Stepwise Approach to Static Circular External Fixation
John J. Stapleton
Vasilios D. Polyzois
Thomas Zgonis
Introduction
The successful outcome for utilizing static circular external fixation is determined not only by careful procedure and patient selection but also by understanding the fundamental principles and designs of external fixation to prevent the risk of potential complications. The term static, for purposes of this chapter, will be used for the description of a pre-built circular external fixation that provides osseous stability for various foot and ankle pathologies. This design can also have dynamic functions such as joint distraction or compression if desired. Pre-built or partially built circular external fixation devices with a similar design can be applied in an expedited manner and are used in many case scenarios as they are very beneficial for the surgical management of deformities, posttraumatic conditions, neuromuscular disorders, diabetic complications, and revisional surgery.
The goal of this chapter is to discuss the indications in which this design is advantageous along with providing the reader a step-by-step technical approach to its application in various foot and ankle conditions. Technical pearls and meticulous details are also discussed.
Indications/Contraindications
The indications for the utilization of a static circular external fixation are numerous. The main advantage inherent to this external fixation system is the reproducibility of using a similar design to manage a variety of conditions involving the midfoot, rearfoot, and ankle. However, the capability to treat such a wide variety of foot and ankle pathology with a static circular external fixation requires a significant learning curve and surgical experience of the complex surgical procedures in order to produce a successful outcome.
Some of the most common indications for this external fixation device include but are not limited to midfoot, rearfoot, and ankle arthrodesis for posttraumatic arthrosis, malunions and/or nonunions, Charcot neuroarthropathy (CN), gross deformity, neuromuscular disorders, avascular necrosis of the talus, previous history of infection or septic joint, and salvage of a failed ankle arthroplasty. These clinical case scenarios are often not amenable to the sole use of internal fixation; therefore, external fixation becomes a salvage tool to achieve osseous stability while protecting the soft tissue envelope. At times, the use of internal fixation can be supplemented with external fixation to enhance osseous stability and/or to promote an earlier weight bearing status (Clinical Cases I–V).
Static circular external fixation may also be beneficial in the acute management of diabetic ankle fractures and/or dislocations to provide further stabilization in the presence of dense peripheral neuropathy. Furthermore, static circular external fixation can provide additional stability when combined with internal fixation to avoid the possible development of acute CN with unstable fracture patterns and anticipated premature weight bearing (Clinical Case VI).
Static circular external fixation is indicated for a majority of diabetic limb salvage cases involving the midfoot, rearfoot, and ankle. CN with unstable deformities, malunions, and/or nonunions of the foot and ankle can often be addressed with a pre-built static circular external fixation. Other common indications in the diabetic population include limb-threatening conditions such as infected hardware and/or previous failed surgeries with infected wounds and ulcerations. Static circular external fixation is beneficial to achieve osseous stability, deformity correction, salvage arthrodesis and to surgically off-load and stabilize the soft tissue envelope for the majority of diabetic limb salvage cases. Soft tissue immobilization is crucial among diabetic patients with open wounds that often require plastic surgical reconstruction in addition to their osseous procedure(s) (Clinical Cases VII–IX).
The contraindications of static circular external fixation usually do not pertain to the application of the device but rather to the procedure that is performed in conjunction. Key points to consider as contraindications are the presence of severe peripheral vascular disease with limb ischemia not amenable to revascularization and active infection with systemic manifestations. External fixation is often utilized to limit soft tissue dissection and to avoid the placement of retained hardware. These two advantages inherent to external fixation often lead to its use in the patient population with peripheral arterial disease and/or history of infection. For this reason, a thorough preoperative
vascular examination of the lower extremity determines if static circular external fixation with its proposed procedure would be contraindicated. A systematic and rational approach to the management of deep osseous and soft tissue infections needs to be performed before the application of the external fixation device. Active, untreated infection is a contraindication to the utilization of a static circular external fixation.
vascular examination of the lower extremity determines if static circular external fixation with its proposed procedure would be contraindicated. A systematic and rational approach to the management of deep osseous and soft tissue infections needs to be performed before the application of the external fixation device. Active, untreated infection is a contraindication to the utilization of a static circular external fixation.
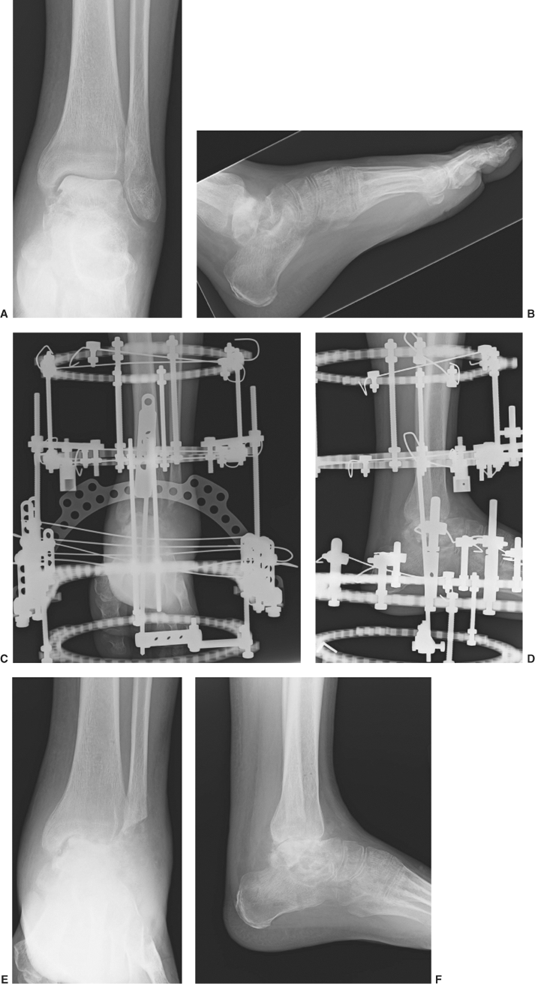
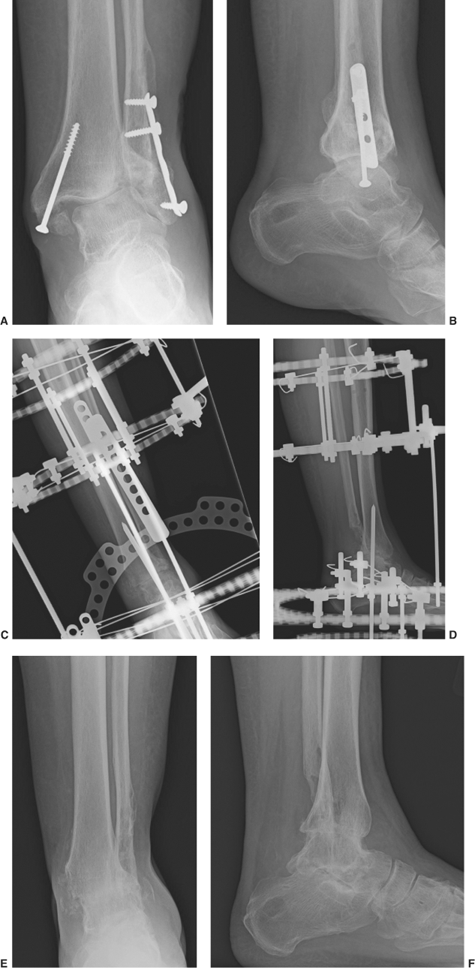
Clinical Case I
Anteroposterior (A) and lateral (B) ankle radiographic views showing the preoperative lower extremity equinocavovarus deformity from a post-polio syndrome. The patient had a prior history of a midfoot arthrodesis, Achilles tendon lengthening, and resection of the distal fibula with a failed outcome. An ankle arthrodesis was performed with the utilization of Steinmann pins and static circular external fixation. Please note the alignment of the lower extremity and the utilization of the tibial block connected to the foot plate (C, D). The external fixation device was maintained for about 10 weeks and the patient was then transitioned to a knee–ankle–foot orthosis with permitted weight bearing status. Final radiographic views at 1 year postoperatively showing successful arthrodesis and alignment of the lower extremity (E, F).
 |
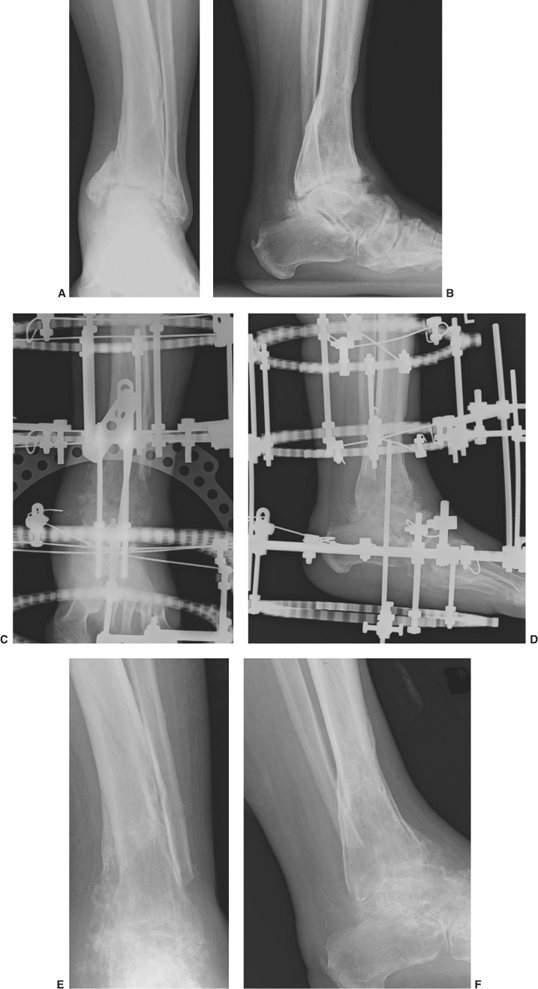
Clinical Case II
Preoperative anteroposterior (A) and lateral (B) ankle radiographic views showing the avascular necrosis of the talus with collapse after a nonunion of a talus fracture. A tibiotalocalcaneal arthrodesis was performed with the utilization of Steinmann pins and static circular external fixation (C, D). The external fixation device was removed at 10 weeks postoperatively and the patient was then transitioned to a non–weight bearing below the knee cast application for 4 weeks followed by a weight bearing status with the cast application for an additional 2 weeks. Final radiographic views at 9 months postoperatively showing successful arthrodesis at the subtalar joint and stable pseudoarthrosis at the ankle joint (E, F).
 |
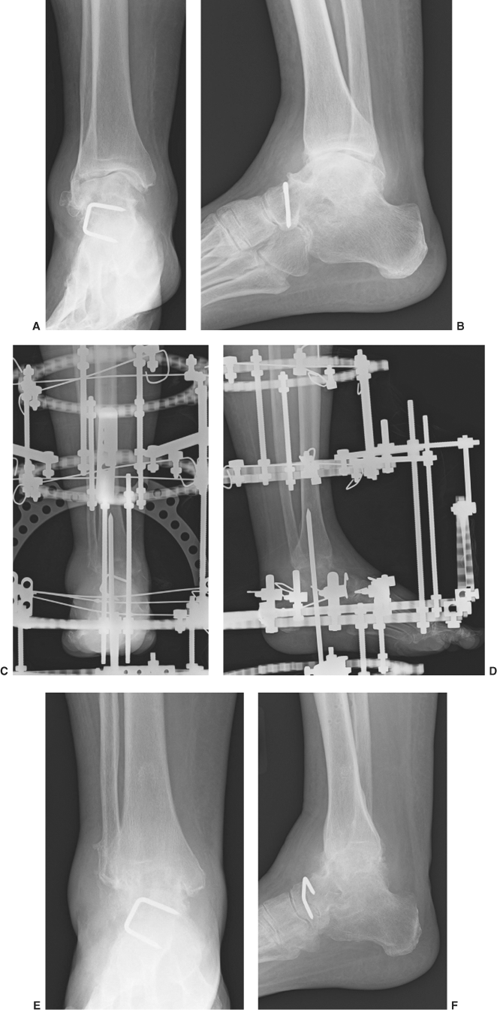
Clinical Case III
Preoperative anteroposterior (A) and lateral (B) ankle radiographic views showing posttraumatic arthrosis and varus deformity of the subtalar and ankle joints secondarily to a malunion of a distal tibia fracture. A tibiotalocalcaneal arthrodesis was performed with the utilization of Steinmann pins and static circular external fixation (C, D). The external fixation device was removed at about 10 weeks postoperatively and the patient was transitioned to a weight bearing cast for another 4 weeks. The patient resumed full ambulation with regular shoes and returned to his normal daily activities. Final radiographic views at 1 year postoperatively showing successful arthrodesis at both subtalar and ankle joints (E, F).
 |
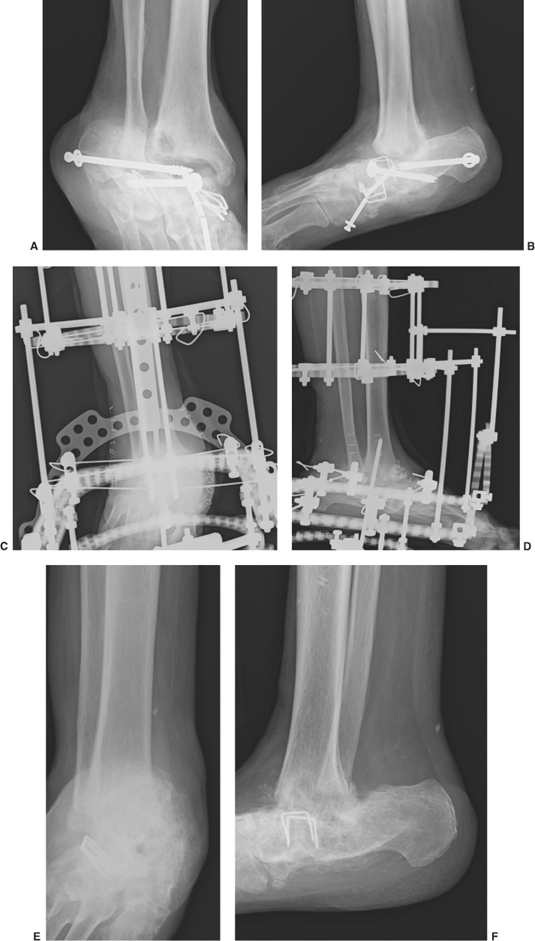
Clinical Case IV
Preoperative anteroposterior (A) and lateral (B) ankle radiographic views showing ankle joint arthrosis and equinocavovarus deformity after a triple arthrodesis for a neuromuscular foot deformity correction. An ankle arthrodesis with an acute deformity correction was performed with the utilization of Steinmann pins and static circular external fixation (C, D). The external fixation device was removed at about 10 weeks postoperatively and the patient was transitioned to a weight bearing cast for another 4 weeks. The patient resumed an ambulatory status with regular shoe gear and without any bracing. Final radiographic views at 10 months postoperatively showing successful arthrodesis at the ankle joint with deformity correction (E, F).
 |
Clinical Case V
Preoperative anteroposterior (A) and lateral (B) ankle radiographic views demonstrating osteomyelitis of the ankle joint with resorption of the talar body. The patient had a history of rheumatoid arthritis and a failed triple arthrodesis. Initially, all internal hardware was removed and a thorough surgical debridement of the remaining talus and distal tibia was performed with the insertion of nonabsorbable cemented antibiotic impregnated beads at the ankle joint. The inserted antibiotic beads were removed at about 6 weeks and a revisional tibiocalcaneal arthrodesis was performed with the utilization of Steinmann pins and static circular external fixation (C, D). The external fixation device was removed at about 12 weeks postoperatively and the patient was transitioned to a non–weight bearing cast for 2 weeks followed by a weight bearing cast for an additional 2 weeks. The patient resumed full ambulation with an extra depth rocker bottom shoe at 5 months postoperatively. Final radiographic views at 1 year postoperatively showing successful osseous union at the tibiocalcaneal arthrodesis site (E, F).
 |
Clinical Case VI
Preoperative anteroposterior (A) and lateral (B) ankle radiographic views demonstrating a nonunion/malunion of a bimalleolar ankle fracture. A draining sinus laterally and deep infection involving the hardware and fibula were evident. Initially, all infected hardware was removed and the infected bone was debrided and packed with cemented antibiotic impregnated beads. Negative pressure wound therapy was also utilized at the open wound. The inserted antibiotic beads were removed at about 6 weeks and an ankle arthrodesis was performed with the utilization of Steinmann pins and static circular external fixation (C, D). The external fixation device was removed at about 12 weeks postoperatively and the patient was transitioned to a non–weight bearing cast for 2 weeks followed by a weight bearing cast for an additional 4 weeks. Final radiographic views at about 1 year postoperatively showing successful osseous union at the ankle joint with slight valgus deformity (E, F).
 |
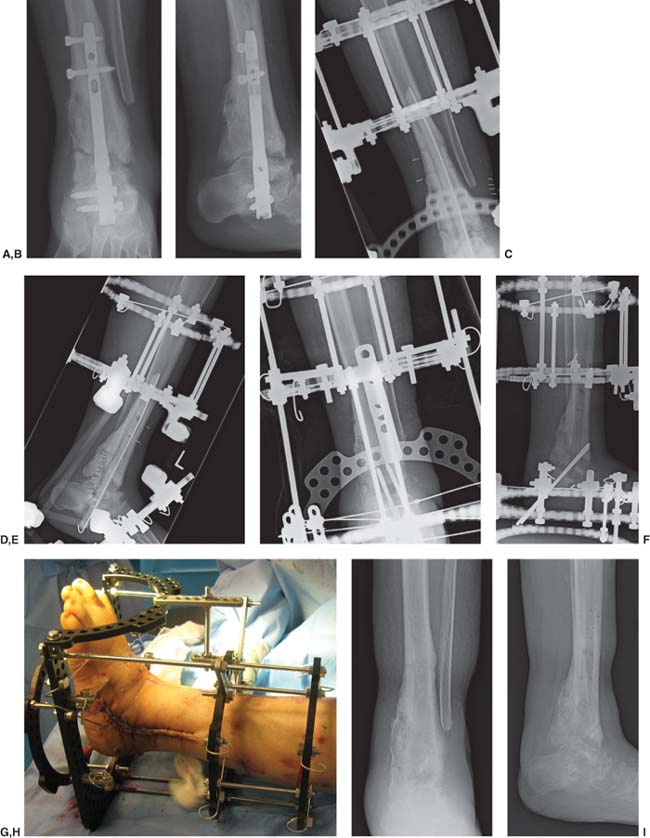
Clinical Case VII
Preoperative anteroposterior (A) and lateral (B) ankle radiographic views demonstrating an infected nonunion of a tibiotalocalcaneal arthrodesis with an intramedullary rod for a diabetic Charcot ankle in a hemodialysis-dependent patient. Initially, the deep infection and osteomyelitis was managed with removal of the intramedullary rod, extensive osseous and soft tissue debridement, and reaming of the entire medullary canal of the tibia. An antibiotic impregnated cemented rod was then inserted at the previous attempted arthrodesis site and the lower extremity was stabilized with a hybrid external fixation system (C, D). The inserted antibiotic cemented rod was removed at about 6 weeks and a revisional tibiotalocalcaneal arthrodesis was performed with the utilization of Steinmann pins and static circular external fixation (E–G). The external fixation device was removed at about 12 weeks postoperatively and the patient was transitioned to a non–weight bearing cast for 4 weeks. Final radiographic views at about 6 months postoperatively showing a stable pseudoarthrosis without any clinical evidence of infection (H, I).
 |
Clinical Case VIII
Preoperative anteroposterior (A) and lateral (B) foot radiographic views demonstrating a rocker-bottom diabetic Charcot neuroarthropathy deformity. Initially, an extensive osseous and soft tissue debridement was performed and intraoperative bone biopsy did confirm osteomyelitis of the midfoot bones from the plantar chronic ulceration. After systemic antibiosis treatment, the patient was brought back to the operative room for an “internal” midfoot amputation and stabilization of the remaining joints with Steinmann pins and static circular external fixation (C–E). The external fixation system provided assistance to the acute shortening and compression of the diabetic Charcot foot. The external fixation device was removed at about 8 weeks postoperatively and the patient was transitioned to a non–weight bearing cast for 2 weeks followed by a weight bearing cast for an additional 2 weeks. Final radiographic views at about 6 months postoperatively showing stable pseudoarthrosis with shortening of the diabetic Charcot midfoot (F, G).
 |
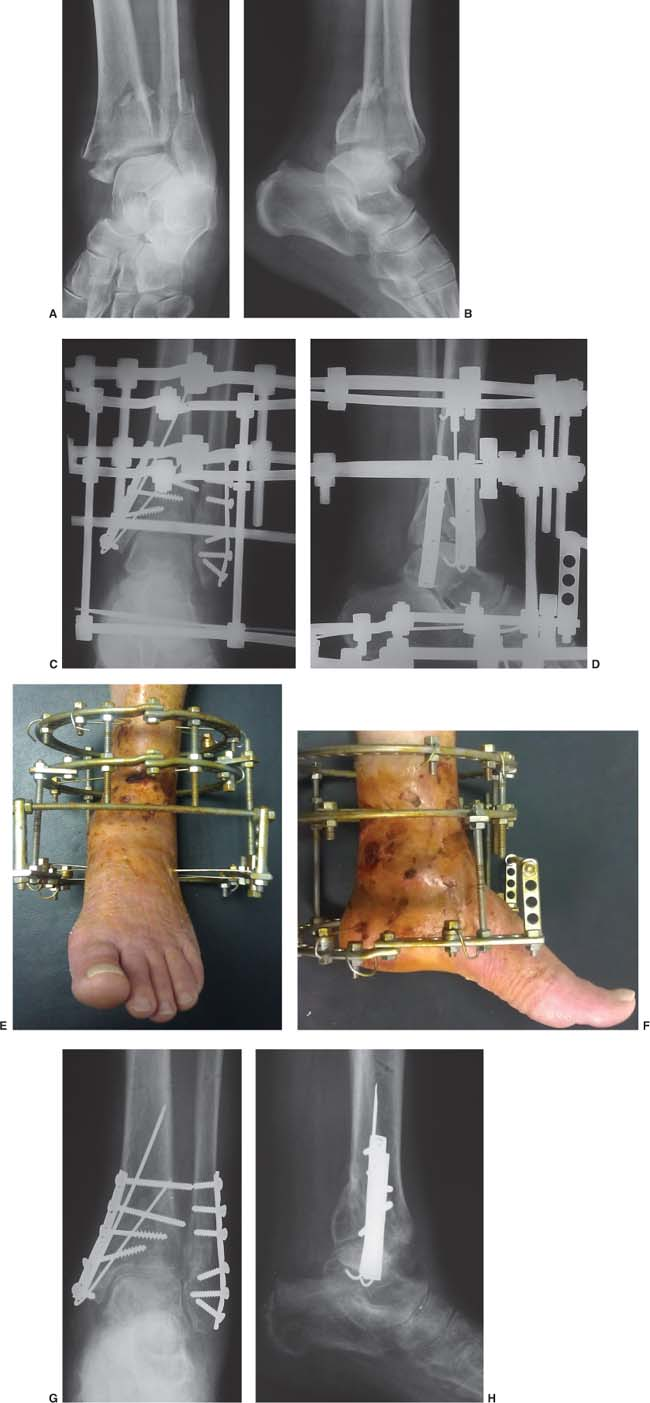
Clinical Case IX
Preoperative anteroposterior (A) and lateral (B) ankle radiographic views demonstrating a high-energy pilon fracture/dislocation in a patient with a history of diabetes mellitus. The patient underwent reduction of the severe injury with the use of internal fixation supplemented by a static circular external fixation for further stability and protection of the soft tissue envelope. Radiographic (C, D) and clinical (E, F) views at 6 weeks postoperatively showing anatomic alignment and healing of the soft tissue injury. The static circular external fixator was removed at approximately 18 weeks after surgery (G, H).
 |
History of noncompliance with treatment is a relative contraindication. Psychosocial issues may need to be addressed prior to surgery and while they might not be an absolute contraindication, they may have implications with the postoperative regimen. On the contrary, in certain case scenarios in which the need for additional osseous stabilization achieved with a static circular external fixation is required among the noncompliant patient, the procedure is performed as the anticipation of hardware failure, nonunion, malunion, and/or amputation is feasible. Amputation may also be preferable in certain patients who are nonambulatory in the presence of a lower extremity deformity, peripheral vascular disease, and severe infection.
Preoperative Considerations
Determining the Appropriate Size of the Static Circular External Fixation
In adults, circular ring sizes that are most commonly utilized are between 155 and 205 mm while the external foot plates range between 155 and 180 mm dependent on the manufacturer. Custom made external fixation circular rings and foot plates may need to be made if a larger ring diameter is required. The static circular external fixation consists of two tibia circular rings and an external foot plate. These rings are initially assembled with two threaded rods measuring approximately 120 to 150 mm in size and are placed in opposite directions bisecting the center of the ring. The placement of these threaded rods will align with the anterior crest of the tibia once assembled. This “tibial block” which consists of the two tibia rings is then connected to the foot plate with two threaded rods measuring approximately 150 to 200 mm in length and located within the posterior central portion of the foot plate (Clinical Case X).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








