Abstract
Objective
This study aimed at testing the ability of the superimposed electrical stimulation technique to restore the mobility of pre-stiff thumbs after operative repair for rupture of the ulnar collateral ligament.
Material and methods
Eight patients demonstrating a pre-stiff metacarpophalangeal joint were involved in two rehabilitation sessions of a counterbalanced design. In the voluntary contraction session, they performed 20 min of repeated active flexions of the impaired metacarpophalangeal joint. In the superimposed electrical stimulation session, they performed 20 min of percutaneous neuromuscular electrical stimulations which were superimposed to voluntary flexion.
Results
Mean active range of motion improvement from pre- to post-session was significantly greater in the superimposed electrical stimulation condition compared to the voluntary contraction condition (11 ± 5 deg versus 3 ± 4 deg; P < 0.01).
Conclusion
Superimposing electrical stimulation to voluntary contractions is an efficient technique to improve active range of motion of the pre-stiff metacarpophalangeal joint of the thumb.
Résumé
Objectif
Cette étude avait pour objectif de tester l’efficacité de la technique d’électrostimulation surimposée sur la mobilité du pouce pré-raide après réparation chirurgicale d’une rupture du ligament collatéral ulnaire.
Matériel et méthodes
Huit patients présentant une articulation métacarpo-phalangienne pré-raide ont participé à deux sessions de rééducation dans un modèle contrebalancé. Dans la session de contraction volontaire seule, les patients réalisaient 20 minutes de flexions actives de l’articulation métacarpo-phalangienne opérée. Dans la session de stimulation électrique surimposée, ils réalisaient 20 minutes de flexions de cette même articulation avec stimulation électrique transcutanée surimposée à la contraction volontaire.
Résultats
L’amélioration des amplitudes articulaires actives pré- versus post-test était significativement supérieure dans la condition de stimulation électrique surimposée en comparaison de la condition active volontaire (11 ± 5 deg versus 3 ± 4 deg ; p < 0,01).
Conclusion
Surimposer une stimulation électrique à la contraction musculaire volontaire est une technique efficace pour améliorer l’amplitude de l’articulation métacarpo-phalangienne de pouces pré-raides.
1
English version
1.1
Abbreviations
MP
metacarpophalangeal joint
SES
superimposed electrical stimulation
UCL
ulnar collateral ligament
VAS
visual analogic scale
VOL
voluntary active contraction
1.2
Introduction
Rupture of the ulnar collateral ligament (UCL) of the metacarpophalangeal joint (MP) of the thumb, also called the skier’s (acute) or gamekeeper’s thumb (chronic), is frequently associated to injuries to the dorsal capsule, palmar plate, and adductor aponeurosis . Post-surgically, the thumb is immobilized during 4 to 6 weeks which increases the risk of stiffness . As range of motion loss is an important factor for patient dissatisfaction with the outcome of UCL surgery , avoiding stiffness (i.e., a permanent loss of range) is a priority.
In rehabilitation, stiffness resulting from inflammation and adhesions is one of the potentially incapacitating complications that often challenges therapeutic skills . Joint mobilization has already proved to be efficient in preventing stiffness. Specifically, joint mobilization increases tensile strength of the wound , directs the alignment and orientation of collagen fibers , enhances tendon gliding , reduces tendon adhesions and limits joint stiffness . However, in some cases, adherences between tissues can remain despite the use of classical rehabilitative techniques. In this context, studies that have investigated the effects of electrical stimulation on range of motion recovery may be of interest . Indeed, adhesions are mainly composed of collagen, a tissue whose resistance to gradual deformation by tensile stress (i.e., viscosity) depends on its previous history of length changes . This mechanical property is defined as thixotropy . As a consequence, artificially prolonging the stress imposed to adhesions would reduce their viscosity and result in greater deformation of this tissue. Clinically, it would prevent stiffness for a longer period of time thereby increasing the possibility for recovering greater range of motion. The superimposed electrical stimulation technique , i.e., percutaneous electrical stimulation superimposed to a voluntary muscle contraction, has recently proved to prolong the muscle ability to repeat maximal contractions without altering force parameters over time .
Here, we intended to compare, for the first time, the effects of voluntary muscular contraction (VOL) and superimposed electrical stimulation (SES) on the range of motion recovery of pre-stiff MP of the thumb after operative repair of UCL. It was hypothesized that the SES technique would be more efficient than VOL to restore joint mobility of the thumb’s MP joint.
1.3
Material and methods
1.3.1
Patients
Eight volunteers (age: 43 ± 12 years; 3 females) were recruited among patients who were undergoing treatment within a hand therapy center (Centre grenoblois de rééducation de la main et du membre supérieur, France) to resume functional use of their thumb after UCL surgery (different surgeons). Postoperatively, the involved MP joint was immobilized in a thermoplastic splint for 4 weeks . After these 4 weeks, patients were allowed to start active gentle flexion/extension exercises . Resistive work was started at 6 weeks . To be included in the study, patients had to be between 20 and 65 years old. In addition, after 8 weeks post-surgery (61 ± 9 days) all patients who demonstrated a loss of range of motion in the injured MP of at least 10 deg (31 ± 9 deg) when compared to the opposite thumb and whose range was not improving anymore using classical rehabilitative techniques (i.e., pre-stiff patients) were included in the study. Exclusion criteria were a history of complex regional pain syndrome, peripheral vascular disease, peripheral neuropathy, central nervous system dysfunction, and diabetes. Features of the patient sample are reported in Table 1 . Patients provided written informed consent and their rights were protected as required by the Helsinki Declaration (1964) and the local Ethics Committee.
| Patient | Age | Injury | Surgery | ROM deficit | Pain | Days post-surgery |
|---|---|---|---|---|---|---|
| 1 | 35 | Corporeal tear | Direct suture of the UCL to itself | 29° | 1.7 | 80 |
| 2 | 37 | Stener lesion | Intraosseous suture anchor (Mitek) | 20° | 1.0 | 56 |
| 3 | 43 | Distal tear | Direct suture of the UCL to the periosteum | 30° | 0.2 | 60 |
| 4 | 52 | Stener lesion | Intraosseous suture anchor (Mitek) | 22° | 0.3 | 59 |
| 5 | 63 | Proximal tear | Direct suture of the UCL to the periosteum | 10° | 0.0 | 54 |
| 6 | 50 | Proximal tear | Direct suture of the UCL to the periosteum | 15° | 0.3 | 53 |
| 7 | 38 | Distal tear | Direct suture of the UCL to the periosteum | 16° | 0.0 | 59 |
| 8 | 25 | Proximal tear | Direct suture of the UCL to the periosteum | 18° | 0.1 | 70 |
1.3.2
Task and procedures
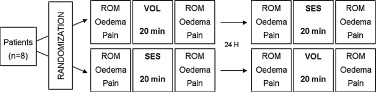
Patients were seated, their shoulder abducted approximately 15 deg and neutrally rotated, elbow flexed 110 deg, forearm in a neutral position and wrist extended 30 deg. Prior to sessions, 5 min of passive mobilizations were performed by a physiotherapist at the carpometacarpal, MP and interphalangeal joints of the thumb. Patients were then instructed to maximally bend their thumb each time they felt electrical stimulation. This task was performed in two experimental conditions (VOL and SES) of 20 min each in a counterbalanced design ( Fig. 1 ). All patients performed the two conditions 24 hours apart. Order of the conditions was randomized across patients. Patients were acquainted with the protocol and the sensation of neuromuscular electrical stimulation through participation in a single practice session prior to testing. The primary study endpoint was the range of motion in the injured MP. In this preliminary study, the variance value was unknown which prevented from computing the number of required participants.
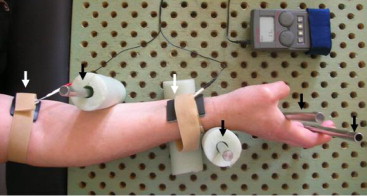
For electrical stimulation, a portable stimulator (Danmeter ® , Elpha 2000 model) was used to deliver constant current, rectangular, symmetric, biphasic pulses. Train characteristics were the following : 30 Hz frequency, 200 μs pulse duration, and 40% duty cycle (4 s on, 6 s off). Trains were delivered at a self-set maximal tolerated intensity (15 ± 5 mA). Electrical stimulation was applied using two stainless steel electrodes covered with a wet sponge (3.5 × 2 cm) placed on the involved upper extremity and maintained onto the skin with hook-and-loop fasteners. Sponge electrodes were preferred to adhesive ones to easily adjust positioning and get maximal effect on the MP joint. The proximal electrode was positioned onto the elbow flexion crease, medially to the biceps brachii tendon, onto the median nerve that is closer to the skin at this point. The distal electrode was positioned at the forearm, on the flexor pollicis longus muscle which is close to the anterior aspect of the radius. Stimulation of the flexor pollicis longus muscle was preferred to the flexor pollicis brevis because pre-tests showed greater efficiency of this positioning for MP flexion. Exact positioning choice of the muscular electrode varied from individual to individual based on which position allowed the best thumb MP flexion. To set the pace in the VOL condition, electrical trains were delivered at a sensitive intensity on the forearm of the non-injured side. Because of the neuromuscular electrical stimulation, joint blocking was required to focus muscular actions on the MP . Specifically, blocking of the wrist was carried out through a hand therapy pegboard ( Fig. 2 ).
Immediately before and after each session, active range of motion, pain, and oedema of participants were collected by the same physical therapist who was blinded to the tested condition. Range of motion was measured using a finger goniometer (EMS Physio ® ) on the dorsal aspect of MP . Goniometry of active MP range of motion has demonstrated intrarater reliability ranging from 0.64 to 0.93 (intraclass coefficient) and method errors ranging from 1.23 to 3.47 deg . Pain and oedema were respectively assessed by means of a visual analogue scale (VAS) and joint perimeter.
1.3.3
Data analysis
To test VOL and SES effects on range of motion, pain, and oedema, the difference between pre- and post-session scores was computed for each patient. Results were then submitted to a t -test for paired samples. Level of significance was set at P < 0.05.
1.4
Results
As illustrated in Fig. 3 A , descriptive results evidenced a greater range of flexion post-SES as compared to post-VOL. No patients were lost to follow-up.
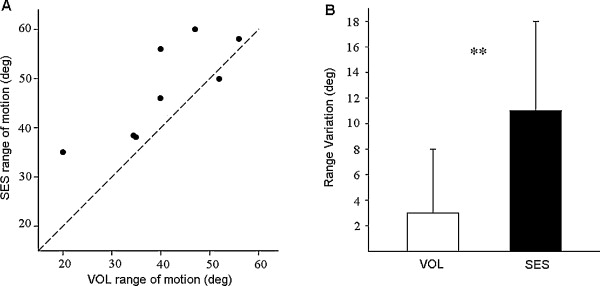
As illustrated in Fig. 3 B, analysis of the range of motion variation demonstrated that range improvement between pre- and post-session measures was significantly greater in the SES compared to VOL condition (11 ± 5 deg versus 3 ± 4 deg; mean ± S.D.; P < 0.01). The range of motion variation was significantly different from zero in the SES condition ( P < 0.05) but not in the VOL one ( P > 0.05). Levels of post-VOL and post-SES pain were very low (VAS score = 0.7 ± 0.8 and 1.0 ± 0.9, respectively) and not different from pre-test (VAS score = 0.4 ± 0.6 and 0.5 ± 0.7, respectively; Ps > 0.05). The VOL and SES conditions had no significant effect on oedema (perimeter variation = 1 ± 1 mm in both conditions; Ps > 0.05). Patients reported no side effects.
1.5
Discussion
This study tested the effects of the superimposed electrical stimulation technique versus voluntary active contraction on the range of active flexion in pre-stiff metacarpophalangeal joints of the thumb after operative repair of the ulnar collateral ligament.
Results demonstrated that superimposing electrical stimulation to muscle contraction resulted in greater range improvement as compared to voluntary mobilizations alone. More specifically, the superimposed electrical stimulation technique succeeded in restoring active mobility in ranges that were no longer accessible through voluntary mobilizations. These results in pre-stiff joint support previous studies in non-stiff joints where electrical stimulation was also efficient to recover range of motion after interphalangeal sprain or tenolysis of hand’s flexor tendons . Thixothropy, the history-dependent resistance to gradual deformation , is likely to constitute the theoretical basis that explains the present and previous results. Indeed, the superimposed electrical stimulation imposes maximal stress on adhesions for a longer period of time compared to voluntary contractions and thereby reduces adhesions’ viscosity . As a consequence, resistance of adhesions to gradual deformation is weaker and range of motion recovery improves.
The absence of side effects, together with the absence of pain and oedema differences across conditions and between pre- and post-session values, suggests that the superimposed technique is not going beyond the physiological limits of the metacarpophalangeal joint tissues. The fact that superimposed electrical stimulation technique had no effect on oedema is not surprising at this late stage of the rehabilitation process as there is generally no oedema anymore. This result rules out the possibility for the range improvement to be explained by a reduced oedema and confirms that adhesions’ lengthening is the main reason for range improvement when electrical stimulation is superimposed to voluntary contraction.
In conclusion, the superimposed electrical stimulation technique should be considered as an efficient tool to recover range of motion in the pre-stiff metacarpophalangeal joint of the thumb.
The results of the present study call for additional studies testing the effect of electrical stimulation techniques on range of motion improvement. Sample sizes of these studies should be larger than the present one to avoid limited inferences to the general population. In addition, future studies should include a longer follow-up and investigate the clinical importance of such range improvement by means of functional tests .
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Abbréviations
MP
articulation métacarpo-phalangienne
SES
stimulation électrique surimposée
LCU
ligament collatéral ulnaire
EVA
échelle visuelle analogique
VOL
contraction active volontaire
2.2
Introduction
La rupture du ligament collatéral ulnaire (LCU) de l’articulation métacarpo-phalangienne (MP) du pouce, aussi appelée le « pouce du skieur », est fréquemment associée à des lésions de la capsule dorsale, de la plaque palmaire et de l’aponévrose de l’adducteur . Après chirurgie, le pouce est immobilisé pendant 4 à 6 semaines , ce qui augmente les risques de raideur . Étant donné que la perte d’amplitude articulaire est une importante source d’insatisfaction du patient suite à la chirurgie du LCU , éviter la raideur (i.e., une perte de mobilité permanente) est une priorité.
En rééducation, la raideur résultant de l’inflammation et des adhérences est une complication potentiellement invalidante qui complique souvent la prise en charge du patient . La mobilisation articulaire a déjà montré son efficacité pour prévenir cette raideur. Elle permet notamment d’améliorer la résistance des tissus à la traction , d’organiser l’alignement et l’orientation des fibres de collagène , d’améliorer le glissement des tendons , de réduire les adhérences , et de limiter la raideur articulaire . Cependant, dans certains cas, des adhérences peuvent persister malgré l’utilisation de techniques de rééducation classiques. Dans ce contexte, les études qui se sont intéressées aux effets de l’électrostimulation sur la récupération des amplitudes articulaires pourraient s’avérer intéressantes . En effet, les adhérences sont principalement composées de collagène, un tissu dont la résistance à une déformation graduelle imposée par une force de traction (i.e., la viscosité) dépend des déformations préalables . Cette propriété mécanique se nomme la thixotropie . Ainsi, prolonger artificiellement la tension imposée aux adhérences réduirait leur viscosité et produirait une déformation plus importante de ces tissus pour une même force de traction. Cliniquement, cela permettrait de lutter contre la raideur articulaire sur une période de temps plus longue et augmenterait les possibilités de récupérer de la mobilité articulaire. La technique de stimulation électrique neuromusculaire surimposée , i.e., une stimulation électrique percutanée surimposée à une contraction volontaire, a récemment montré qu’elle pouvait prolonger la capacité du muscle à répéter des contractions maximales sans altérer les paramètres de force au cours du temps .
Dans cette étude, nous comparons, pour la première fois, les effets de la contraction musculaire volontaire (VOL) et de la technique de stimulation électrique surimposée (SES) sur la récupération d’amplitude articulaire de l’articulation MP de pouces pré-raides après réparation du LCU. Nous faisons l’hypothèse que la technique SES sera plus efficace que la VOL pour restaurer la mobilité de l’articulation MP.
2.3
Matériel et méthodes
2.3.1
Patients
Huit volontaires (âge : 43 ± 12 ans, 3 femmes) ont été recrutés parmi des patients pris en charge dans un centre spécialisé (Centre grenoblois de rééducation de la main et du membre supérieur, France) pour retrouver un usage fonctionnel de leur pouce après chirurgie réparatrice du LCU (différents chirurgiens). Suite à l’opération, l’articulation MP était immobilisée 4 semaines dans une attelle thermoformée . À la fin de ces 4 semaines, les patients étaient autorisés à commencer des exercices doux de flexion/extension active . Le travail contre résistance était initié à 6 semaines post-opératoires . Pour être inclus dans cette étude, les patients devaient être âgés de 20 à 65 ans. En outre, après 8 semaines post-opératoires (61 ± 9 jours), tous les patients présentant un déficit d’amplitude articulaire d’au moins 10 deg par rapport au pouce opposé (31 ± 9 deg) et dont la mobilité ne s’améliorait plus à l’aide des méthodes de rééducation classiques (i.e., patients pré-raides) étaient inclus dans cette étude. Les critères d’exclusion étaient des antécédents de syndrome douloureux régional complexe, une maladie vasculaire périphérique, une neuropathie périphérique, un dysfonctionnement du système nerveux central et du diabète. Les caractéristiques des patients sont présentées dans le Tableau 1 . Les patients ont été informés et ont donné leur consentement écrit, libre et éclairé. Leurs droits étaient protégés comme prévu par la déclaration d’Helsinki (1964) et le comité d’éthique local.









