Stepwise Approach to Charcot Hindfoot/Ankle Reconstruction and External Fixation
Paul S. Cooper
Thomas Zgonis
Introduction
Charcot neuroarthropathy (CN) hindfoot/ankle deformities are the most unstable and therefore the most urgent of all Charcot locations in the lower extremity to be treated surgically. While cast immobilization is effective for various CN deformities in the midfoot, the inherent instability associated with CN destruction of the hindfoot/ankle joints leaves little time interval between the subfibular ulceration and the osteomyelitis with deep abscess formation.
A deep infection in association with an active Charcot process in the ankle joint frequently necessitates a lower-limb amputation. Charcot hindfoot/ankle deformities, unlike the foot counterparts, are inherently unstable resulting in collapse even while immobilized in a cast. Surgical intervention either with internal, external, or with combination fixation is imperative and sometimes urgent in these case scenarios. The goals of operative management of a CN hindfoot/ankle are the same as they were described with the CN midfoot including, but are not limited to restoring alignment, achieving stability for bracing, decompression of bony prominences, and prevention of skin breakdown in addition to shortening the course of CN process (Table 17.1).
Preoperative Considerations
Basic principle in surgical management of CN hindfoot/ankle deformity is to achieve a stable arthrodesis or, as an alternative, a stable painless pseudoarthrosis that allows for bracing. Joint reconstruction, total ankle arthroplasties, and limb lengthening should be avoided when planning for Charcot foot and ankle reconstruction. The technical challenges involved with CN reconstruction of the hindfoot/ankle include bone quality such as osteoporosis and various degrees of bone loss, patient noncompliance, and severe soft tissue compromise.
General principles in approaching the surgical correction of a CN deformity include full thickness incisions, spanning uninvolved joints to achieve adequate fixation for primary arthrodesis. Typically, there is a balance between the degree of skeletal shortening and the realignment. In addition to anatomic location, CN deformities are based on the Eichenholtz classification of radiographic findings. The stage 1, or dissolution phase, involves acute inflammation with erythema, warmth, swelling, and regional bone demineralization. There are also periarticular fragmentation and joint dislocations. Stage 2, the stage of coalescence, involves diminished inflammation and decreased fluctuation of swelling, absorption of bone debris, reorganization, and early healing of fragments or periosteal bone formation. Stage 3, the final stage of resolution, involves swelling being replaced by the final fixed deformity, normalization of skin temperatures, and enlargement of the foot and/or ankle. Radiographic findings include bony or fibrous ankylosis and smoothing of bone fragments.
The timing for surgical intervention is usually optimal in late stage 2 to stage 3; however, in Charcot involvement of the hindfoot/ankle joints, early intervention takes precedence over the stage. Typically, the patient will be in early stage 1 where advanced destruction and bone porosity makes traditional internal fixation difficult. External fixation with pin or wire stabilization confers an optimal method of stabilization in any Eichenholtz stage. In addition, due to the limited exposures required for stabilization compared to internal fixation with extended internal plating, soft tissue dissection is kept to a minimum. In most cases, external fixation adjustment can be performed postoperatively allowing for continued compression, and correction of residual deformity that could not be addressed at the time of the index procedure.
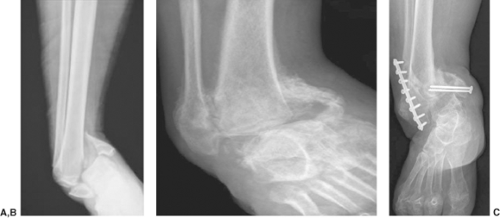
In general, there are three patterns involving the hindfoot/ankle in CN. The first, tibial involvement is generally felt to be more unstable, drifting into varus position and it is seen most often following an open reduction and internal fixation of the ankle (Figure 17.1A–C). The fibula by being prominent, combined with the instability of the ankle joint, creates a pressure ulceration under the fibula in a short period of time early in the Charcot development. The tibial Charcot pattern, however, is easier to salvage with either a tibiotalar or a tibiotalocalcaneal arthrodesis. The talar Charcot process while less common, tends
to be more stable, is seen more frequently in diabetics with end-stage renal disease and has a tendency to axially collapse or drift into valgus (Figure 17.2A and B). While not as quick to develop skin breakdown as the tibial variant, this pattern of involvement is more difficult to salvage due to the absence and resolution of the talus in most cases. Salvage consists of either a primary tibiocalcaneal or a pantalar arthrodesis. The rarest pattern, peritalar collapse, involves a Charcot process around the talus whereby the calcaneus and foot sublux and rotate off the talus laterally (Figure 17.3A–C). Due to the secondary soft tissue contractures and shortening, this pattern is the most difficult to reduce and requires frequently either a gradual reduction of the hindfoot and forefoot around the talus or salvage with a talectomy and resulting tibiocalcaneal arthrodesis.
to be more stable, is seen more frequently in diabetics with end-stage renal disease and has a tendency to axially collapse or drift into valgus (Figure 17.2A and B). While not as quick to develop skin breakdown as the tibial variant, this pattern of involvement is more difficult to salvage due to the absence and resolution of the talus in most cases. Salvage consists of either a primary tibiocalcaneal or a pantalar arthrodesis. The rarest pattern, peritalar collapse, involves a Charcot process around the talus whereby the calcaneus and foot sublux and rotate off the talus laterally (Figure 17.3A–C). Due to the secondary soft tissue contractures and shortening, this pattern is the most difficult to reduce and requires frequently either a gradual reduction of the hindfoot and forefoot around the talus or salvage with a talectomy and resulting tibiocalcaneal arthrodesis.
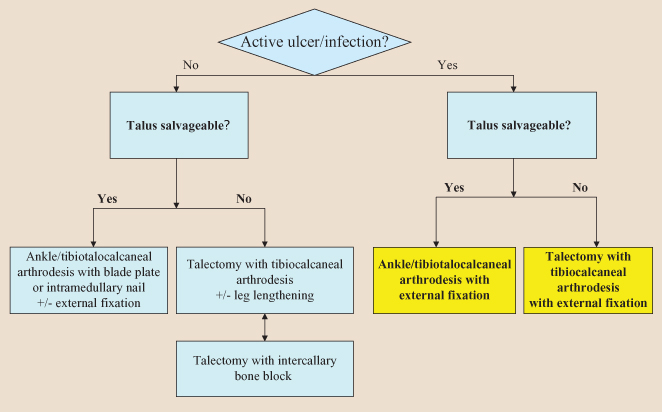
Table 17.1 Surgical Algorithm for Approaching a Charcot Hindfoot/Ankle Deformity | |
|---|---|
|
Due to the increased expenditure associated with below-the-knee amputation (BKA) in the diabetic patient, limb salvage with reconstructive hindfoot/ankle arthrodesis confers advantages over the BKA with regard to both energy expenditure and lifetime prosthetic costs. However, in cases where the host is severely compromised in combination with extensive bone loss, large open wounds, or osteomyelitis, limb salvage may not be preferable over BKA.
 Figure 17.2. Examples of Charcot neuroarthropathy talar variant (A, B). Note complete destruction of the talus with axial collapse. |
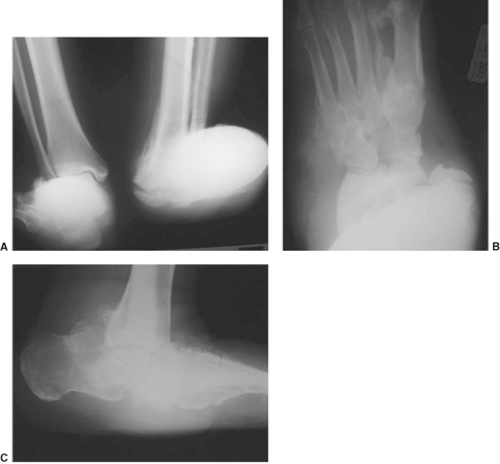 Figure 17.3. Examples of Charcot neuroarthropathy peritalar variant (A–C). Note complete lateralization of the foot from the intact talus. |
Detailed Surgical Technique
Charcot Ankle Arthrodesis
The deformity is primarily approached through a longitudinal incision over the distal third of the fibula (Figure 17.4A and B). The incision curves under the talus to extend into the subtalar joint. Following the subperiosteal dissection, the distal approximate 20% of the fibula is resected. This fibular bone should be avoided for use as autogenous grafting especially in infected and osteomyelitic cases. A second optional incision medially over the distal medial malleolus, 4 cm in length, may be used for recalcitrant or fixed varus deformities that cannot be corrected through the lateral approach alone. Transverse joint articular resections with either an osteotome or a sagittal saw perpendicular to the longitudinal axis of the tibia are made to both the tibial and talar articular surfaces, respectively (Figures 17.5A and B and 17.6A–C). The resected segments are then temporarily stabilized with the ankle aligned in neutral dorsiflexion/plantarflexion, approximate 5 to 10 degrees valgus and posterior translation of the talus on the tibia using a series of large threaded Steinmann pins (Figure 17.7A and B).
External fixation designs for the CN hindfoot/ankle deformity involve assessment of bone quantity, bone quality,
and residual deformity not corrected through the resection osteotomy on the tibia and talus. Circular external fixation is constructed with a standard tibial block of two rings connected by either threaded rods or alternatively threaded sockets (Figures 17.8 and 17.9). In addition, a standard foot plate (ring) construct is utilized consisting of an enclosed half ring at the distal end of the ring, stabilizing both the hindfoot and the forefoot. Options for connections between the tibial block and the foot ring consist of either threaded rods, telescoping rods,
or multiaxial struts depending on whether axial compression or angular deformities need to be corrected in the postoperative period. If active wounds are present and need access for dressing changes or additional surgery in the postoperative period, adjustable struts are preferred over rods due to ease of correction.
and residual deformity not corrected through the resection osteotomy on the tibia and talus. Circular external fixation is constructed with a standard tibial block of two rings connected by either threaded rods or alternatively threaded sockets (Figures 17.8 and 17.9). In addition, a standard foot plate (ring) construct is utilized consisting of an enclosed half ring at the distal end of the ring, stabilizing both the hindfoot and the forefoot. Options for connections between the tibial block and the foot ring consist of either threaded rods, telescoping rods,
or multiaxial struts depending on whether axial compression or angular deformities need to be corrected in the postoperative period. If active wounds are present and need access for dressing changes or additional surgery in the postoperative period, adjustable struts are preferred over rods due to ease of correction.
The circular external fixator once constructed is slid over the lower leg and lined up with the subtalar joint corresponding to the glabrous skin junction. As was previously described in Chapter 16, the tibial block and the foot ring are first secured by their respective anatomic transosseous wires (Figure 17.10). With these transosseous reference wires in place, residual translation medial to lateral can now be adjusted. The tibial block segment is definitively stabilized with either transosseous wires, half-pins, or a combination of each. Pin spread is critical especially with the use of half-pins. Multiple half-pins in a linear pattern will increase the risk for pathologic fracture following removal (Figure 17.11A–C).
Attention is then turned to both hindfoot and talar stabilization. Two to three transosseous wires are added in a divergent pattern through the calcaneus and tensioned or tightened appropriately (Figure 17.12). Without talar transosseous wires, the primary focus of compression is through the subtalar joint. Transverse tensioned wires inserted through the talus redistribute most of the compression applied to that across the tibiotalar joint (Figure 17.13A–C). These talar wires require posts connected to the wire fixation bolts on the foot plate for appropriate securing. Olive wires minimize the potential for subluxation of the talus while compression is applied following completion of the external fixation construct (Figure 17.14).
If additional fixation is needed into the forefoot, the wires/pins are directed into the metatarsals. Generally, two transosseous wires are recommended, one through the first and second metatarsals, the other through metatarsals three through five with each tensioned or tightened in a cross pattern onto the foot plate. Once stability on the foot plate is achieved, the threaded ankle transfixation Steinmann pins are removed, and any displacement at the arthrodesis site is noted (Figure 17.15A and B). Compression is then applied across the ankle joint and both visually and through C-arm fluoroscopic guidance the ankle joint is checked for any subluxation or change in alignment (Figure 17.16). Postoperative adjustments and instructions
on weight bearing status are case dependent according to the patient’s medical and ambulatory status, presence of wounds or infection, and social issues (Figure 17.17A–D and Clinical Cases I–III).
on weight bearing status are case dependent according to the patient’s medical and ambulatory status, presence of wounds or infection, and social issues (Figure 17.17A–D and Clinical Cases I–III).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree