Stepwise Approach to Taylor Spatial Frame for the Foot and Ankle
John J. Stapleton
Vasilios D. Polyzois
Thomas Zgonis
Introduction
On the basis of the design of the Taylor spatial frame (TSF), one of the main applications is to correct long bone deformities. Deformity analysis requires the interpretation of radiographs to determine the level and plane of deformity. The TSF incorporates the mathematical field of deformity analysis to develop an external fixator that is capable of creating a single-axis hinge to correct a six-axis deformity. The TSF is a modification of an Ilizarov circular external fixation system that utilizes six telescoping rods that are free to rotate at their fixation points of the proximal and distal circular ring and/or external foot plate. Through adjustments of the length of each of the telescoping rods between two circular rings, or a circular ring and an external foot plate, the device can be preconstructed to mimic and resemble any deformity. TSF has become very advantageous in cases where conventional circular external fixation constructs require extensive modifications throughout the postoperative period to perform the necessary deformity corrections on various planes. The purpose of this chapter is not to discuss the intrinsic details to perform deformity corrections but to provide the reader some of the most common applications in deformity correction for the foot and ankle. TSF can often become very difficult to treat complex foot and ankle deformities since the deformity is not only multiplanar but also coexists in multilevel segments within close proximity. When dealing with deformities of the long bones multiple TSF constructs can be applied to correct the deformity at each level. At the foot and ankle level, the proximity of these deformities often prevents proper deformity analysis and radiographic evaluation of the TSF in relation to the deformity. In addition, the realistic utilization of multiple TSF constructs at the foot and ankle level can become very cumbersome and difficult to manage for both the patient and the surgeon. On the contrary, the strength sustained with a TSF along with its dynamic capabilities become advantageous to manage various complex foot and ankle pathologies. While conventional circular external fixators can typically be utilized for the majority of foot and ankle cases, inherent advantages to the TSF are discussed and presented throughout this chapter.
Indications/Contraindications
Some of the most common indications for the utilization of TSF include and are not limited to deformity corrections of complex midfoot, rearfoot, ankle, and supramalleolar conditions. Its main advantage over a traditional circular external fixator is its inherent stability with precise and more predictable deformity correction outcomes.
Other common indications for the foot and ankle include severely neglected clubfoot deformities, equinus contractures, burn injuries, and combined multilevel rearfoot and ankle deformities (Clinical Cases I–III). Another indication of the TSF is ankle and/or subtalar joint arthrodiastasis while simultaneously correcting deformity at the ankle or supramalleolar level (Clinical Case IV).
More common applications at the ankle level include but are not limited to an ankle arthrodesis, revisional tibiotalocalcaneal arthrodesis, and where absolute osseous stability and union is required to achieve bone healing for high-risk patients. TSF can also be utilized to perform distraction osteogenesis in combination with deformity corrections and/or rearfoot and ankle arthrodesis. Morbidly obese patients who would potentially pose significant stress to a traditional circular external fixator can be further stabilized with a TSF to prevent any unwanted postoperative lower leg malpositioning and frame instability. Charcot neuroarthropathy (CN) of the midfoot, rearfoot, and/or ankle can also be addressed with a TSF. The unique 6 × 6 butt frame is beneficial for select Charcot rocker-bottom midfoot deformities. Its inherent stability is beneficial for allowing the TSF to have a static role after an acute correction is obtained at the time of surgery and to also perform necessary dynamic corrections if necessary during the postoperative course.
Relative contraindications include and are not limited to surgical procedures that cannot be adequately addressed secondary to the crowding of the TSF struts. An example of this is a triple arthrodesis that requires placement of smooth transosseous wires in close proximity to adequately compress the affected joints. A TSF can be cumbersome to perform this procedure since the necessary wire fixation on the external foot plate is limited to provide compression. For this reason,
the surgeon has to carefully assess the degree and planes of deformity in addition to concomitant procedures that may need to be performed to adequately determine if a TSF is required.
the surgeon has to carefully assess the degree and planes of deformity in addition to concomitant procedures that may need to be performed to adequately determine if a TSF is required.
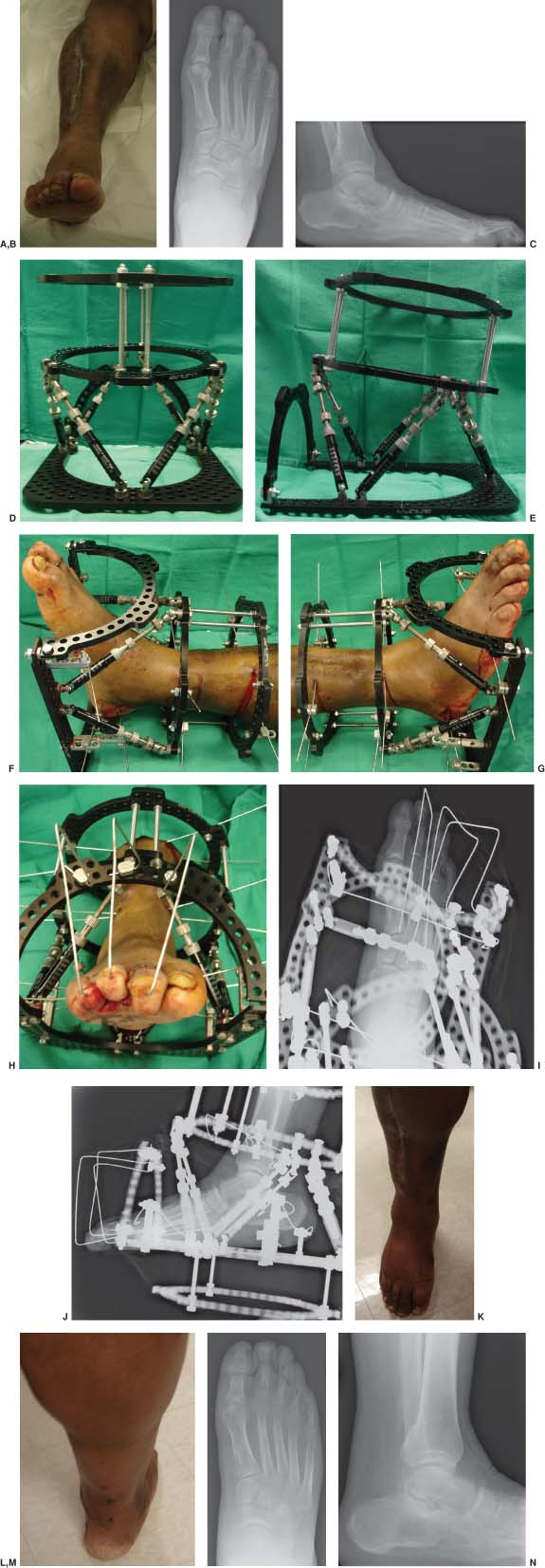
Clinical Case I
Clinical (A) and radiographic anteroposterior (B) and lateral (C) views of a right lower extremity showing the severe ankle equinus deformity and contracted digits as a result of a previous gunshot injury and skin contractures from grafting. Patient underwent a percutaneous tendo-Achilles lengthening with flexor tenotomies and pinning of digits 2 to 5 to the right foot (D–J). Please note the preassembled TSF construct (D, E) that is mimicking the ankle equinus deformity of the patient. The external fixator was removed at approximately 7 weeks and the patient was transitioned to a non–weight bearing cast immobilization for approximately 4 weeks followed by appropriate surgical boot off-loading and aggressive physical therapy exercising program. Final clinical (K, L) and radiographic (M, N) views at 5-month follow-up showing the equinus and multiple contracted digits correction.
 |
Peripheral vascular disease is often a contraindication to proceed with deformity correction and application of a TSF. The surgeon needs to adequately evaluate the peripheral circulation and if compromised appropriate referral to a vascular surgeon for a necessary intervention may be warranted prior to the procedure. Absolute contraindications of the TSF include and are not limited to a noncompliant patient who is not capable of making gradual corrections if required.
Preoperative Considerations
Deformity Planning
Surgical planning involves a thorough physical examination of the patient and deformity analysis interpreting weight bearing radiographs of the lower extremity. Examining the patient initially while standing and ambulating if possible is preferred. The surgeon can quickly develop an understanding of suprastructural deformity or compensatory changes that are present. Limb length discrepancy, pelvic obliquity, frontal plane deformity of the knee, and position of the heel to the lower leg are assessed. Evaluating the range of motion about the ankle and rearfoot is important to determine compensatory contractures that may be evident. Limited range of motion and contractures of the subtalar joint are commonly encountered with coronal supramalleolar and/or ankle deformities. Malposition of the talus and limited subtalar joint range of motion is commonly encountered with posttraumatic deformities involving the ankle and rearfoot. In the normal foot, there is considerably less eversion than inversion of the subtalar joint. For this reason, supramalleolar/ankle varus deformities are less compensated for than valgus deformities. Equinus contractures of the ankle are also evaluated to determine if capsular,
gastrocnemius, or Achilles deformities need to be addressed at the time of surgery. Any coexisting anterior ankle bone block impingement conditions are also assessed when planning for deformity correction.
gastrocnemius, or Achilles deformities need to be addressed at the time of surgery. Any coexisting anterior ankle bone block impingement conditions are also assessed when planning for deformity correction.
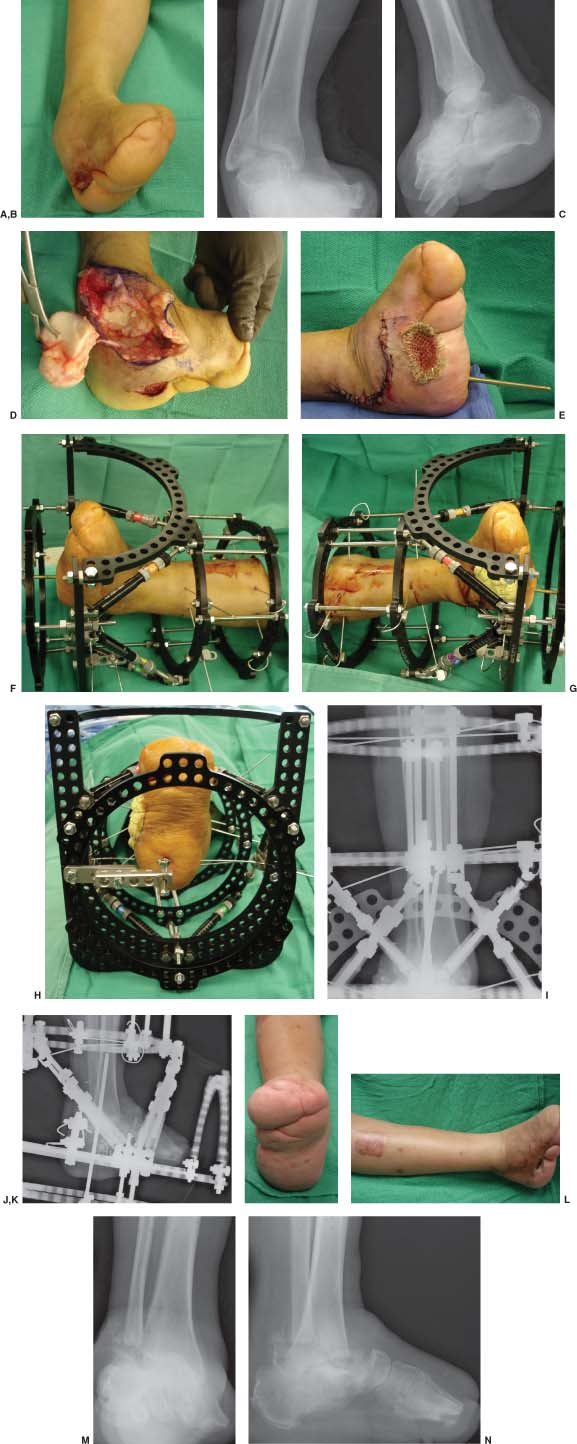
Clinical Case II
Clinical (A) and radiographic anteroposterior (B) and lateral (C) right ankle views of a diabetic patient with a severe equinocavovarus deformity and chronic ulcerations after a surgical treatment for a transmetatarsal amputation. Patient underwent an initial incision and drainage procedure that was followed 6 days later by a total talectomy (D) with tibiocalcaneal arthrodesis, bone allografting, and split thickness skin grafting at the lateral aspect of the right foot (E). This was accomplished by the utilization of the TSF construct for compression and stabilization of the right lower extremity (F–J). The external fixator was removed at approximately 7 weeks and the patient was transitioned to a non–weight bearing cast immobilization for approximately 6 weeks followed by appropriate surgical boot off-loading and accommodative orthotic devices. Final clinical (K, L) and radiographic (M, N) views at 15-month follow-up.
 |
Planning of deformity correction starts with weight bearing radiographs of bilateral lower extremities. Full-length radiographs are beneficial to determine limb length discrepancy and to evaluate the mechanical axis of the lower extremity. Often, the determination to performing an opening-wedge, dome, or closing-wedge osteotomy is dependent on the limb length along with the plane of deformity compared to the contralateral leg. The mechanical axis of the distal tibia should be in alignment with the mechanical axis of the lower extremity. The mechanical axis extends through the center of the ankle joint under normal circumstances. In addition, the angle formed between the mechanical axis and the tibial plafond on a weight bearing anteroposterior and lateral radiographs are determined with normal values averaging 93 and 80 degrees, respectively.
The ultimate goal of performing deformity correction is to restore the limb to these normal parameters while considering
the position of the contralateral leg. In evaluation of deformities about the ankle, one must consider the position of the talus, calcaneus, and forefoot in relation to the tibia. Hindfoot and rearfoot malposition is best evaluated on hindfoot alignment radiographs. The calcaneal axis should be parallel and 5 mm lateral to the mid-diaphyseal line of the tibia in normal circumstances. Coronal plane deformities of the forefoot must be evaluated to determine their influence on the position of the calcaneus. For example, a plantarflexed first ray can lead to compensatory varus deformity of the calcaneus. Understanding these normal parameters is essential before attempting any type of deformity correction for the foot and ankle. In addition, most of the deformities are multiplanar and can involve coronal and sagittal components that can be present at different levels. Multiplanar deformities are measured by their center of rotation and angulation (CORA). The CORA is the bisection of
the mechanical axis of the proximal and distal segment of the deformity to be corrected. If the corrective osteotomy is performed at the level of the CORA, then angular and rotational deformities can be corrected without translation. The difficulty arises when angular and rotational deformities are performed away from the CORA. In these circumstances, the distal segment will need to be translated in addition to the angular and rotational corrections to adequately align the lower extremity while preventing a secondary translational deformity.
the position of the contralateral leg. In evaluation of deformities about the ankle, one must consider the position of the talus, calcaneus, and forefoot in relation to the tibia. Hindfoot and rearfoot malposition is best evaluated on hindfoot alignment radiographs. The calcaneal axis should be parallel and 5 mm lateral to the mid-diaphyseal line of the tibia in normal circumstances. Coronal plane deformities of the forefoot must be evaluated to determine their influence on the position of the calcaneus. For example, a plantarflexed first ray can lead to compensatory varus deformity of the calcaneus. Understanding these normal parameters is essential before attempting any type of deformity correction for the foot and ankle. In addition, most of the deformities are multiplanar and can involve coronal and sagittal components that can be present at different levels. Multiplanar deformities are measured by their center of rotation and angulation (CORA). The CORA is the bisection of
the mechanical axis of the proximal and distal segment of the deformity to be corrected. If the corrective osteotomy is performed at the level of the CORA, then angular and rotational deformities can be corrected without translation. The difficulty arises when angular and rotational deformities are performed away from the CORA. In these circumstances, the distal segment will need to be translated in addition to the angular and rotational corrections to adequately align the lower extremity while preventing a secondary translational deformity.
The TSF is commonly utilized to address these types of severe deformities about the foot and ankle. Typically, the magnitude of these deformities is high and clinical scenarios are complex and hence the need for the TSF as opposed to more traditional fixation methods. Careful evaluation of the current neurovascular status is paramount to determine if these structures are at risk for further injury or if concomitant prophylactic nerve decompressions need to be performed at the time of deformity correction. Commonly, with severe varus deformity corrections a tarsal tunnel release may need to be performed to prevent further nerve injury to the posterior tibial nerve. The soft tissue is a structure at risk with severe deformity corrections. The surgeon needs to consider previous soft tissue coverage such as flaps, previous scar contractures, and compromised areas in deciding incision placement and for determining the rate of deformity correction to decrease tension of the surrounding soft tissues thereby preventing potential wound complications.
Detailed Surgical Technique
Taylor Spatial Frame for Supramalleolar Deformity Correction
The circular rings are placed independently to the proximal and distal segments of deformity correction. The proximal fixation segment for these types of deformities can be addressed by placing one circular ring or a tibial block to the proximal
segment. The proximal ring or tibial block is placed to optimally fit the proximal leg and is aligned orthogonal to the axis of the proximal tibia. This is typically accomplished by first placing a frontal plane smooth wire from a lateral to medial direction and securing it to the circular ring ensuring that the ring is perpendicular to the tibia under C-arm fluoroscopy. An additional half-pin is also inserted from an anterior to posterior direction across the anterior crest of the tibia securing the alignment of the proximal ring. At this time, an additional ring is applied if a proximal tibial block is desired. Typically, for deformity correction two smooth wires and a half-pin are applied to each ring if two rings are utilized. If one ring is placed to secure the proximal segment, then two smooth wires attached directly to the ring and two to three half-pins extended from the ring with rancho cubes are utilized to enhance frame stability. The proximal or the distal ring to the proximal tibial block is then referred to as the “reference” ring. The next step is to assemble the distal circular ring. The ring is aligned distal to the proposed osteotomy and is typically aligned with the distal aspect of the tibia metaphysis. The distal ring is secured with two crossed smooth wires and a half-pin. The proximal ring or tibial block is then connected to the distal tibia ring with the TSF struts. At this point, the origin and the corresponding point along with the mounting parameters must be established. The origin typically utilized is the center of the bone segment on the proximal side of the deformity while the corresponding point is the center of the bone segment on the distal side of the deformity. The goal is to reduce the moving segment (corresponding point) to the origin. The four mounting parameters required describe the location of the origin to the reference ring, which is the proximal tibia ring that was placed orthogonal to the proximal tibia. The mounting parameters consist of defining the distance of the center of the reference ring from the origin and the anteroposterior (sagittal), medial/lateral (coronal), axial, and rotatory frame offset. Six deformity parameters then establish
the spatial relationship of the origin and the corresponding point. The deformity parameters describe the rotation and translation of the origin and the corresponding point in the coronal, sagittal, and axial plane. Once the frame, mounting, and deformity parameters are established they can be entered into the Internet-based software (www.spatialframe.com). The speed of correction and structures at risk are determined and the program will provide a daily schedule for the patient to perform adjustments on each numbered of the six struts. Close monitoring of the deformity correction and clinical appearance is paramount to the patient’s successful postoperative outcome (Clinical Case V).
segment. The proximal ring or tibial block is placed to optimally fit the proximal leg and is aligned orthogonal to the axis of the proximal tibia. This is typically accomplished by first placing a frontal plane smooth wire from a lateral to medial direction and securing it to the circular ring ensuring that the ring is perpendicular to the tibia under C-arm fluoroscopy. An additional half-pin is also inserted from an anterior to posterior direction across the anterior crest of the tibia securing the alignment of the proximal ring. At this time, an additional ring is applied if a proximal tibial block is desired. Typically, for deformity correction two smooth wires and a half-pin are applied to each ring if two rings are utilized. If one ring is placed to secure the proximal segment, then two smooth wires attached directly to the ring and two to three half-pins extended from the ring with rancho cubes are utilized to enhance frame stability. The proximal or the distal ring to the proximal tibial block is then referred to as the “reference” ring. The next step is to assemble the distal circular ring. The ring is aligned distal to the proposed osteotomy and is typically aligned with the distal aspect of the tibia metaphysis. The distal ring is secured with two crossed smooth wires and a half-pin. The proximal ring or tibial block is then connected to the distal tibia ring with the TSF struts. At this point, the origin and the corresponding point along with the mounting parameters must be established. The origin typically utilized is the center of the bone segment on the proximal side of the deformity while the corresponding point is the center of the bone segment on the distal side of the deformity. The goal is to reduce the moving segment (corresponding point) to the origin. The four mounting parameters required describe the location of the origin to the reference ring, which is the proximal tibia ring that was placed orthogonal to the proximal tibia. The mounting parameters consist of defining the distance of the center of the reference ring from the origin and the anteroposterior (sagittal), medial/lateral (coronal), axial, and rotatory frame offset. Six deformity parameters then establish
the spatial relationship of the origin and the corresponding point. The deformity parameters describe the rotation and translation of the origin and the corresponding point in the coronal, sagittal, and axial plane. Once the frame, mounting, and deformity parameters are established they can be entered into the Internet-based software (www.spatialframe.com). The speed of correction and structures at risk are determined and the program will provide a daily schedule for the patient to perform adjustments on each numbered of the six struts. Close monitoring of the deformity correction and clinical appearance is paramount to the patient’s successful postoperative outcome (Clinical Case V).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








