Stepwise Approach to Forefoot Elective and Reconstructive Surgery with External Fixation
Paul S. Cooper
Introduction
The use of uniplane monolateral external fixation in the forefoot comprises bone and joint distraction, scar extension, and arthrodesis of the metatarsophalangeal joint (MTPJ). Further, the monolateral external fixator is a useful adjunct for nonhealing sub-metatarsal ulcers in conjunction with soft tissue repair. Forefoot deformities by virtue of the condensed anatomy and skeletal geometry are best addressed with uniplane monolateral external fixators. External fixator configurations consist of rail and hinged designs, with half-pins ranging from threaded 2 to 3 mm in diameter (Figures 13.1 and 13.2).
Detailed Surgical Technique
Brachymetatarsia
Brachymetatarsia consists of a congenitally shortened metatarsal, most frequently involving the fourth metatarsal. Main indications for surgical correction include transfer metatarsalgia of the adjacent bones, often associated with toe drift. While small degrees of shortening may be addressed with direct lengthening and intercalary bone grafting, greater degrees run the risk of neurovascular compromise and dislocation of the MTPJ. External fixation allows for a slow gradual metatarsal lengthening minimizing these risks (Clinical Case I).
 Figure 13.1. Examples of various modified uniplane monolateral external fixators with and without hinges. |
 Figure 13.2. Examples of 2 and 3 mm threaded half-pins for the application of a monolateral external fixator. |
The first half-pin is located under C-arm fluoroscopic guidance distally into the metatarsal head and is directed perpendicular to the longitudinal axis of the metatarsal involved (Figures 13.3 and 13.4). Once this is confirmed, the desired uniplane monolateral external fixator is slid over the half-pin to be used as a drill guide for insertion of the other pins (Figures 13.5 and 13.6). The adjustment end should be facing proximal for patient ease in turning daily the necessary bolts. Following this, the external fixator is adjusted in length to ideally position the proximal pins into the base of the metatarsal shaft and diaphyseal bone as confirmed under C-arm fluoroscopy. In choosing the proper length fixator, factor in the amount of lengthening involved in the process (Figure 13.7). The proximal pins are then drilled and locked into place, followed by the remaining distal pins (Figures 13.8 and 13.9). There should be a minimum of two half-pins per corticotomy side of the uniplane monolateral external fixator.
Clinical Case I
Clinical (A) and radiographic (B) views of a congenital left fourth brachymetatarsal that was symptomatic with an overlapping fifth digit. Percutaneous metatarsal corticotomy with a Gigli saw (C) and an application of a uniplane monolateral external fixator (D). Postoperative radiographs (E, F) showing the mid-diaphyseal corticotomy and final outcome after the external fixation removal (G).
 |
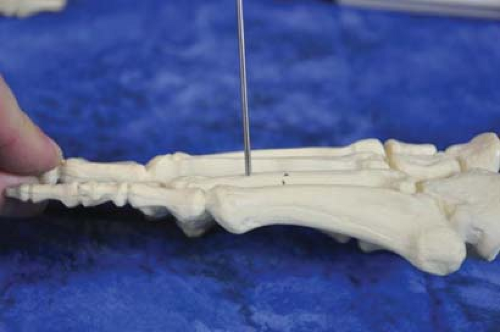 Figure 13.4. Example showing the distal half-pin insertion perpendicular to the longitudinal axis of the involved metatarsal. |
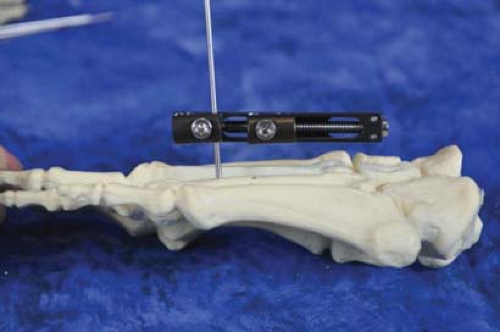 Figure 13.5. Example of proper alignment reference with external fixator parallel to the involved metatarsal. |
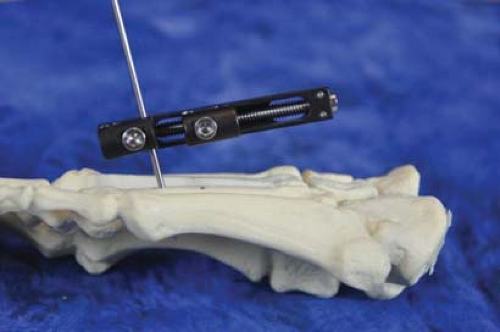 Figure 13.6. Example of a malpositioned half-pin setting the external fixator divergent from metatarsal shaft. |
 Figure 13.7. The adjustment end should be facing proximal for patient ease in turning daily the necessary bolts. |
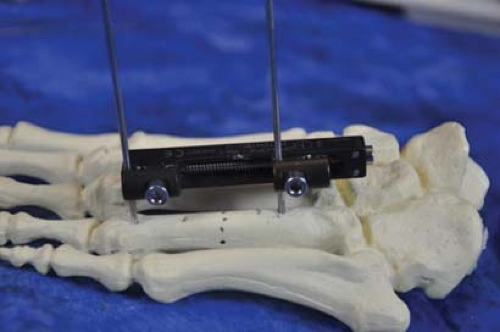 Figure 13.8. Second pin inserted proximal into the metatarsal base. The external fixator is adjusted prior to half-pin insertion for maximum lengthening excursion. |
 Figure 13.9. Example of a minimum of two half-pins per corticotomy side of the uniplane monolateral external fixator. |
Next, the external fixator is removed, and a small longitudinal (less than 1 cm) incision is made at the desired point of mid-diaphyseal or diaphyseal–metaphyseal corticotomy. Dissection includes preservation of the periosteum protected by soft tissue Hohmann retractors. The corticotomy may be performed by several methods including multiple drill holes and an osteotome, sagittal saw and osteotome or Gigli wire saw (Figures 13.10 and 13.11). Following successful corticotomy, the uniplane monolateral external fixator is re-applied with sufficient distance to allow for soft tissue swelling. Several turns to establish preliminary axial lengthening and full corticotomy is performed and confirmed under C-arm fluoroscopy if the desired lengthening is in axial alignment with the shaft of the metatarsal (Figure 13.12). Frequently, the MTPJ of the involved metatarsal may sublux during the lengthening procedure and should be provisionally stabilized with a 0.062-in. Kirschner wire during the lengthening process (Figure 13.13).
First Metatarsophalangeal Joint Arthrodesis and Arthrodiastasis
Arthrodesis of the first MTPJ with external fixation is indicated in dysvascular cases where soft tissue dissection is risky, and as a salvage procedure for infected primary arthrodesis with conventional internal fixation. The uniplane monolateral external fixator may also be used in staged reconstructive cases of excessive metatarsal or phalangeal shortening, where the soft tissues are stretched first and followed by arthrodesis at the lengthened position as a second procedure.
Following extensive MTPJ preparation, an appropriate monolateral external fixator is chosen to be applied medially. Factors involved in choosing the appropriate external fixator include the mechanism for compression and ability to address rotating, translational and sagittal plane correction. Many monolateral external fixators have a cannulated hinge where a guide pin can be placed to determine the MTPJ center
(Figure 13.14A–C). The first half-pin is dictated by the proximal phalanx and should be inserted perpendicular to the axial length of the proximal phalanx (Figure 13.15). The monolateral external fixator is then applied and the distal clamp temporarily tightened to be used as a pin template for the proximal pins. The monolateral external fixator should be set to two-thirds maximum length before inserting the proximal pins so as to allow room in the mechanism for adequate compression excursion. The second half-pin is inserted proximally at the most proximal hole in the metatarsal pin clamp centered over the base of the first metatarsal (Figure 13.16). With hinged monolateral external fixators, it is important to center the hinge over the isometric center point of the MTPJ or otherwise an asymmetric alignment when correction of the sagittal plane position will occur (Figures 13.17–13.19).
(Figure 13.14A–C). The first half-pin is dictated by the proximal phalanx and should be inserted perpendicular to the axial length of the proximal phalanx (Figure 13.15). The monolateral external fixator is then applied and the distal clamp temporarily tightened to be used as a pin template for the proximal pins. The monolateral external fixator should be set to two-thirds maximum length before inserting the proximal pins so as to allow room in the mechanism for adequate compression excursion. The second half-pin is inserted proximally at the most proximal hole in the metatarsal pin clamp centered over the base of the first metatarsal (Figure 13.16). With hinged monolateral external fixators, it is important to center the hinge over the isometric center point of the MTPJ or otherwise an asymmetric alignment when correction of the sagittal plane position will occur (Figures 13.17–13.19).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










