Stepwise Approach to Charcot Midfoot Reconstruction and External Fixation
Paul S. Cooper
Crystal L. Ramanujam
Zacharia Facaros
Thomas Zgonis
Introduction
The management of Charcot neuroarthropathy (CN) midfoot deformities has evolved from a nonoperative approach using total contact casting and off-loading, to that of a surgical one. Challenges in reconstruction and especially in patients with diabetes mellitus include compliance, osteoporosis, diminished bone stock, severe deformities, and wound healing. External fixation as a treatment method can address most of these issues, and in many cases it is safer for the patient. In the presence of active wounds or associated osteomyelitis, it is the only viable option to consider.
The most common CN midfoot deformities occur at the tarsometatarsal, intercuneiform, or transverse tarsal joint level. As a rule, the more proximal the point of involvement, the greater instability and need for surgical stabilization. Charcot deformities at Lisfranc’s level are divided into two subcategories. The first involves a dorsal subluxation of the metatarsals in relation to the midtarsus. This may create a high-pressure point under the medial cuneiform leading to ulceration plantar-medially. Surgical correction involves an osteotomy through the deformity and translation plantarly to restore the medial longitudinal arch. The second is the classic rocker bottom deformity, which is a slow chronic deformity with extensive joint reorganization over time. Correction involves a biplanar wedge resection to correct both forefoot abduction and dorsal angulation.
Surgical techniques vary from acute correction with either internal, external, or combination fixation to gradual postoperative correction with external fixation. Factors to consider in choosing type of fixation and methods of correction include porosity of bone, rigidity of deformity, soft tissue stiffness, skin healing potential, and existence of superficial or deep infection. In general, the majority of CN midfoot deformities can be adequately addressed with an acute reduction of the deformity with definitive stabilization achieved (Table 16.1).
Preoperative Considerations
Due to CN being a bone destructive process, joint subluxation and deformity is clinically seen, leading to compromise of soft tissue integrity and often resulting in ulceration. For correction of the underlying deformity, which in turn provides long-term eradication of this type of ulceration, osseous reconstruction involving multiple joint arthrodesis is required. Both internal and external fixation are often utilized, yet the approach is case specific, depending on the apex of deformity and numerous patient variables, such as the patient’s age, weight, physical demands, and the presence of concomitant deformities. Proper assessment of underlying infection and instability of the midfoot are essential components in treating these conditions. Immediate surgical intervention is indicated when a limb-threatening infectious process requires decompression and stabilization.
The primary objective in the CN midfoot deformity is to establish a functional ambulatory lower extremity by restoring a stable, plantigrade foot without residual skin breakdown. In the presence of midfoot infection and/or osteomyelitis, staged surgical interventions may be necessary in order to eradicate the infection followed by the definitive reconstruction.
Extended medial column arthrodesis is a valuable option to establish a stable ambulatory foot, performed with internal fixation, external fixation, or a combination of both methods. Procedure selection is based on multiple factors including the osseous integrity, presence of bone loss, extent of fracture–dislocations, integrity of soft tissue envelope, history of deep infection, and the patient’s medical and ambulatory status. In some cases, the talocalcaneal and tibiotalar joints are frequently stabilized, maintaining foot and ankle neutral alignment while the midfoot arthrodesis site consolidates. This may be configured with internal Steinmann pin fixation or by way of the external fixator construct. The theory supporting this approach is that elimination of any frontal plane movement during the healing process inhibits disruption to the midfoot arthrodesis site.
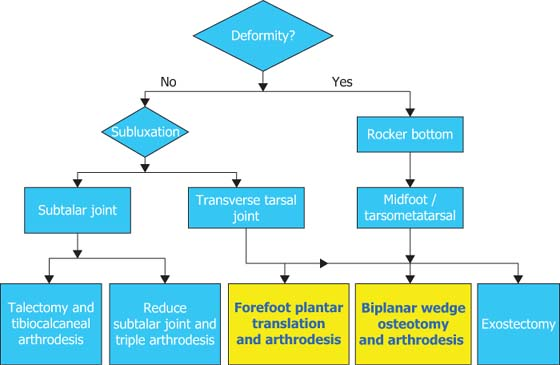
Table 16.1 Surgical Algorithm for Approaching a Charcot Midfoot Deformity | |
|---|---|
|
The Achilles tendon is characterized as a major deforming force in the diabetic patient, particularly among Charcot foot and ankle pathologies. The tendon is composed of the soleus and gastrocnemius muscles, the former originating on the posterior aspect of the tibia and fibula, while the latter originates on the posterior aspect of the distal femoral condyles. Both muscle bellies and supportive connective tissue combine to form the Achilles tendon, the insertion of which is into the posterior aspect of the calcaneus, functioning to plantarflex the ankle joint while supinating the subtalar joint during ambulation. The tendon externally rotates beginning approximately 12 cm proximal to the insertion, a critical component when performing an Achilles tendon lengthening procedure, a common step of the reconstructive process. Ankle joint dorsiflexion is needed for normal gait, roughly 10 degrees being the consensus value. Equinus is the limitation of this motion, occurring when the ankle joint is restricted. It may result from a tight joint capsule, scar tissue, or adhesions, or as in the case of the diabetic population, tendon thickening having evolved with increased density and structural disorganization. This disorganization has been linked to glycation-induced collagen cross-linking resulting in increased stiffness and a decrease in tensile strength and elasticity. These changes may ultimately lead to the equinus deformity and subsequently elevated peak plantar pressures, providing a significant alteration in contact forces promoting further instability. The majority of Charcot foot collapse is typically seen at the medial column and particularly at Lisfranc’s joint articulation. Biomechanical compensation may be seen within adjacent joints, causing further breakdown and collapse when the deformity is neglected.
Diabetic CN patients commonly present with undiagnosed peripheral vascular disease (PVD), and in many cases, a thorough workup by the foot and ankle specialist can determine the extent of the disease. When various risk factors are present in this patient population, including and not limited to, history of cigarette smoking, advanced age, impaired glucose tolerance, hyperlipidemia, and hypertension, patient counseling is required to discuss the potential perioperative risks and complications and any recommended alternatives to surgical intervention. Basic non-invasive testing and assessment for PVD includes obtaining an ankle-brachial index (ABI), toe-brachial index (TBI), segmental limb pressures, segmental volume plethysmography, or otherwise known as pulse-volume recording (PVR), and transcutaneous oxygen tension (TcPO2). A handheld Doppler probe is a convenient instrument for initial examination when pulses are not readily palpable. Otherwise, the tests mentioned are typically ordered through the vascular lab, followed by a formal vascular surgery consultation when indicated.
The clinical presentation of CN is typically categorized into acute or chronic phases. In the acute phase, proper assessment calls for recognition of soft tissue abnormalities and/or subtle structural compromise. The objective is to stabilize the lower extremity so as to ease the disease progression from the acute to the chronic phase. Further monitoring appreciates the presence of early fragmentation with fracture–dislocation in the acute episode, followed by eventual trabecular bridging, bony ankylosis, and sclerosis of the affected joints when transitioned to the chronic phase. Radiographic assessment and further medical imaging is paramount, providing visualization of bony deformities and prominences to determine the full extent of pathology. Careful clinical monitoring of patients is essential to optimize treatment for CN and improve the long-term outcome.
Detailed Surgical Technique
When needed, the tendo-Achilles lengthening (TAL) or gastrocnemius recession procedure is executed initially. One must decide which procedure is most appropriate and when
performing the TAL, an open versus percutaneous incision will dictate if the patient requires placement in prone position. Various gastrocnemius recession procedures are available and implemented accordingly. Osseous deformities may pertain to both the medial and lateral columns of the midfoot, with the medial aspect being more commonly affected. The pneumatic tourniquet is inflated prior to skin incision and is deflated before surgical wound closure and the application of the circular external fixator. Tourniquet use is contraindicated in those instances when local perfusion is significantly compromised or in patients with a recent history of major lower extremity revascularization.
performing the TAL, an open versus percutaneous incision will dictate if the patient requires placement in prone position. Various gastrocnemius recession procedures are available and implemented accordingly. Osseous deformities may pertain to both the medial and lateral columns of the midfoot, with the medial aspect being more commonly affected. The pneumatic tourniquet is inflated prior to skin incision and is deflated before surgical wound closure and the application of the circular external fixator. Tourniquet use is contraindicated in those instances when local perfusion is significantly compromised or in patients with a recent history of major lower extremity revascularization.
 Figure 16.1. Example of a Charcot neuroarthropathy midfoot rocker bottom deformity. Note the ankle equinus associated with the midfoot collapse (A, B). |
Charcot Midfoot Arthrodesis with Compression Through Olive Wire Docking
The deformity apex typically dictates a medial longitudinal exposure (Figure 16.1A and B). Alternatively, a bony wedge resection of the CN midfoot deformity may be addressed through a plantar ulcer if sufficient size and depth permits access. Any associated equinus deformity is first addressed and stabilized with a threaded Steinmann pin (Figure 16.2). If a medial longitudinal incision is made, a biplanar midfoot wedge resection is outlined by inserting two smooth 2 mm Kirschner (K) wires, placed at the apex of the deformity (Figure 16.3A and B). The biplanar wedge resection typically consists of an apex dorsally and laterally to perform a closing wedge resulting in plantarflexion and adduction reduction of the forefoot. Optimal reduction is confirmed when the two K-wires achieve parallelism following resection (Figure 16.4A and B). The osteotomy is then temporarily stabilized using a 2 mm threaded Steinmann pin across the midfoot directed distal-medial to proximal-lateral (Figure 16.5A and B).
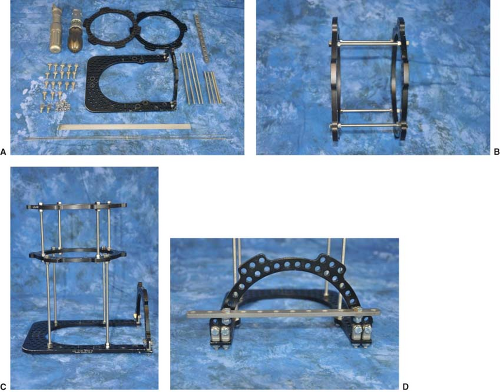
A standard static circular external fixator for CN midfoot arthrodesis involves a multiplane configuration with two distal tibial rings and a foot plate (Figure 16.6A). The prebuilt construct is placed over the foot and leg with folded sterile towels placed between the leg and the external fixator to maintain proper spacing and to assist in orientation. In addition, surgical towels are placed along the outside of the entire construct to prevent any rotation or angulation of the lower extremity. This external fixator consists of two segments: One segment incorporating the two full rings, which may be referred to as the tibial block, while the second segment consists of the foot plate (Figure 16.6B–D). For scenarios involving internal fixation, regardless of whether it is pins, screws, or a plate, this apparatus is primarily utilized for neutralization and stabilization but may also include compression augmentation when desired. Each respective segment is then connected to the underlying anatomy by way of smooth wires, olive wires, and/or half-pins. The ring and adjoined pin or wires may be thought of as a stable block, at which point the individual segments require fixation to one another for further adequate stability. Multiple threaded rods are utilized to achieve this. Once in position, multiple wires and/or half-pins are driven adjacent to both tibial rings and involve opposing wire placement in a similar fashion (Figure 16.7A–C).
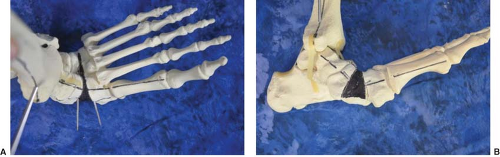 Figure 16.3. Example of two smooth K-wires to create a biplanar osseous wedge resection of the midfoot deformity (A). Note the segment to be resected in black outlined by the two smooth K-wires (B). |
 Figure 16.4. Example of the midfoot alignment after resection of the osseous segment resulting in parallel K-wires (A, B). |
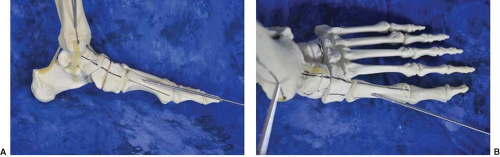 Figure 16.5. Example of the forefoot held in alignment with a threaded Steinmann pin fixation (A, B). |
Refer to Chapter 8 and Figures 8.1–8.5 for detailed description and visualization of the following six transosseous wires combined with half-pins when necessary. The first wires are initially driven from a lateral-to-medial direction and inferior to the respective tibial rings. The opposing wires are then driven from a medial-to-lateral direction and superior to the tibial rings. Four wires are used in total, placed in a bicortical fashion, driven with steady and even pressure and should not deviate from their intended course. The laterally inserted tibial wires are at 90 degrees to the longitudinal axis of the lower extremity while the medially placed wires are roughly 45 degrees to the same axis. The angles between the two should be as large as possible without compromising balance. Once again, half-pins may be interchanged accordingly, particularly implemented when the static circular external fixator requires placement for longer durations. A third transosseous wire may also be driven in place of a half-pin. Wire fixation bolts and nuts are configured to attach the wires to the rings, while neutral alignment of the foot and lower leg is maintained for desired postoperative healing. In the arrangement involving two transosseous wires for each ring, manual tightening with wrench instrumentation is done starting laterally and to the inferior fixation points on both rings, at which time tightening transpires medially and to the corresponding anterior fixation points. Tensioning with a dynamometric tensiometer is first to the medial wires connected along the posterior aspects in which further tightening is required to secure and lock the wires into position. Tensioning is then carried out laterally. The smooth wires placed in the tibia are typically tensioned between 110 and 130 kg of force, but at times, 90 to 110 kg of force will suffice in the diabetic population. Appropriate cutting and bending of the wires conclude this portion of the procedure at the tibial block fixation.
Regarding the foot plate, axial calcaneal olive wires are now incorporated, providing additional stabilization without translation. The first olive wire is driven from a lateral-to-medial
direction, placed firmly in the posterior-superior calcaneal process, making sure to engage both cortices. This ensures that the neurovascular bundle located on the medial aspect is avoided and uncompromised. As the olive wire approaches the skin, the drilling stops and a minimal percutaneous stab incision, followed by blunt soft tissue dissection by way of a curved hemostat is performed. This provides a clear, uninhibited entry point of the olive portion into the skin. The drilling then resumes until light resistance against the olive is felt and a mallet is now used to complete entrance of the wire, resulting in a parallel wire with olive abutment against the lateral calcaneal wall. A second olive wire is driven in an opposite direction, from medial to lateral, attempting to orient the wire away from the neurovascular bundle, thus, typically driven from a proximal-medial direction into the posterior-inferior aspect, exiting distal-laterally. Again, the driven wire is ceased before the olive portion reaches the skin, at which time a small percutaneous stab incision is placed followed by blunt dissection, and so forth. Two olive wires are now abutting the calcaneus for rotational and angular stability and avoidance of frontal plane translation. The wires are connected to the foot plate by way of posts, fixation bolts, and nuts. In the diabetic population, these wires are not usually tensioned but if one was to do so, typical force ranges from 70 to 90 kg of force.
direction, placed firmly in the posterior-superior calcaneal process, making sure to engage both cortices. This ensures that the neurovascular bundle located on the medial aspect is avoided and uncompromised. As the olive wire approaches the skin, the drilling stops and a minimal percutaneous stab incision, followed by blunt soft tissue dissection by way of a curved hemostat is performed. This provides a clear, uninhibited entry point of the olive portion into the skin. The drilling then resumes until light resistance against the olive is felt and a mallet is now used to complete entrance of the wire, resulting in a parallel wire with olive abutment against the lateral calcaneal wall. A second olive wire is driven in an opposite direction, from medial to lateral, attempting to orient the wire away from the neurovascular bundle, thus, typically driven from a proximal-medial direction into the posterior-inferior aspect, exiting distal-laterally. Again, the driven wire is ceased before the olive portion reaches the skin, at which time a small percutaneous stab incision is placed followed by blunt dissection, and so forth. Two olive wires are now abutting the calcaneus for rotational and angular stability and avoidance of frontal plane translation. The wires are connected to the foot plate by way of posts, fixation bolts, and nuts. In the diabetic population, these wires are not usually tensioned but if one was to do so, typical force ranges from 70 to 90 kg of force.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree