Stepwise Approach to Foot and Ankle Osteomyelitis and External Fixation
Roberto H. Rodriguez
Luke C. Jeffries
Thomas Zgonis
Introduction
Osteomyelitis of the foot and ankle remains a serious and common complication associated with traumatic, iatrogenic, diabetic, and ischemic etiologies. Advances in technology and surgical strategies have sharpened the surgeon’s ability to diagnose and treat osteomyelitis of the foot and ankle. The judicious use of external fixation in conjunction with wide surgical debridement, heat-stable impregnated antibiotic-loaded cement, negative pressure wound therapy (NPWT), orthobiologics, soft tissue coverage procedures, and final stage arthrodesis has become a useful approach in foot and ankle salvage surgery.
Because of the relatively superficial depth of osseous structures, vulnerable vasculature, abundance of avascular tendinous and ligamentous structures, the foot is particularly at high risk of infection in the setting of a wound, whether it is traumatically or surgically induced. When there is a history of diabetes, peripheral vascular disease, or tobacco use, this risk is compounded. The presence of normal skin flora on the lower extremity may convert traumatically induced soft tissue deficits into grossly infected wounds with contiguous involvement of adjacent osseous structures. Aggressive surgical resection, intravenous antibiotics, and the stabilization of osseous segments have become the standard approach for managing lower extremity osteomyelitis. Definitive reconstruction of osseous defects through arthrodesis of involved joints with a stable and functional soft tissue envelope represents the ultimate goal in creating a functional plantigrade foot. This goal, however, can be a major challenge to even the most experienced reconstructive surgeon. Relatively minor bone loss can be addressed with bone grafting; more significant loss requires more challenging procedures, including distraction osteogenesis, alone or in combination with soft tissue reconstructive procedures. Selective digital or ray amputation for the management of terminal sites of osteomyelitis may be required to avoid total limb loss.
The primary intraoperative goal in the treatment of osteomyelitis is the radical debridement of infected and devitalized bone, which often conflicts with the simultaneous desire to maintain limb length and function. External fixation allows the spanning of osseous segments with simultaneous use of heat-stable local antibiotics in the form of polymethyl methacrylate (PMMA) antibiotic-loaded cement spacers or beads. Circular external fixation allows off-loading of the surgical lower extremity while simultaneously providing access to soft tissue defects for interim NPWT in lieu of definitive soft tissue coverage through advanced plastic surgery techniques, such as local muscle, pedicle, or free flaps. Soft tissue closure is deferred after the complete eradication of osteomyelitis. Furthermore, external fixation can stabilize the osseous segments adjacent to the surgical wound and allow utilization of bone grafts during the final reconstructive stage.
Compression techniques through the use of external fixation can provide a stable, plantigrade foot through arthrodesis without the use of internal fixation at the previously infected site. The use of NPWT improves the postoperative management of surgical wounds and allows joint arthrodesis with exposed bone graft through the Papineau technique. External fixation can be adjusted gradually to achieve proper alignment and length. Rigid stability of bone and soft tissue can prevent further infection, while promoting continual osseous consolidation and soft tissue closure.
Given its complexity, the successful management of lower extremity osteomyelitis requires the cooperative efforts of multidisciplinary specialties, including and not limited to a reconstructive foot and ankle surgeon, vascular surgeons, infectious disease specialists, and internal medicine, among others. The benefits of a multidisciplinary team approach have been validated in the literature, and the failure to recognize this will likely result in a poor outcome.
Indications/Contraindications
Most common clinical scenarios in which the use of external fixation is indicated for the management of osteomyelitis in the foot and ankle include and are not limited to the following: Presence of broken or loosened hardware, Charcot neuroarthropathy (CN), nonunions, unstable deformities, significant bone loss, osteopenia, osteonecrosis, and exposed bone and joint structures (Clinical Cases I–IV).
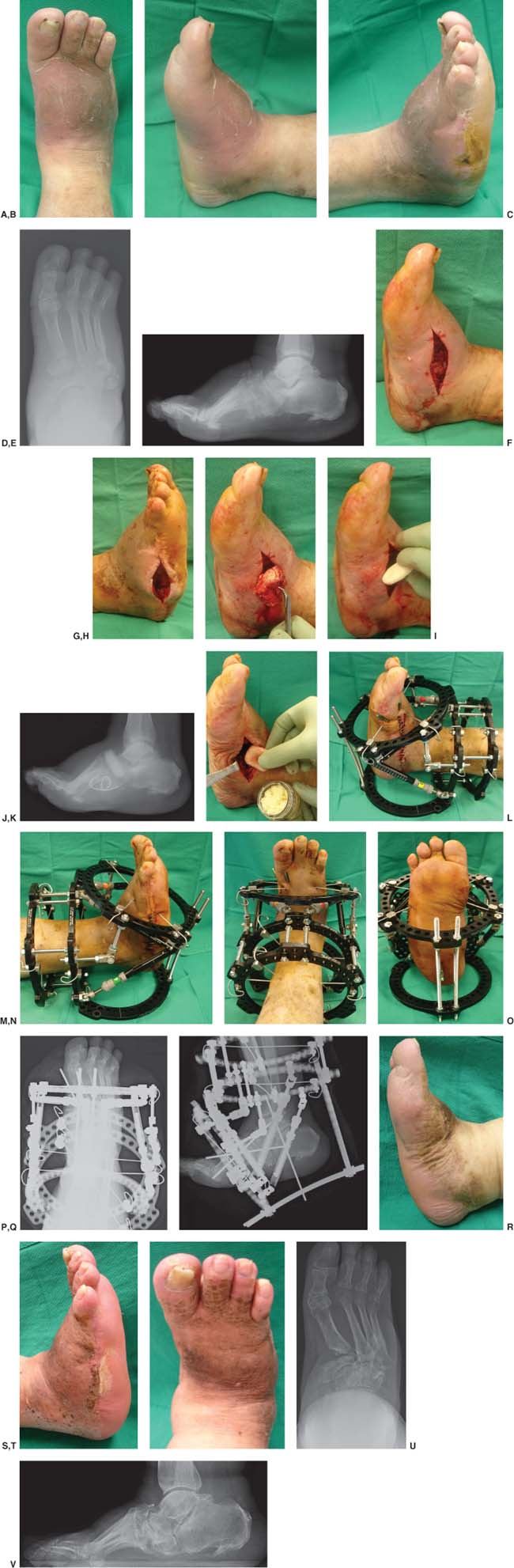
Clinical Case I
Clinical (A–C) and radiographic anteroposterior (D) and lateral (E) views showing an infected diabetic Charcot neuroarthropathy right foot with abscess and osteomyelitis. The patient presented with systemic signs of infection and had a history of open wounds and partial fifth ray amputation. The patient underwent an initial multiple incision and drainage procedure and obtaining of deep intraoperative bone and soft tissue cultures and bone biopsy (F, G). Cultures were positive for osteomyelitis of the medial cuneiform and base of fifth metatarsal. The patient returned to the operating room 2 days after the first surgery for an entire resection of the medial cuneiform (H) and fifth metatarsal base and insertion of a nonbiodegradable antibiotic-cemented spacer (I) and beads at the medial and lateral columns of the foot, respectively (J). Three months later, the patient returned to the operating room for removal of any retained nonbiodegradable antibiotic-cemented spacers and beads and further obtaining of intraoperative cultures. The final-staged reconstructive procedure was performed 5 days later with a medial column arthrodesis and osteotomy, allogenic bone grafting (K), and skeletal fixation of the subtalar and ankle joints by using a Taylor spatial frame (L–Q). The external fixation device was removed at approximately 7 weeks and the patient was transitioned to a non–weight bearing cast immobilization for approximately 6 weeks followed by appropriate surgical boot off-loading and accommodative orthotic devices. The patient required an additional incision and drainage procedure medially and eventually healed at his last 14-month follow-up (R–V).
 |
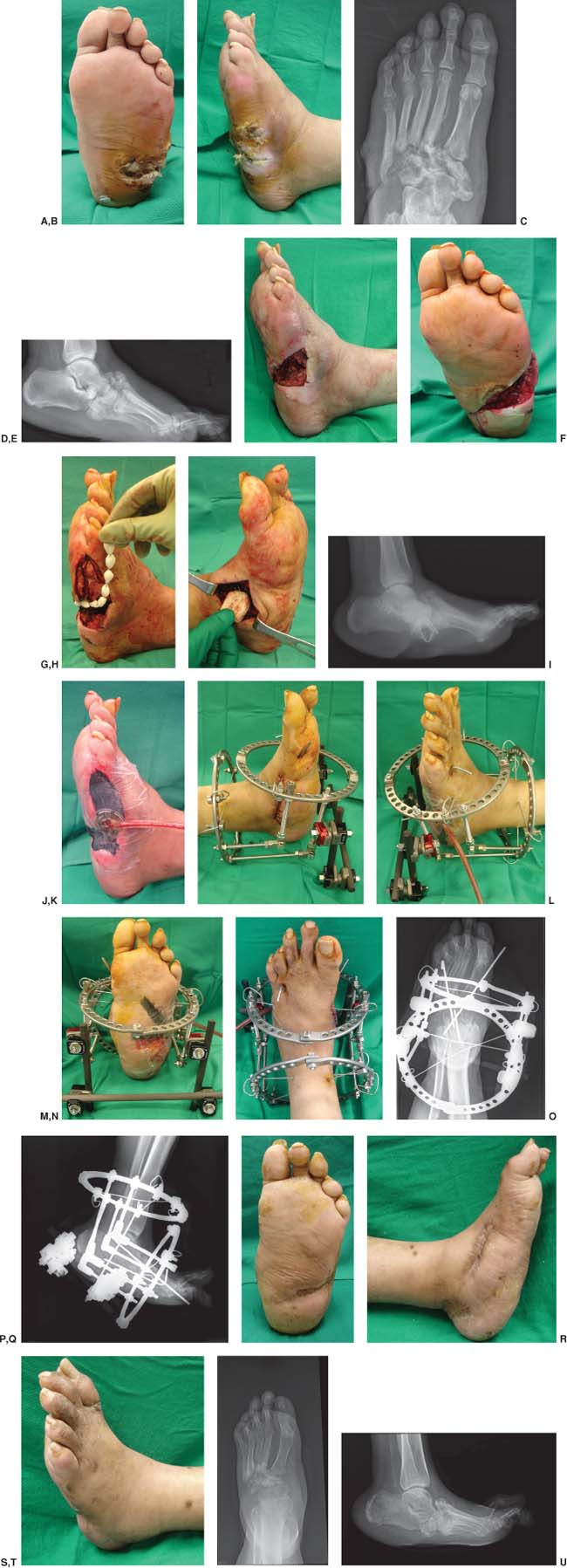
Clinical Case II
Clinical (A, B) and radiographic anteroposterior (C) and lateral (D) views showing a severely infected Charcot neuroarthropathy left foot with abscess and osteomyelitis. The patient presented with systemic signs of infection and had a history of open wounds to the left foot with associated trauma and non-diagnosed diabetes mellitus. The patient underwent an initial multiple incision and drainage procedure and obtaining of deep intraoperative bone and soft tissue cultures and bone biopsy (E, F). Cultures were positive for osteomyelitis and the patient returned to the operating room 5 days after the first surgery for an entire resection of the navicular and medial cuneiform with partial resection of the fifth metatarsal base and insertion of nonbiodegradable antibiotic-cemented beads (G) and spacer (H) at the lateral and medial columns of the foot, respectively (I). An intraoperative negative pressure wound therapy (NPWT) device was also utilized to cover the large plantar soft tissue deficit as well (J). At approximately 3 months later, the patient returned to the operating room for removal of the retained nonbiodegradable antibiotic-cemented spacers and beads and further obtaining of intraoperative cultures. The final-staged reconstructive procedure was performed 5 days later with a medial column arthrodesis and osteotomy, allogenic bone grafting, plantar local advancement flap with NPWT (K–N), and skeletal fixation of the subtalar and ankle joints by using an off-loading and stabilization external fixation (O, P). The external fixation device was removed at approximately 7 weeks and the patient was transitioned to a non–weight bearing cast immobilization for approximately 6 weeks followed by appropriate surgical boot off-loading and accommodative orthotic devices. The patient required an additional incision and drainage procedure medially and eventually healed at his last 14-month follow-up (Q–U).
 |
The contraindications to lower extremity salvage with external fixation belong to two categories. The first has to do with the extent and location of infection. Superficial or localized osteomyelitis away from a load-bearing part of the lower extremity may be successfully treated with staged surgical debridement followed by delayed soft tissue coverage. The second consideration depends on the patient’s recuperative potential. Extremely debilitated patients or those with irreversible ischemia are poor candidates for lower extremity salvage with external fixation. The functional demands and expectations of the patient should be considered when determining if reconstruction will be beneficial over amputation.
Patients with chronic and long-standing comorbid conditions are considered high risk and may require a single, primary amputation. These high-risk patients may not tolerate the energy expenditure involved in multiple-staged procedures. A thorough review of the patient’s past medical history is vital in recognizing potential complications associated with the patient and planned reconstructive procedures. Diabetes mellitus with uncontrolled hyperglycemia, renal insufficiency, cardiovascular disease, peripheral vascular disease, severe infection with systemic manifestations, smoking history, poor nutrition, immunosuppression, and psychosocial difficulties, if not addressed appropriately, will compromise the ability to obtain favorable outcomes. The Cierny–Mader classification system may be useful in helping the surgeon to predict which patients are good candidates for lower extremity salvage with the use of external fixation. Similarly, those patients with significant comorbidities can be classified according to the Cierny–Mader scheme and may be better candidates for primary lower extremity amputation.
In addition, local factors may preclude the patient from undergoing lower extremity salvage. Chronic lymphedema, venous stasis dermatitis, and venous insufficiency are often not amenable to correction with external fixation. Furthermore, patients with critical lower extremity ischemia or life-threatening infections, such as gas gangrene and necrotizing fasciitis, may not be suitable for external fixation usage and may require immediate amputation.
Clinical Case III
Clinical (A, B) and radiographic anteroposterior (C) and lateral (D) views showing a severely infected Charcot neuroarthropathy right foot with a deep abscess. The patient presented with systemic signs of infection and had a history of open wounds to the right foot with associated trauma and poorly controlled diabetes mellitus. The patient underwent an initial multiple incision and drainage procedure, plantar cuboidectomy, and obtaining of deep intraoperative bone and soft tissue cultures and bone biopsy (E). Cultures were negative for osteomyelitis and the patient returned to the operating room 5 days after the first surgery for an entire resection of the navicular and medial cuneiform that were used as autografts after meticulous dissection of their cartilaginous articulations combined with multiple midtarsal arthrodesis and a plantar local advancement flap on the basis of the medial plantar artery (F–I). The entire medial column of the foot was fused with the use of a locking plate combined with an off-loading and stabilization external fixation system (J, K). At approximately 6 weeks later, the patient returned to the operating room for removal of the external fixator and cast application below the knee. The patient subsequently developed a deep abscess and severe infection 4 months after the external fixation removal. At that time, the internal fixation was removed and was followed by insertion of nonbiodegradable antibiotic-cemented beads at the medial (L) and plantar (M) aspects of the foot. An intraoperative negative pressure wound therapy device was also applied at the plantar wound (N) while the medial aspect of the foot was closed primarily (O). Please note the utilization of the off-loading and stabilization external fixation system for the right foot and ankle (P, Q). The external fixation device and retained antibiotic beads were removed at approximately 8 weeks and the patient was transitioned to a non–weight bearing cast immobilization for approximately 8 weeks followed by appropriate surgical boot off-loading and accommodative orthotic devices. The patient required an additional incision, drainage and closure procedure at the plantar aspect of the foot which eventually healed at his last 13-month follow-up (R–V).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








