-articular and extra-articular soft tissue pathologies.53 In addition, it is particularly effective in identifying soft tissue masses that can injure or compress the suprascapular nerve.40 Ganglion cysts, for example, are readily visible on MRI. On T2-weighted images, cysts are seen as high signal, well-defined, masses, originating from the posterosuperior aspect of the glenohumeral joint27,43,53,59 (Fig. 33-4). If unclear, gadolinium can enhance the visualization of the cyst by increasing the signal intensity of its outer rim.27 Denervation changes within the muscle mass, such as fatty infiltration and decreased mass, are also well defined on MRI.40,59,67 Denervated muscles typically demonstrate high signal changes on the T2-weighted images and, according to one study, the degree of denervation correlated with the degree of signal intensity.59 In some images with sufficient resolution, the actual nerve can even be visualized. T2-weighted oblique sagittal views, for example, may demonstrate the suprascapular nerve as it courses through the suprascapular fossa.109
If an MRI is not readily available, ultrasonography may be utilized with some success in identifying ganglion cysts and other masses around the shoulder. A ganglion cyst will appear as a hypoechoic, well-defined homogeneous mass.51 Ultrasound may also detect muscle atrophy consistent with denervation.67 While ultrasonography offers a cost-effective alternative, it is operator dependent and may not be an accurate imaging modality in the hands of inexperienced operators.
Non-operative Treatment
In the absence of a compressive lesion or rotator cuff tear, a trial of non-operative therapy is typically the initial treatment of choice. In many patients who do not have a well-defined lesion, most of the symptoms should resolve spontaneously.79,99 Unfortunately, however, a significant amount of time, perhaps as long as 12 months, is often required for complete resolution of symptoms.109 Therefore, patient counseling is the key component to non-operative treatment. In addition, patients should be instructed to avoid repetitive overhead activities that can potentially irritate the nerve. Rehabilitation should focus on regaining and improving the flexibility, strength, and endurance of the shoulder girdle musculature. The scapular stabilizers are of particular importance in re-establishing proper glenohumeral and scapulothoracic kinematics.
The overall success rate of non-operative management is not well established in the literature and can vary widely among individual reports. For example, one series reported that all patients in their small series were successfully treated non-operatively33 while another reported that all patients in their study failed non-operative therapy and required surgical intervention.16 In a retrospective review of 15 patients with a follow-up of almost 4 years, Martin et al. reported that five excellent and seven good results were obtained after nonoperative management of isolated suprascapular neuropathy. The remaining three patients (20%) continued to suffer from persistent symptoms and required surgical management.79
Despite these conflicting reports, the likelihood of successful non-operative management appears to depend primarily on the etiology and location of the nerve lesion.27,109 In general, patients with a distal nerve injury without a discrete lesion are more likely to respond favorably to non-operative management. For example, one study reported that most patients with isolated infraspinatus muscle atrophy were successfully treated non-operatively as they obtained good pain relief, increased muscle mass, and improved strength at 6 to 12 months.27 Ferretti et al. reported similar results in their experience with 38 professional volleyball players who were suffering from isolated infraspinatus atrophy.38 Thirty-five patients (92%) responded well to non-operative treatment which consisted of rehabilitation focusing on external rotation strengthening exercises. These authors noted that isolated infraspinatus muscle atrophy did not affect the competitive performances of these athletes and that surgical intervention should be reserved for those patients suffering from persistent pain.38
In contrast to these reports, non-operative management of patients with a well-defined lesion, particularly ganglion cysts, appears to be associated with unfavorable outcomes.3,27,36,79 Cummins et al. performed a review of the literature and identified 21 cases of suprascapular nerve lesions secondary to ganglion cysts that were managed non-operatively. Five of these patients had complete resolution of their symptoms and another experienced partial relief. The remaining 15 patients (71%) had “unsuccessful” results with 9 patients requiring a surgical decompression.27 Similarly, Piatt et al. reported a 53% satisfaction rate in patients with spinoglenoid cysts treated nonoperatively, while 97% satisfaction rate was noted in patients managed with surgical cyst excision and labral repair.96 Thus, although patients with a discrete lesion can initially be managed non-operatively, they should be counseled that surgical intervention may ultimately be required.
For patients with a confirmed ganglion cyst, ultrasound or CT-guided aspiration may prove useful.40,51,119 In their review of the literature, Cummins et al. found eight such cases, all of which were associated with satisfactory pain relief at a shortterm follow-up.27 Aspiration, however, does not address the intra-articular pathology of the labrum that led to cyst formation. Thus, over time, the cysts may recur. According to one study, the rate of recurrent cyst formation after aspiration was as high as 48%.52 Therefore, while some short-term outcome reports may be promising, further experience with guided aspiration is necessary to document its long-term clinical efficacy, especially in patients with concurrent labral pathology.
Operative Treatment (Open)
Exploration and decompression of the suprascapular nerve has been the surgical treatment of choice. The surgical approach is usually dictated by the location and etiology of the lesion (Fig. 33-5). While an anterior approach to the suprascapular notch has been described, it has not been routinely utilized due to the difficult dissection, increased risk of neurovascular injuries, and poor visualization of the nerve.87,98,109, Therefore, the majority of the surgeons tend to use either the posterior or the superior approach to the nerve.
Initially described by Post and Mayer, the advantages of the posterior suprascapular nerve decompression include excellent exposure, limited risk to the neurovascular structures, and avoidance of major muscle damage.27,98 For this approach, the patient is placed in a semi-prone position with the arm draped free. The skin incision is made just superior, but parallel, to the scapular spine. The underlying trapezius muscle is then sharply elevated and retracted to expose the supraspinatus muscle. Once the supraspinatus muscle is retracted inferiorly, the transverse scapular ligament can be visualized. If the ligament is the source of the nerve lesion, it can be excised in its entirety. Otherwise, it is incised to expose the nerve and any compressing structures. Care should be taken to ensure that the vascular structures that lie just superior to the ligament are not injured. It has also been suggested by some authors that isolated ligament resection may be insufficient to decompress the nerve and that the nerve can still be tethered by its course over the notch.103 Therefore, in addition to ligament release, all resected edges of bone as well as the notch should be contoured to minimize any potential damage to the nerve.109
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree